Cholesterol plays a key role in cardiovascular health, with elevated low-density lipoprotein (LDL) being a major contributor to atherosclerosis. Excess cholesterol deposits in arterial walls, narrowing vessels and increasing the risk of heart attack and stroke.
High-density lipoprotein (HDL) has protective effects by removing excess cholesterol from circulation and transporting it to the liver for excretion. Maintaining a healthy balance between LDL and HDL is crucial for optimal heart health.
Risk factors such as poor diet, obesity, sedentary lifestyle, and genetic predisposition contribute to high cholesterol levels. Preventive measures include a heart-healthy diet, regular physical activity, and smoking cessation.
Pharmacological treatments, particularly statins, are highly effective in lowering LDL cholesterol. Regular monitoring and adherence to prescribed therapy significantly reduce cardiovascular morbidity and mortality.
What Is Cholesterol and Why Is It Essential for Our Body?
Cholesterol is a waxy, fat-like substance that is used in the production of many important molecules, from hormones to vitamin D, which is the building block of our cells.
Contrary to popular belief, cholesterol is not intrinsically bad. Our bodies need it to function in a healthy way. Your liver already produces most of the cholesterol your body needs. The rest we get through food.
Some of the basic and vital functions of cholesterol in our body are as follows:
- Being the basic building block of cell membranes
- Helping the body produce vitamin D
- Producing sex hormones such as testosterone and estrogen
- Making hormones such as cortisol secreted by the adrenal glands
- Producing bile acids that aid in the digestion of fats
As you can see, it is impossible to live a healthy life without cholesterol. The problem starts not with cholesterol itself, but with the amount and the balance of its types in our blood. Animal foods in particular (meat, dairy products, egg yolks) contain cholesterol. Eating foods high in saturated fats can also cause your liver to produce more cholesterol, which can raise blood levels.
Good Cholesterol, Bad Cholesterol… What Do These Different Types of Cholesterol Mean?
Cholesterol cannot circulate in the blood on its own; it is transported in packages called lipoproteins. LDL (“bad” cholesterol) clogs blood vessels, while HDL (“good” cholesterol) helps to clean them. The balance of the two is the key to your heart health.
Because cholesterol and other fats are insoluble in water, they cannot move freely in the liquid part of the blood. Our body solves this problem by coating the fats with proteins, forming carriers called lipoproteins. The main types we need to know in terms of heart health are the following:
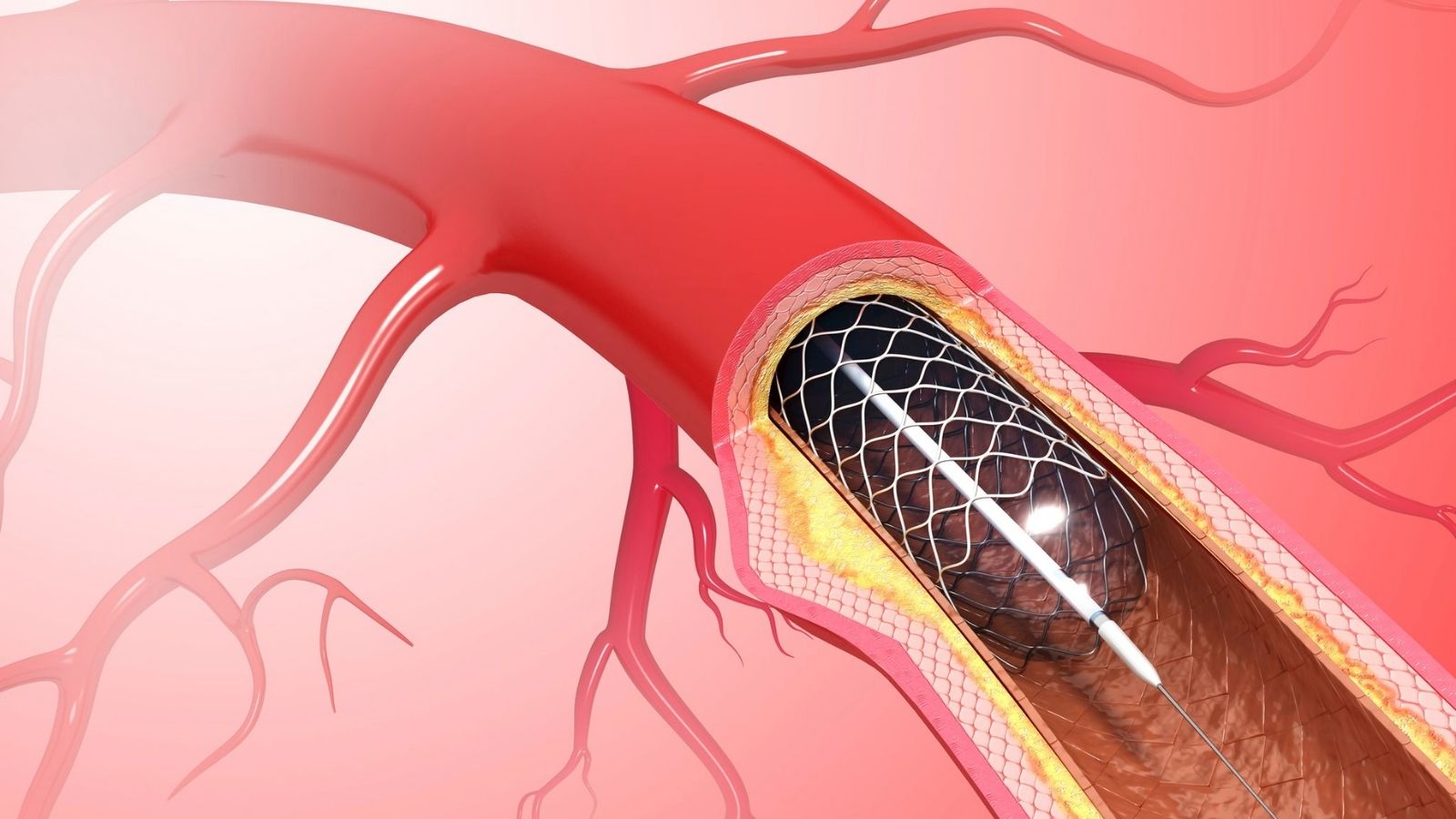
LDL (Low Density Lipoprotein): This is called “bad” cholesterol for a reason. Its job is to take cholesterol from the liver and carry it to the cells. But if you have more LDL in your blood than you need, this excess cholesterol starts to stick to the walls of your arteries. Over time, it builds up and forms hard layers called “plaques”. These plaques narrow and harden your arteries like the calcification of a water pipe. We call this atherosclerosis and it is the main cause of heart attack and stroke. The general rule for LDL is simple: the lower the better.
HDL (High Density Lipoprotein): This is also called “good” cholesterol because it does the opposite. HDL works like a kind of garbage collector. It collects excess cholesterol that accumulates in the blood vessels and cells and takes it back to the liver for disposal. High HDL levels therefore help keep your arteries clean and reduce your risk of heart disease.
Triglycerides: A type of blood fat that is different from cholesterol. It is the body’s way of storing calories (especially from sugar and fats) that we eat but don’t immediately use as energy. High triglyceride levels are also an important risk factor for atherosclerosis, especially if you have low HDL or high LDL.
Total Cholesterol: This is a number that shows the total amount of all types of cholesterol in your blood. It gives you an idea on its own, but what really matters is the ratio of your LDL, HDL and triglyceride numbers. Your doctor looks at all of these values together when assessing your risk of heart disease.
What Do the Cholesterol Values in My Blood Test Mean and What Should Healthy Levels Be?
Ideal cholesterol levels are individualized and depend on your risk factors. However, as a general guideline, total cholesterol should be below 200 and LDL below 100. HDL should be above 40 in men and above 50 in women.
When interpreting your blood test (lipid panel) results, remember that these figures should be considered in conjunction with your general health, age, family history and other conditions such as diabetes or high blood pressure. You should therefore discuss the results with your doctor.
The table below is a general guide (values in mg/dL):
| Cholesterol Type | Healthy (Desirable) | High at the Border | High |
| Total Cholesterol | under 200 | 200-239 | 240 and above |
| LDL (“Bad”) Cholesterol | below 100 (Optimal) | 130-159 | 160 and above |
| HDL (“Good”) Cholesterol | 60 and above (Protective) | Male: 40-59,
Woman: 50-59 |
Male: 40 under,
Female below 50 (Low) |
| Triglycerides | under 150 | 150-199 | 200 and above |
One point to pay particular attention to: If you have had a heart attack, have diabetes or have multiple risk factors, your doctor may want to lower your LDL (“bad”) cholesterol target to below 70 mg/dL, and in some cases even below 55 mg/dL. This means that treatment must be completely individualized.
What Causes High Cholesterol in My Veins?
High LDL (“bad”) cholesterol gradually builds up on the inner walls of your arteries, forming a fatty, hard layer called “plaque”. Over time, these plaques narrow the blood vessels, making them less flexible and impairing blood flow and the nutrition of organs.
We can liken this process to how the clean water pipes in your home become calcified and clogged over time.
The Beginning of Deposition When too much LDL cholesterol circulates in your blood, these tiny fat particles leak into the delicate layer lining the inside of your arteries (the endothelium) and begin to build up there.
Plaque Formation: The body’s immune system recognizes this buildup as a threat and tries to intervene. However, this process worsens the situation, causing cholesterol, calcium and other cellular waste to accumulate and form plaque.
Narrowing of the Veins As the plaque grows, it narrows the space inside the vessel. This means that blood cannot flow as freely as before. For example, when the blood vessels that supply your heart narrow, you may feel chest pain (angina) during exertion.
The Most Dangerous Moment: Plaque Rupture: The most frightening aspect of atherosclerosis is that these plaques can suddenly crack or rupture. The body recognizes this as a wound and activates the clotting mechanism. A blood clot quickly forms on the ruptured plaque. This clot can completely block the already narrowed vessel. If this happens in the heart, it can cause a heart attack; if it happens in the brain, it can cause a stroke.
Which Serious Cardiovascular Diseases Does High Cholesterol Put You at Risk?
High cholesterol leads to arteriosclerosis (atherosclerosis), laying the foundation for many potentially fatal diseases such as heart attack, stroke, peripheral arterial disease (blocked leg arteries) and aneurysms.
Vascular damage caused by high cholesterol can affect different parts of the body, causing various diseases. The main ones are:
Coronary Artery Disease: Narrowing or blockage of the arteries that supply the heart (coronary arteries). It occurs when there is not enough blood supply to the heart muscle.
Heart Attack (Myocardial Infarction): It is a sudden blockage of one of the coronary arteries that permanently damages part of the heart muscle.
Stroke (Paralysis): Damage to brain tissue caused by blockage or bleeding in the blood vessels supplying blood to the brain. Most occlusive strokes develop against a background of cholesterol plaques.
Peripheral Arterial Disease: Narrowing of the arteries that usually supply the legs. The most typical symptom is pain in the legs (claudication) that occurs when walking and goes away at rest.
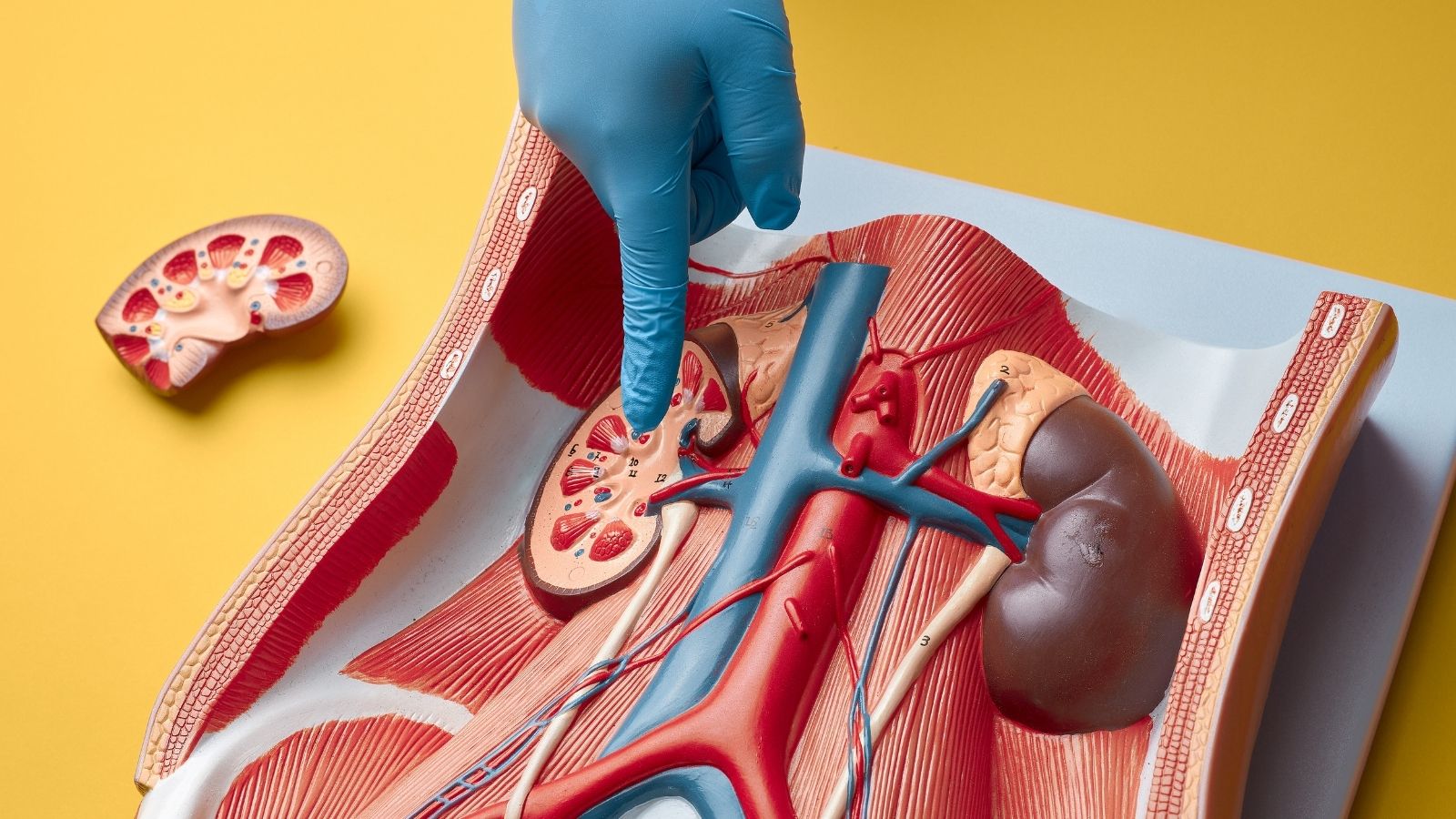
Aneurysm: It is a weakening and ballooning of the vessel wall. It is especially common in the aorta, the main artery in the abdomen, and its rupture can lead to fatal internal bleeding.
Chronic Kidney Disease: Over time, narrowing of the blood vessels that supply the kidneys can lead to impaired kidney function.
Which Risk Factors Play a Role in the Development of High Cholesterol?
Factors that increase the risk of high cholesterol include lifestyle habits we can change, such as diet, inactivity and smoking, as well as factors we cannot control, such as age, gender and genetic inheritance.
The factors that influence your cholesterol levels can be divided into two main groups.
Risk Factors that you can change (Controllable) are:
- Unhealthy diet (diet rich in saturated and trans fats)
- Lack of physical activity (sedentary lifestyle)
- Overweight or obesity
- Smoking
- Excessive alcohol consumption
Risk Factors that you cannot change (cannot be controlled) are as follows:
Age: Cholesterol levels naturally tend to rise with age.
Gender: In men, the risk usually increases at a younger age, while in women the risk increases markedly after menopause.
Family History (Genetics): If you have a family history of early heart disease or high cholesterol, your risk increases.
Having more than one risk factor multiplies the risk. For example, a person who both smokes and is overweight has a much higher risk of heart disease than someone with only one risk factor.
What Could Be the Impact of My Genetic Heritage on High Cholesterol?
Some people, especially those with an inherited condition called “Familial Hypercholesterolemia”, can have very high cholesterol levels genetically, no matter how healthy they live. This significantly increases the risk of heart disease at a very early age.
If your cholesterol is still too high despite eating a healthy diet and exercising regularly, it may be due to your genes. One of the most well-known genetic conditions is Familial Hypercholesterolemia (FH). This is when the mechanism that allows the body to remove LDL (“bad”) cholesterol from the blood does not work properly due to a genetic defect.
The main features of FH are:
- Very high LDL cholesterol levels from birth
- Significantly increased risk of having a heart attack at an early age (before the age of 55 in men and 60 in women) if left untreated
- Sometimes yellowish cholesterol deposits on the skin or eyelids (xanthoma and xanthelasma)
- Lifestyle changes alone are not sufficient and often require medication at an early age
If you have a family history of heart attack or stroke at an early age or have a known history of high cholesterol, you may also have a genetic predisposition. In this case, cholesterol screening from childhood and consultation with a specialist is of great importance.
How Can I Change My Lifestyle for High Cholesterol?
The most powerful way to get your cholesterol under control is to adopt lifestyle habits such as a heart-healthy diet, regular exercise, maintaining an ideal weight, quitting smoking and managing stress.
Even if medication is required, lifestyle changes are the cornerstone of treatment and increase the effectiveness of medication. Here are the steps you can take:
Changes you can make to your diet:
Reduce Saturated and Trans Fats:
- Processed meats (salami, sausage, pepperoni)
- Fatty red meats
- Full-fat dairy products (butter, cheese, cream)
- Packaged snacks and fries
Add to Your Table:
Soluble Fiber: Oats, barley, apples, oranges, carrots, dried beans, chickpeas, lentils.
Healthy Fats: Olive oil, avocado, walnuts, almonds, hazelnuts.
Omega-3: Fatty fish such as salmon, mackerel, sardines, flaxseed.
Lots of vegetables and fruit: It should make up half of your plate at each meal.
Other Important Habits:
Get Moving: Aim for moderate-intensity exercise such as brisk walking, swimming or cycling for 30 minutes at least 5 days a week.
Lose Weight: Losing excess weight, even a 5-10% weight loss, can make a significant improvement in your cholesterol levels.
Quit Smoking Quitting smoking is the best thing you can do for your heart health. Within a year of quitting, your risk of heart disease is halved.
Manage Stress: Try to remove stress from your life through yoga, meditation, deep breathing exercises or a hobby you enjoy.
What medicines are used for high cholesterol if lifestyle changes are not enough?
When cholesterol targets cannot be achieved despite lifestyle changes or when the individual’s risk is too high, various cholesterol-lowering drugs, especially “statins”, form the basis of treatment.
Medication is a proven method of reducing the risk of heart attack and stroke, especially by lowering LDL cholesterol. Your doctor will determine the most appropriate medication and dose based on your risk profile. The main groups of medicines are:
Statins The backbone of cholesterol treatment. They work by reducing the liver’s production of cholesterol. They are very effective in lowering LDL.
Ezetimibe: A drug that blocks the absorption of cholesterol from the intestines. It is usually preferred in addition to statins or in patients who cannot use statins.
PCSK9 Inhibitors: These are very powerful new generation drugs administered by injection. They are usually used in very high-risk patients with genetic high cholesterol or who have not responded to other treatments.
Fibrates: They are mainly used to lower triglyceride levels and slightly increase the good cholesterol HDL.
Remember, even if you start taking medication, maintaining healthy lifestyle habits is critical to the success of treatment.
When Should I Consult a Cardiovascular Surgeon for Cholesterol Management?
If you are in a high-risk group, if you have a family history of early heart disease, if your cholesterol is not reaching the target despite standard treatments, or if you have started to experience symptoms (such as chest pain, leg pain) due to vascular blockage, it may be vital to consult a Cardiovascular Surgery Specialist.
In most cases, cholesterol management can be successfully managed by your family doctor or a cardiologist. However, in some cases, the expertise of a Cardiovascular Surgeon is needed.
These are the situations in which you should consider contacting a specialist:
- You have a serious genetic condition such as Familial Hypercholesterolemia
- Failure to control your cholesterol levels despite treatments
- Atherosclerosis is advanced and begins to show symptoms
- Coronary angiography or other imaging methods show severe stenosis in the vessels
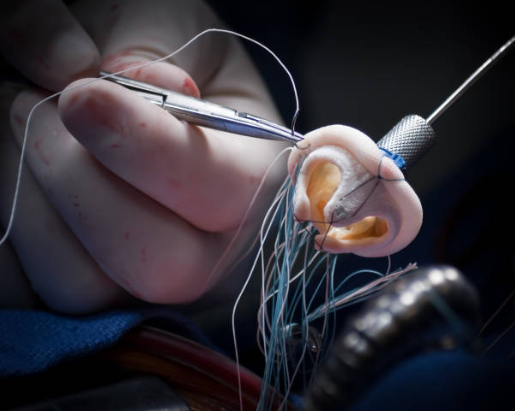
- When surgical or interventional treatment options such as bypass surgery, stenting, aneurysm repair should be considered.
A Cardiovascular Surgeon not only prescribes medication, but also assesses the structural damage to your blood vessels caused by high cholesterol and offers the most advanced treatment modalities to repair this damage. Remember, cholesterol management is a team game and you are the most important player on that team. Being informed about your health, having regular check-ups and getting support from a specialist when needed is the key to a long and healthy life.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.