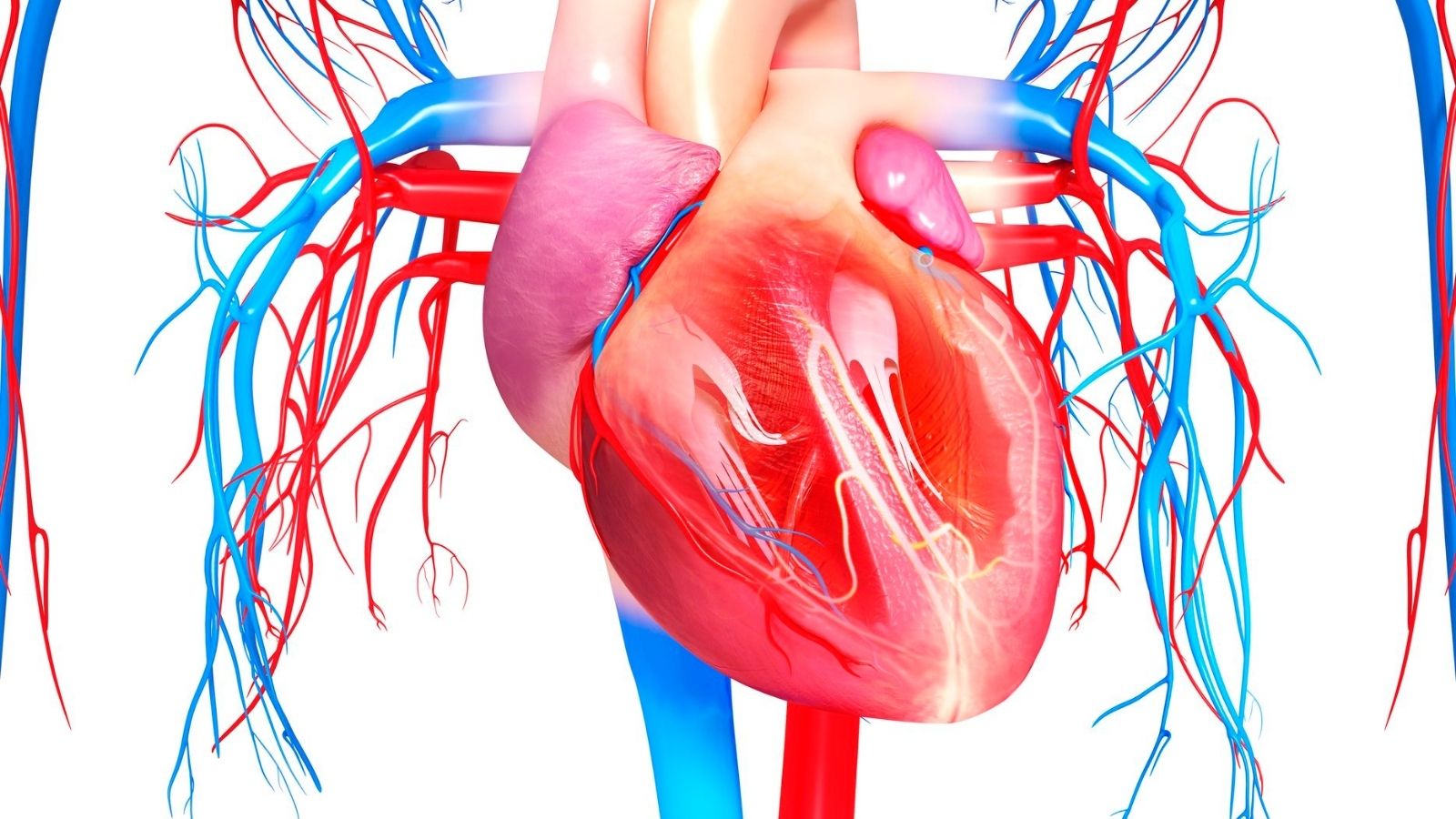
A vascular graft is an artificial or biological conduit used to replace or bypass diseased blood vessels. It restores circulation in cases of arterial obstruction, aneurysm, or vascular trauma.
Synthetic grafts, commonly made from materials such as Dacron or PTFE, are widely used in large vessel replacement. Biological grafts, derived from human or animal tissues, are preferred in specific cases to reduce thrombosis risk.
Complications of vascular grafts include infection, thrombosis, and graft failure, requiring close follow-up. Long-term outcomes depend on graft type, surgical technique, and patient-related factors.
Vascular grafts are vital in cardiovascular surgery, ensuring blood flow continuity and preventing limb loss or organ damage in critical circulatory disorders.
| Medical Name | Graft (Artificial Vein, Vascular Graft) |
| Frequent Use Areas | – Bypass surgeries (coronary artery, peripheral artery bypass)- Vascular repair after vascular occlusion or injury |
| Causes | – Restoring blood flow to a blocked or damaged vascular area |
| Risk Factors | – Vascular diseases- Diabetes- Smoking- Hypertension- Atherosclerosis |
| Complications | – Graft occlusion- Infection- Bleeding- Clot formation- Graft enlargement (aneurysm) |
| Diagnostic Methods | – Angiography – Doppler ultrasonography – CT or MR angiography |
| Treatment Methods | – Use of synthetic (artificial) or biological (autologous, allograft) vascular graft- Supportive treatment with anticoagulants and antiplatelet drugs- Regular follow-up |
| Prevention Methods | – Control of risk factors (blood pressure, sugar, cholesterol)- Regular vascular imaging and control- Healthy lifestyle |
What is an artificial vascular graft and what does it do?
As the name suggests, an artificial vascular graft is a specially designed, man-made vessel that is used when the body’s own vessel is unable to function. Imagine an old or damaged water pipe in your home that you need to replace with a new, sturdy pipe to ensure uninterrupted water flow. This is what an artificial vein graft does. When the arteries that carry blood throughout the body become blocked or damaged due to various diseases, these synthetic vessels are used to restore blood flow.
These grafts create a “bridge” or “side-path” for the blood to travel around the blocked or diseased area and reach its destination. Its main purpose is to allow blood to continue its journey through the body unhindered. This ensures that enough blood and oxygen reach vital organs and tissues, especially the heart, brain and legs. As a result, the patient’s symptoms are reduced and the overall quality of life is significantly improved.
These artificial veins should not be thought of as a simple plastic pipe. They are high-tech medical products developed to work in harmony with the body’s biological structure. They are made of biocompatible materials that will be easily accepted by the body and will not cause any harmful reactions. Over time, the body begins to cover the inner surface of this artificial vessel with a smooth layer of cells, just like our own natural vessels. This natural healing process is vital for the graft to function smoothly for many years.
In which cases is vascular grafting surgery mandatory?
Vascular grafting surgery is a life-saving intervention when blood flow is critically reduced and tissue health is compromised. There are major medical conditions that make this operation necessary.
We can list these situations as follows:
- Atherosclerosis (Arteriosclerosis)
- Aneurysms (Vascular Ballooning)
- Peripheral Arterial Disease (PAD)
- Coronary Artery Disease (CAD)
- Hemodialysis Need
- Traumatic Vascular Injuries
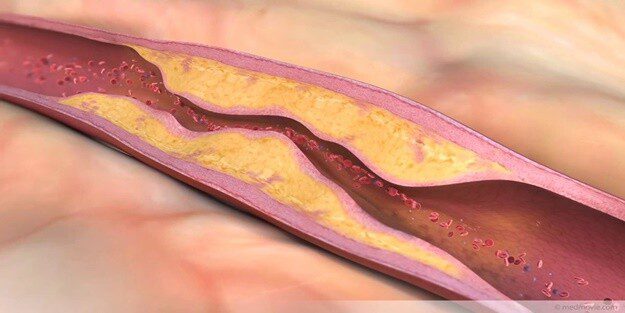
Arteriosclerosis, or atherosclerosis, is the most common reason for these operations. Fat and cholesterol plaques build up on the artery walls over time, narrowing and eventually blocking the arteries like a layer of lime. Peripheral arterial disease usually refers to these blockages in the arteries of the legs. Artificial vein surgery in a leg in this situation can eliminate severe pain when walking (claudication) and prevent the worst-case scenario of limb loss.
Aneurysms are when the vessel wall weakens and expands like a balloon. Especially when they occur in major vessels such as the aorta, they carry the risk of rupture, which can be fatal. A graft is used to support or completely replace this weakened area, avoiding this life-threatening risk. When the coronary arteries supplying the heart are blocked, coronary bypass surgery restores blood flow. Finally, for patients with kidney failure to undergo dialysis, a durable vascular access (graft) may need to be created to ensure adequate blood flow to the machine. Vascular grafting is often used as a permanent and effective solution when the disease has progressed and simpler methods such as medication or stents are inadequate.
How many types of vascular grafts are there on the market?
Vascular grafts are basically divided into two main groups according to their origin. This is the fundamental distinction that the surgeon considers when making the best decision for the patient’s condition.
These two main groups are:
- Biological Grafts
- Synthetic Grafts
Biological grafts, as the name suggests, are obtained from living tissues. The most ideal and considered to be the “gold standard” are vessels taken from the patient’s own body (autograft). The saphenous vein from the inside of the leg is usually used for this purpose. Because it is part of the body, it fits perfectly, has a very high long-term patency rate and has a natural resistance to infection. However, not every patient may have a vein of suitable quality or length. It may have been used in previous surgeries or may have deteriorated due to varicose veins. In this case, biological grafts from another human donor (allograft) or specially treated animal tissues (xenograft) may be an alternative.
Synthetic grafts are vessels produced in the laboratory from man-made polymers. The most well-known are Dacron and ePTFE (Teflon) materials. The biggest advantage of these grafts is that they are always ready for use in the desired diameter and length. They are especially indispensable in the repair of large diameter vessels such as the aorta or in cases where the patient’s own vessel is not suitable. Artificial vessel prices can vary depending on whether the graft is synthetic or biological, its brand and technological features. For example, more complex designs such as the Y graft, which is used at the point where the aorta splits into the legs and has a special shape, may be priced differently. The answer to the question of what is a Y graft is actually a synthetic vessel produced in the shape of the letter ‘Y’ in order to fully adapt to this bifurcation (bifurcation) area.
What materials are commonly used synthetic (artificial) vascular grafts made of?
There are two main “workhorse” materials that are prominent in the production of synthetic grafts used in vascular surgery today. These are polyester (commonly known by the trade name Dacron®) and expanded polytetrafluoroethylene (commonly referred to as ePTFE or Teflon®). These materials have been used safely in millions of patients for many years and have proven their effectiveness.
There are some basic properties that a material must have in order to be used as an artificial vessel. These characteristics determine how successful the graft will be inside the body.
The properties that an ideal graft material should have are as follows:
- Biocompatibility
- High Mechanical Strength
- Durability
- No Clot Formation (Thromboresistance)
- Porosity (Porosity)
Biocompatibility means that the material does not cause a foreign body reaction or allergy when it enters the body. Mechanical strength and durability are critical so that the graft can withstand the high blood pressure inside the artery for years and not degrade its structure. This is directly related to the lifespan of the artificial vessel. The non-clotting property prevents blood from sticking to the inner surface of the graft and clotting (thrombosis), which is one of the most important factors for the graft to remain open. Finally, porosity means that the material has microscopic pores. These pores allow the body’s own cells to attach to the wall of the graft and “internalize” it, which allows the graft to integrate with the body. The surgeon’s choice of material is the art of finding the balance between these properties that best suits the patient’s needs.
What are the main features and differences between Dacron and ePTFE grafts?
Although Dacron and ePTFE are both successful synthetic grafts, they show some fundamental differences in terms of their structure and usage areas. The surgeon prefers one of these two materials according to the area to be operated on and the characteristics of the vessel.
Dacron (Polyester): This material has a woven or knitted fabric structure. Woven ones have a tighter structure and leak less blood. Braided ones are more flexible and their porous structure allows them to grow into the body tissue better. As it is a very durable material, it is usually the first choice for repairing large diameter vessels exposed to high pressure, such as the aorta.
ePTFE (Teflon): The inner surface of this material is much smoother than Dacron. This smoothness and the material’s natural negative electrical charge make it difficult for blood cells and clotting factors to adhere to the surface. Therefore, the risk of clotting is lower. Thanks to this superior feature, it is frequently used in bypass surgeries (artificial vein surgery in the leg), especially in the legs where blood flow is slower, and in vascular access routes created for dialysis patients.
A common disadvantage of both materials is that they are considerably stiffer than natural vessels. The junction (anastomosis) where a flexible natural vessel is sewn to a rigid synthetic graft experiences a kind of “mismatch”. Over time, this mechanical stress can lead to thickening of the vessel wall (intimal hyperplasia) and new narrowings at these junctions. This is one of the biggest challenges of current synthetic graft technology.
Which artificial vascular graft performs better in the long term?
This is a question on which there is no consensus even among surgeons. Because the long-term success of a graft depends not only on its material, but also on where it is placed, the diameter of the vessel, the blood flow rate and the general health status of the patient. There is no “one truth” on this issue.
Scientific studies confirm this, sometimes with contradictory results. For example, some large studies examining leg artery bypasses have found that Dacron grafts have slightly better long-term patency rates than ePTFE. However, other studies report no significant difference between the two materials. Similarly, it has been observed that both materials have similar success rates in aortic surgeries.
These data show us this: there is no universal concept of the “best” graft; there is the “most appropriate” graft for the patient. The surgeon makes this decision by combining the patient’s anatomical structure, vessel quality, clotting risk and his/her own experience. Today, more advanced versions are also available, in which the surfaces are coated with substances such as heparin, which prevents clotting, to improve the performance of both materials. These technological improvements make the long-term results of the grafts even better.
How is a vein grafting surgery performed in practice?
Vascular grafting surgery is a serious surgical procedure performed under general anesthesia (i.e. while you are completely asleep) in the operating room of a full-fledged hospital. Although the basic steps of the surgery vary slightly depending on the area to be bypassed, they generally follow a similar logic.
In general terms, the process consists of the following steps:
Making an Incision The surgeon makes an incision on the skin to reach the diseased vessel. The location of this incision depends on the purpose of the surgery. For example, the sternum is opened for a heart bypass, the groin and/or knee for a leg bypass, and the abdomen for an aortic aneurysm.
Controlling the vessel: Once the target vessel has been found, the blood flow is temporarily controlled with special instruments (clamps).
Graft Placement: This is the most delicate and important part of the procedure. The surgeon meticulously sutures one end of the selected artificial vascular graft to the intact vessel above the blockage and the other end to the intact vessel below the blockage with very fine stitches. This creates a new “highway” through which blood can flow bypassing the blockage.
Control and Closure: After the graft is sutured, the clamps are opened and it is checked whether the blood flows through the new pathway and whether there is leakage in the suture lines. If everything is in order, the layers of tissue and skin are closed in accordance with the anatomical sequence and the operation is terminated.
What are the risks and benefits of artificial vein surgery?
Like any major surgical procedure, vascular grafting surgery has significant benefits as well as potential risks. It is very important to understand both sides in a balanced way in the decision-making process.
The biggest benefit of the surgery is that it saves lives and limbs by restoring blood flow and dramatically improves quality of life by eliminating complaints such as pain. The most important benefit of this surgery is that it prevents catastrophic events such as heart attack, stroke, ruptured aneurysm or loss of a leg.
On the other side of the coin, however, there are risks associated with artificial vascular surgery.
The risks of general surgery include:
- Anesthesia-related reactions
- Bleeding
- Infection
- Clot formation in the lung (pulmonary embolism)
- Temporary impairment of kidney function
There are also graft-related risks specific to this surgery. The answer to the question “Will the artificial vein be blocked?”, which patients are most curious about, is at the top of these risks.
Major graft-specific complications:
Thrombosis (Blockage by Clot): It is the formation of a blood clot inside the graft and blockage of the vessel. This is the most common cause of graft failure. Blood thinners used after surgery are given to reduce this risk.
Anastomotic Stenosis (Intimal Hyperplasia): It is the formation of a new stenosis over time, usually at the connection points where the graft is sutured to the natural vessel, as a result of the body’s overreaction to healing.
Graft Infection Synthetic materials are more prone to infection than the body’s natural tissues. Graft infection is a serious condition that is very difficult to treat and often requires removal of the graft.
Structural Deterioration of the Graft: Very rarely, fatigue and enlargement of the graft material may occur over the years.
Although the presence of these risks may seem frightening, these risks are minimized with today’s surgical techniques and postoperative follow-up protocols.
What is the recovery process after artificial vein surgery?
The period after artificial vein surgery is a step-by-step healing process that requires patience and care. Full recovery usually takes 6 to 12 weeks.
During the first few days in hospital, you will be closely monitored. You will usually stay in the intensive care unit for one or two days after the operation. Your pain will be controlled with medication and the aim is to get you up and walking as soon as possible to prevent complications such as clots.
The first 4-6 weeks after returning home is the most critical period of recovery.
There are some important points you should pay attention to during this period:
Rules to follow when it comes to physical activity:
- Avoiding pushing, pulling and heavy lifting (usually more than 5 kilos)
- Taking short, slow-paced walks on a daily basis
- Not driving for at least 4-6 weeks
- Climbing stairs slowly and resting
Basic principles for wound care:
- Keeping incision sites clean and dry
- Avoiding the bath or pool until your doctor gives permission
- Not applying lotion or cream to incision sites
- Tell your doctor immediately if you notice redness, discharge or excessive swelling
What you need to do in your diet:
- Reducing salt consumption
- Avoid saturated and trans fats
- Consuming high-fiber foods (vegetables, fruits, whole grains)
- Drink plenty of water
A very important thing to remember is emotional healing. Having a major surgery is as exhausting for the soul as it is for the body. It is perfectly normal to feel more emotional, anxious or depressed than usual after surgery. This is part of the healing process. However, if this lasts for a long time, you should not hesitate to seek professional support. The most important thing is to know that the surgery does not “cure” the underlying vascular disease, it only solves a problem. To maintain the health of your graft and all other vessels, quitting smoking, eating a healthy diet, exercising regularly and taking the prescribed medications (blood thinners, cholesterol medications, etc.) regularly for life are the keys to prolonging the life of the artificial vessel and a healthy future.
Veins of the future What does tissue engineered grafts (TEVG) mean?
Tissue engineered vascular grafts (TEVGs) are an exciting innovation that has the potential to revolutionize vascular surgery. The basic philosophy of this approach is to use the body’s ability to heal and regenerate itself to build a completely new and living vessel, rather than inserting a permanent artificial part into the body.
The principle of this technology is as follows: A scaffold (graft) made of a special biodegradable polymer, which dissolves and disappears in the body over time, is inserted in place of the diseased vessel. At first, this scaffold acts as a temporary channel for the blood to flow through. Over a period of months, the body’s own cells migrate into the scaffold, multiply there and produce natural vascular components such as collagen to form a brand new tissue (neovasculature). When this process is complete, the initial artificial scaffold has completely dissolved, leaving behind a living, growing and self-repairing natural vessel composed only of the patient’s own cells. This is a shift from a paradigm of “replacement” to a paradigm of “renewal”.
What advantages do biodegradable grafts promise for the future?
The great promise of these smart grafts, which can dissolve in the body, is that they eliminate the long-term problems of a permanent implant. The fact that they disappear completely after acting as temporary scaffolding brings many important advantages.
These are the main advantages that the grafts of the future can offer:
- Prevention of Persistent Foreign Body Reaction
- Reduced Risk of Chronic Inflammation
- Elimination of Late Coagulation Problems
- Higher Resistance to Infection
- Growth Potential
- Perfect Mechanical Fit
One of the most groundbreaking advantages is the growth potential. Because the end product is the patient’s own living tissue, the vessel can grow with the patient. This is literally revolutionary, especially for children with congenital heart disease who have to undergo repeated surgeries as they grow up. And because these next-generation materials are designed to mimic the elasticity of natural arteries, the problem of “stiff tubing” in existing synthetic grafts and the resulting junction problems could be a thing of the past.
What are the latest and exciting developments in artificial vascular technology today?
The field of vascular grafting is advancing at a dizzying pace on multiple fronts. Today, there are many promising technologies under research and development or in limited clinical use.
Some of the most recent developments in this field include:
- Acellular Tissue Engineered Vessels (ATEVs)
- Advanced Biomimicry (Imitating Nature)
- 3D Bioprinting Technologies
- Minimally Invasive and Robotic Surgery Applications
- Artificial Intelligence Assisted Graft Design
ATEVs are bioengineered “off the shelf” biological grafts that have been stripped of all donor cells, leaving only a natural protein scaffold. They are not rejected by the body and have been shown to be much more resistant to infection than synthetic grafts. 3D printing technology allows for the production of “personalized” grafts that exactly match complex anatomies, based on the patient’s own tomography images. Artificial intelligence algorithms have begun to analyze these images to help surgeons design the optimal graft size, shape and material for a patient.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.