Heart valve replacement is performed when severe valve damage prevents normal blood flow. The procedure involves removing the diseased valve and replacing it with either a mechanical or biological prosthetic valve.
Mechanical valves are highly durable but require lifelong anticoagulant therapy to prevent clotting. Biological valves, often derived from animal tissue, have shorter durability but do not require long-term blood-thinning medication.
The surgery is conducted under general anesthesia with cardiopulmonary bypass support. The diseased valve is excised, and the new valve is carefully positioned to restore efficient cardiac function.
Recovery involves intensive monitoring followed by gradual rehabilitation. Long-term management includes medication adherence, echocardiographic follow-up, and lifestyle adjustments to optimize heart function and valve performance.

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What are the Main Problems Requiring Heart Valve Replacement Surgery?
To understand the decision for heart valve replacement surgery, let’s take a brief look at how our heart works. You can think of our heart as a house with four rooms. Between these rooms there are doors that keep the blood flowing in the right direction, that is, always forward and prevent it from escaping backwards. We call these doors “heart valves”. We have four valves: tricuspid, pulmonary, mitral and aortic. With each heartbeat, these valves open and close in perfect harmony, ensuring healthy blood circulation.
But sometimes these doors can fail for various reasons. This is not a chemical problem that a drug can solve, but a mechanical, i.e. structural failure, such as a broken door hinge. This failure usually takes two basic forms.
The first is stenosis, or stenosis. In this case, the valves harden and calcify over time and become unable to open, like a rusted door. The heart has to work much harder than normal to get the blood through this narrow opening and over time it gets tired.
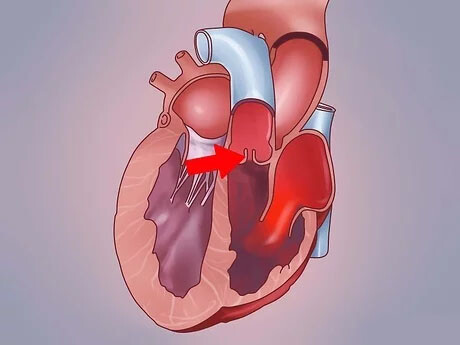
The second is regurgitation, or regurgitation or “leakage” as it is colloquially called. Here the valves cannot close, they remain ajar. Therefore, some of the blood pumped forward leaks backwards into the chamber from which it came. This causes the heart to pump the same blood over and over again, i.e. to row in vain, significantly increasing its workload.
There are many underlying causes of these valve diseases. Some causes are congenital structural differences. Other common causes are:
- Calcification due to aging
- Rheumatic fever caused by untreated throat infections at a young age
- Infections affecting the heart (endocarditis)
Whatever the cause, these diseases are usually progressive. In other words, they get worse over time and without intervention can lead to permanent heart damage and heart failure.
What Symptoms Signal the Need for an Upcoming Heart Valve Replacement Surgery?
When your heart valve fails to function properly and your heart starts to struggle to meet the body’s needs, your body starts to send you signals. It is very important to recognize these signals in time to take precautions before permanent damage occurs. The main symptoms that indicate a problem that may require heart valve replacement surgery and that you should consult a specialist are as follows:
- Shortness of breath
- Unusual fatigue
- Discomfort or pain in the chest
- Dizziness
- Fainting (syncope)
- Palpitations
- Swelling in the ankles, legs or abdomen (edema)
Among these symptoms, shortness of breath can occur especially when climbing stairs, walking uphill or sometimes even just lying down. Fatigue is a constant state of exhaustion that does not go away with rest, as opposed to saying “I am a bit tired today”. Discomfort in the chest can be a feeling of pressure, as if a weight is sitting on you. Any of these symptoms should be taken seriously, especially if they have occurred recently or are getting worse. Because these signals indicate that your heart is now asking for “help”.
Which Diagnostic Methods Are Used to Decide on Heart Valve Replacement Surgery?
In order to create a proper treatment plan, we first need to clearly see what the problem is, where it is located and how serious it is. For this reason, a comprehensive diagnostic process is carried out before heart valve replacement surgery. The steps we usually take in this process are the following:
First, we listen carefully to the patient’s medical history and complaints. In the physical examination that follows, an abnormal sound we hear while listening to the heart with a stethoscope, which we call a “murmur”, may give the first clue to valve disease.
However, our most important tool for definitive diagnosis and to determine the severity of the disease is the Echocardiography (ECHO) test. This test uses sound waves to take a moving movie of the heart, its chambers and valves. This allows us to clearly see which valve has a problem, whether it is a stenosis or a leak, how serious it is and whether the pumping power of the heart is affected.
Sometimes, to get even clearer and more detailed images, we can use Transesophageal Echocardiography (TEE), which is done through the esophagus. This test gives us a much closer look at the valves.
In addition to these basic tests, we may also order additional tests to support the diagnosis and to fully assess the patient’s overall health status. Among these, the ones we use most often are the following:
- Electrocardiogram (ECG)
- Chest X-ray
- Computed Tomography (CT)
- Cardiac Magnetic Resonance (MRI)
In some special cases, especially if bypass surgery is also required, cardiac catheterization (angiography) may also be required to visualize the heart vessels and measure intracardiac pressures. The data obtained from all these tests are evaluated by a multidisciplinary “Heart Team” to determine the most accurate and safest treatment path for the patient.
Why Heart Valve Replacement Surgery is Vital in Aortic Stenosis?
Aortic stenosis is a severe narrowing of the valve of the main artery (aorta) that exits the heart and distributes clean blood throughout the body. This is one of the most common and serious conditions requiring heart valve replacement surgery. We can liken it to a blockage in the main water pipe of a city. The left ventricle, the heart’s main pumping chamber, has to exert enormous pressure to send blood through this narrow doorway to the whole body.
Over time, this constant overwork causes the heart muscle to fatigue and thicken (hypertrophy), and after a while it loses its strength and weakens, leading to heart failure. Once symptoms (chest pain, shortness of breath, fainting) appear in a patient with severe aortic stenosis, the condition rapidly worsens. Without treatment, unfortunately, the patient’s life expectancy is severely shortened. Therefore, when symptoms appear or echocardiography shows that the heart is becoming fatigued, heart valve replacement surgery is no longer an option but a necessity to prevent permanent damage and eliminate the risk to life.
When is heart valve replacement surgery indicated for mitral or other valve problems?
In addition to the aortic valve, other valves can develop serious problems over time and require heart valve replacement surgery.
Mitral regurgitation, for example, is when the valve on the left side of the heart does not close properly and leaks blood back into the lungs. This reduces the efficiency of the heart and causes shortness of breath, palpitations and fatigue. Our priority in mitral valve disease is always to repair the patient’s own valve, if possible. However, if the valve tissue has deteriorated beyond repair due to infection or rheumatic fever, the healthiest and most permanent solution is to replace the valve.
Similarly, conditions such as mitral stenosis (narrowing of the mitral valve) or aortic insufficiency (leaky aortic valve) also impair the functioning of the heart. When these diseases progress and begin to affect the pumping functions of the heart, surgical intervention becomes inevitable to eliminate symptoms and prevent the development of heart failure.
Diseases of the tricuspid and pulmonary valves on the right side of the heart are less common in adults, but can similarly require repair or replacement when they become serious. The goal is always the same: to unburden the heart and restore normal blood circulation.
How Is Heart Valve Replacement Surgery Performed with the Traditional Method?
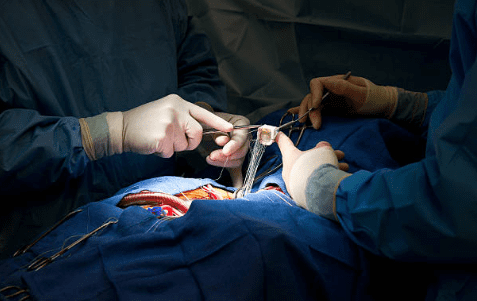
Traditional open heart valve replacement surgery has been practiced for many years. In this operation, the sternum is surgically opened through an incision in the center of the chest. This gives the surgeon the widest and clearest access to the heart and major vessels. This means that even the most complex and delicate operations can be carried out under great control.
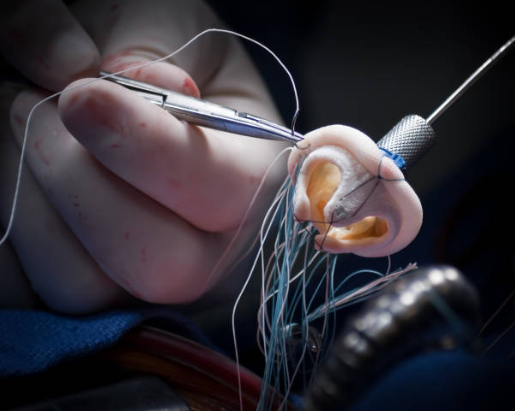
At a critical stage of the operation, the heart is temporarily stopped and a “heart-lung machine” is activated to circulate blood and oxygenate it outside the body. Thanks to this machine, the surgeon can safely work on a bloodless and immobilized heart. The diseased valve is carefully removed and a new prosthetic valve that best suits the patient is carefully sewn in its place. When the procedure is complete, the heart is restarted, the patient is weaned from the heart-lung machine and the sternum is closed, securely joined with special wires. This is a proven approach that can safely perform all types of valve surgery.
What Advantages Does Minimally Invasive (Small Incision) Heart Valve Replacement Surgery Offer to the Patient?
With advances in technology, it is no longer always necessary to completely open the sternum for heart valve replacement surgery. Minimally invasive surgery is a modern technique that allows us to perform this surgery through much smaller incisions. In this method, the breastbone is not cut. Instead, the heart is accessed through a small incision of about 5-7 cm between the ribs, usually in the armpit or under the breast.
The operation is performed with the help of special, long surgical instruments extended through this small incision and a system with a high-resolution camera at the end (endoscope). The surgeon performs the operation with great precision, watching it on a screen. The advantages of this method for the patient are many.
- Less pain: Since there is no large bone incision, postoperative pain is much milder.
- Faster recovery: The hospital stay is shorter and patients return to their normal life and work much more quickly.
- Lower risk: There is less risk of bleeding and infection.
- Better cosmetic result: The scar is much smaller and more aesthetically acceptable.
Minimally invasive procedures may not be suitable for every patient. Factors such as the anatomical structure of the patient, the type of valve disease and the experience of the surgeon are taken into consideration when making this decision.
How is TAVI Heart Valve Replacement Surgery Performed and Who Is It For?
TAVI (Transcatheter Aortic Valve Implantation) is one of the most exciting developments of recent years. With this method, heart valve replacement surgery is performed without a surgical incision, almost like an angio procedure. The rib cage is never opened. Instead, a thin catheter (tube) is inserted through an artery, usually in the groin. A new biological valve is placed on the tip of this catheter, which is compressed.
The catheter is guided through the blood vessels to the heart. Once in the correct position, the new valve is inserted into the patient’s own diseased and narrowed aortic valve and expanded there. The new lid replaces the old lid by pushing it to the edges and starts working immediately.
The main advantage of this procedure is that it eliminates the risks and long recovery period of open heart surgery. The heart is usually not stopped, a heart-lung machine is not needed and the procedure can be performed under sedation rather than general anesthesia. This reduces the hospital stay to 1-2 days and patients can return to their normal lives within a few days. Initially used only for elderly patients with a very high risk of surgery, TAVI is now successfully used in younger and lower-risk patients.
What is the Experience of Heart Valve Replacement Surgery with Robotic Surgery?
Robotic surgery is the pinnacle of minimally invasive surgery. In this technology, the surgeon sits at a special console placed in the room rather than right next to the operating table. From this console, he watches a three-dimensional, magnified and vibration-free image of the heart. The surgeon’s hand movements at the console are projected by robotic arms onto the surgical field as micro-movements that are identical, but much more precise and vibration-free.
In this method, heart valve replacement surgery is performed through several small holes in the chest wall. Robotic arms enter through these holes and perform the surgery. This technology offers extraordinary mobility and precision in areas too narrow for the human hand. It provides a great advantage to the surgeon, especially in complex mitral valve repairs. For patients, it maximizes all the benefits of minimally invasive surgery (less pain, smaller scars, faster recovery). Since the bone is not cut, patients’ postoperative movements are much more comfortable and their return to normal life is significantly accelerated.
Which Prosthetic Valve Types Are Available for Heart Valve Replacement Surgery?
One of the most important questions we need to answer together with the patient after the decision for heart valve replacement surgery is: “Which type of valve will I get?” We basically have two main prosthetic valve options.
- Mechanical Caps: These are extremely robust and durable synthetic covers, usually made of titanium and carbon. Their biggest advantage is that they last a lifetime. Once fitted, they are very unlikely to wear out or deteriorate, which minimizes the risk of future surgery for the valve. However, their most significant disadvantage is that their synthetic surface is prone to forming blood clots. To prevent this clotting and related serious risks such as stroke, patients with these valves must take a lifelong blood thinner (Warfarin/Coumadin) and have regular blood tests (INR monitoring).
- Biological (Tissue) Valves: These valves are usually made from specially treated bovine or porcine heart tissue (pericardium or valve). Their biggest advantage is that they have a very low risk of forming blood clots. This means that the vast majority of patients do not need to take blood thinners for life. This eliminates the risk of bleeding and offers a more comfortable life. However, their main disadvantage is that they wear out over time. Although modern biological valves have a considerably longer lifespan, they can often lose their function after 15-20 years and may require a second heart valve replacement surgery.
How to Determine the Most Appropriate Valve Type and Heart Valve Replacement Surgery for the Patient?
there is no single correct answer to the question “Which valve is right for me?”. This decision is completely personalized and is made jointly with the patient, considering the patient’s condition as a whole. The main factors we consider when making this decision are:
- Age of the Patient: In younger patients with a long life expectancy (usually under 60-65 years of age), the lifelong durability of the mechanical valve may outweigh the lifelong durability of the biological valve. In older patients (usually over 65-70 years of age), biological valves are more often preferred, as they are less likely to undergo reoperation and want to avoid the risks associated with the use of blood thinners.
- Lifestyle and Expectations: Regular blood monitoring and the risk of bleeding may be a limitation for someone who leads a very active lifestyle, plays sports, travels frequently or has a profession that carries a risk of bleeding. In this case, a biological valve may become more attractive.
- Additional Medical Conditions: If a patient is already on lifelong blood thinners for another reason, such as atrial fibrillation, it may make more sense to choose a mechanical valve. Conversely, if a patient has a stomach condition that carries a risk of bleeding, such as an ulcer, a biological valve would be a safer option.
- Valve Position: There may also be slight differences between the aortic position and the mitral position in terms of valve selection.
What is the recovery process at home after heart valve replacement surgery?
| Cover Type | Mechanical valve (long-lasting, requires INR monitoring) or biological valve (shorter-lasting, usually does not require INR monitoring). |
| Recovery Time | Average 10-15 days |
| Medication Use | Lifelong warfarin for mechanical valve; short-term anticoagulant for biological valve. In addition, medications such as beta blockers, ACE inhibitors and statins may be required. |
| INR Monitoring | The target for mechanical valve is usually 2.5-3.5; regular laboratory follow-up is essential. |
| Physical Activity | Light walking is recommended for the first 6 weeks; heavy lifting and pushing are prohibited. After rehabilitation, a transition to moderate exercise can be made. |
| Nutrition | A heart-healthy diet with a balanced vitamin K content, low salt and low fat in general is recommended for those on warfarin. |
| Rhythm and Function Monitoring | Valve function should be monitored regularly by echocardiography; be alert for rhythm disturbances. |
| Complications | There is a risk of valve thrombosis, infection (endocarditis), arrhythmia, bleeding, valve dysfunction. |
| Infection Prevention | Antibiotic prophylaxis, good oral hygiene and wound care are important before dental procedures. |
| Sexual Activity | It is usually possible after 4-6 weeks when physical competence is achieved. |
| Smoking and Alcohol | Definitely not recommended; it has a negative impact on vascular health and valve life. |
| Psychological Support | Chronic disease awareness, lifestyle changes and medication management can create psychological burden. Support recommended. |
| Vehicle Use | It can usually be started after 4-6 weeks, when attention and reflexes are appropriate. |
| Controls | Cardiology follow-up should continue with frequent echocardiography in the first year and regular echocardiography at least once a year thereafter. |
After discharge from hospital, the real healing process begins at home. During this period, it is very important to be patient and listen to the signals your body is sending you. While full recovery after open heart valve replacement surgery usually takes 6 to 8 weeks, it is much shorter after minimally invasive or TAVI.
In the first few weeks, it is normal to feel tired, to lose your appetite, to feel pain or discomfort at the incision site and to have disturbed sleep patterns. Even experiencing emotional fluctuations, sadness or anxiety after surgery is part of this process.
The most important thing to pay attention to during this period, especially if you have had open surgery, is to protect the healing of your breastbone. It takes about 6-8 weeks for the bone to fully fuse. There are some restrictions you must follow during this process:
- avoiding lifting objects heavier than 3-5 kilograms
- Avoiding pushing and pulling movements (such as using a vacuum cleaner, mowing the lawn)
- Lack of strength in the arms when getting out of bed or chair
- Not driving for the first 4-6 weeks
Return to normal activities should be gradual. The best exercise is walking. You can gradually increase your fitness by walking a little more each day than the day before. Sexual activity can usually be resumed after 4-6 weeks, when you feel ready. Return to work can vary between 6 and 12 weeks depending on the nature of the work.
What Should Nutrition and Diet Be After Heart Valve Replacement Surgery?
Proper nutrition is vital for both the rapid healing of your wounds and the long-term health of your heart. In the postoperative period, our aim is to follow a heart-friendly diet that provides the body with the necessary building blocks to repair itself and does not tire the heart.
Here are the foods that should form the basis of your nutrition plan:
- Fresh fruits and vegetables
- Whole grains (oats, bulgur, whole wheat bread)
- Lean protein sources (fish, chicken, legumes)
- Healthy fats (olive oil, avocado, walnuts)
At the same time, there are also things you should limit or avoid for your heart health. Salt (sodium) is one of them. Salt can cause fluid retention in the body and increase blood pressure. Here are other things you should also stay away from:
- Processed and packaged foods
- Sugary drinks and sweets
- Foods containing saturated and trans fats (fried foods, pastries)
If you are taking Warfarin (Coumadin) as a blood thinner, you do not need to completely eliminate vitamin K-rich green leafy vegetables (such as spinach, kale, broccoli) from your diet. It is important to consume approximately the same amount of these foods every day to ensure that the level of your medicine in your blood remains constant.
Why Long-Term Follow-Up After Heart Valve Replacement Surgery is Important?
Heart valve replacement surgery is not the end but the beginning of a new journey for your heart health. On this journey, you will build a lifelong partnership with your cardiology team. Regular follow-up and check-ups are the most important part of this new life.
The main purpose of this follow-up is to monitor whether the new valve is working properly. The most important tool for this is echocardiography (ECHO). After surgery, an ECHO is performed at regular intervals (usually annually) to evaluate the function of the valve in detail.
Patients with prosthetic valves are also at a slightly higher risk of a serious valve infection called “infective endocarditis”. Good oral and dental hygiene is very important to minimize this risk. You may need to take prophylactic antibiotics before some medical procedures, such as tooth extraction. Therefore, you should tell all your doctors and especially your dentist that you have a prosthetic heart valve.
For patients with mechanical valves, lifelong blood thinners and regular INR monitoring are the most critical elements of this long-term follow-up. Patients with biological valves are closely monitored with annual ECHO checks in case the valve wears out over time. Thanks to these regular checks, a potential problem can be detected at an early stage and the necessary measures can be taken in time.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.