Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, particularly the left ventricle. This condition can obstruct blood flow, cause arrhythmias, and increase the risk of sudden cardiac death.
Clinical symptoms of hypertrophic cardiomyopathy include shortness of breath, chest pain, palpitations, and syncope. Many patients remain asymptomatic for years, making regular cardiological screening crucial in families with a history of the disease.
Diagnosis relies on echocardiography and cardiac MRI, which reveal myocardial hypertrophy and possible left ventricular outflow obstruction. Genetic testing can identify familial transmission and assist in risk stratification and early intervention.
Treatment options vary from beta-blockers and calcium channel blockers to surgical septal myectomy or alcohol septal ablation in resistant cases. Implantable cardioverter-defibrillators are considered for patients at high risk of sudden cardiac death.
| Definition | A genetic cardiomyopathy characterized by thickening of the walls of the heart muscle, especially the left ventricle |
| Causes | Genetic (autosomal dominant inherited gene mutations), familial predisposition |
| Risk Factors | Family history of HCMP, genetic mutations, young age in some cases, male gender |
| Symptoms | Shortness of breath, fatigue, chest pain, palpitations, fainting (especially on exertion), sometimes sudden cardiac arrest (in young people and athletes) |
| Diagnostic Methods | Echocardiography (the most important diagnostic method), ECG, cardiac MRI, genetic testing, exercise testing |
| Treatment Methods | Beta blockers, calcium channel blockers, antiarrhythmic drugs, septal myectomy (surgery), alcohol septal ablation, implantable cardioverter defibrillator (ICD), lifestyle modifications |
| Complications | Arrhythmia, sudden cardiac death, heart failure, stroke, mitral valve insufficiency, endocarditis |
| Prevention Methods | Family screening and genetic counseling, ICD implantation in patients at high risk of sudden death, limitation of exertion, regular follow-up and controls |
What Causes Hypertrophic Cardiomyopathy and Is It Familial?
Yes, the vast majority of cases of Hypertrophic Cardiomyopathy are familial and have a genetic root cause. This means that the disease can be passed down from generation to generation. There are proteins that make our heart muscle cells contract and relax. A “typo” or mutation in the genes that govern the production of these proteins is the main cause of HCMP. This faulty genetic code leads to abnormal production of heart muscle proteins and, over time, thickening of the heart wall.
The genetic transmission of the disease usually follows a pattern that we call “autosomal dominant”. This means: Inheriting the disease-causing gene from just one parent is enough to cause the disease. Therefore, the probability that a mother or father with HSMP will pass on this genetic predisposition to each of their children is as high as P.
This makes the diagnosis of HCMP a “family issue” rather than a personal health problem. When someone in a family is diagnosed with HCMP, their first-degree relatives – parents, siblings and children – are also potentially at risk. Even if these people have no symptoms, screening is vital to catch a possible disease at an early stage and take precautions. Genetic counseling is the most important guide for families in this process.
However, a known genetic mutation does not underlie every case. In some patients, no detectable genetic cause may be found with available tests. In these cases, other genetic factors that have not yet been identified or non-genetic factors such as high blood pressure are thought to play a role.
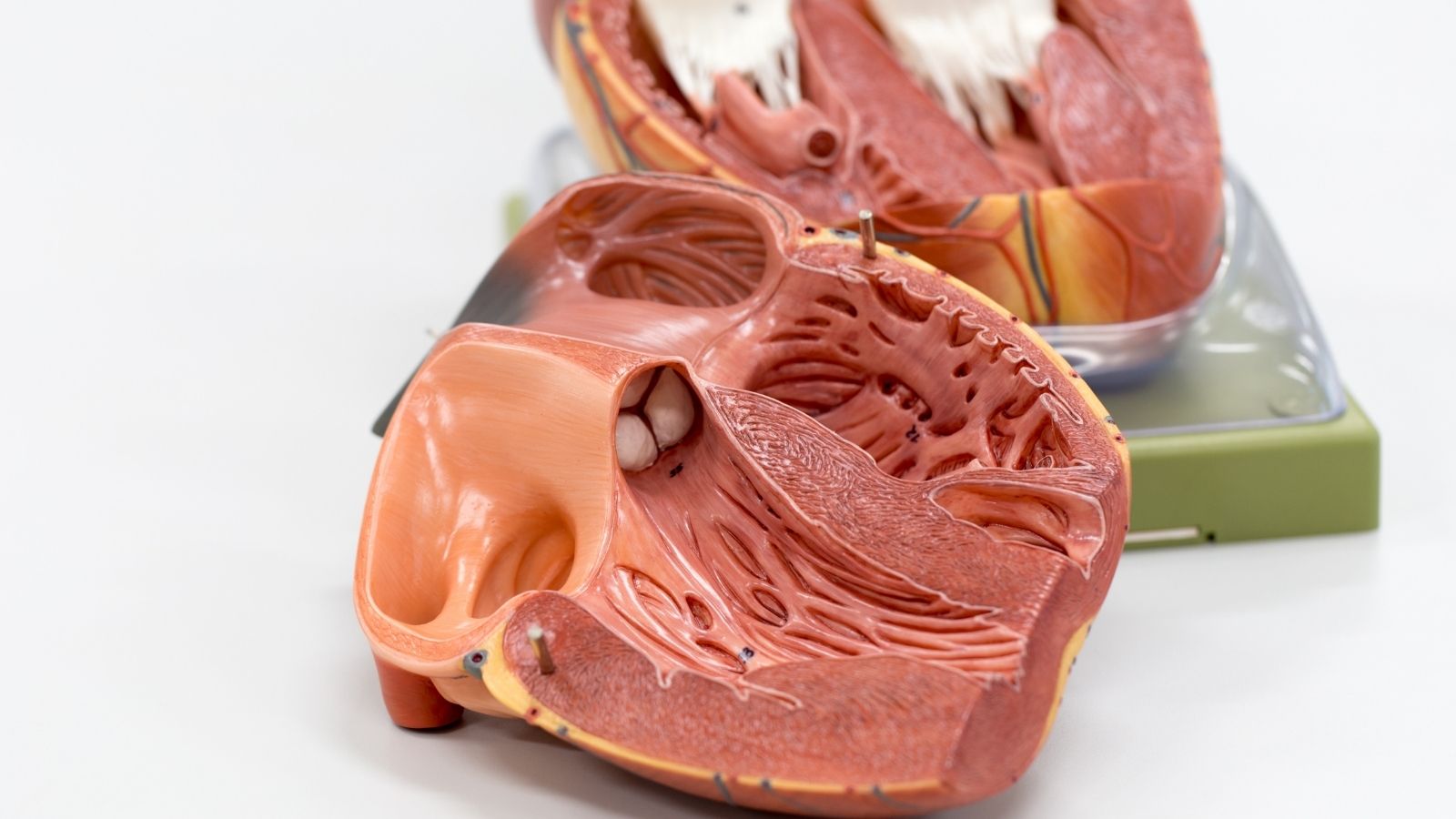
How Hypertrophic Cardiomyopathy Impairs Heart Functioning
A thickened heart muscle affects the normal functioning of the heart in several basic ways. We can liken it to problems in the plumbing system of a house; tightness or constriction in one place affects the whole system.
- Blockage of Blood Flow (Obstruction): This is the most common effect. The thickened muscle, especially the wall of the septum between the two ventricles, narrows the main valve (aortic valve opening) through which blood leaves the heart and distributes throughout the body. This can be compared to the sudden closure of one lane of a highway during rush hour. Traffic jams and the flow slows down. The heart has to exert much more effort to move blood through this narrow space. This strain causes symptoms such as shortness of breath and chest pain, especially when the heart has to work fast, such as during exercise.
- Hardening of the Heart (Diastolic Dysfunction): The thickened muscle also loses its elasticity and becomes stiff. For the heart to work efficiently, it needs to contract, then relax completely and refill with blood. In HCMP, the heart becomes like a hardened balloon; it cannot relax enough and cannot take in enough blood. As a result, less blood is pumped into the body with each beat. This is a major cause of fatigue and reduced capacity for exertion.
- Mitral Valve Problems: This narrowing and pressure changes within the heart also affect the mitral valve between the left atrium and the left ventricle. Blood passing rapidly through the narrow space creates a vacuum effect, pulling the anterior leaflet of the valve towards itself. this phenomenon, which we call “Systolic Anterior Movement” (SAM), both exacerbates the stenosis of the blood outflow and prevents the valve from closing completely, causing blood to leak backwards into the auricle (mitral regurgitation). This leakage further increases the load on the heart.
- Cellular Disorganization: When examined under a microscope, the heart muscle cells in HCMP are not arranged like a regular brick wall, but rather like a tangled mass of yarn. this cellular chaos, called “myofiber disarray”, can disrupt the normal transmission of the heart’s electrical signals. This is one of the most dangerous mechanisms predisposing some patients to severe arrhythmias and the risk of sudden cardiac death.
What are the Types of Hypertrophic Cardiomyopathy?
We basically divide HCMP into two main types. This distinction plays a critical role in determining the patient’s treatment plan, as the management of each type requires different approaches.
The two main forms of the disease are:
- Obstructive Hypertrophic Cardiomyopathy (HOKMP)
- Non-obstructive Hypertrophic Cardiomyopathy
Obstructive HCMP, as the name suggests, is the form in which thickened heart muscle mechanically obstructs the way blood leaves the heart. About two-thirds of patients fall into this group. Most symptoms are caused by this mechanical obstruction and treatment is focused on eliminating this obstruction. In non-obstructive HCMP, there is no obvious obstruction in the blood flow pathway. The main problem here is not a mechanical obstacle, but the inability of the thickened and stiffened heart muscle itself to work efficiently. In these patients, treatment focuses on drug therapies that facilitate relaxation of the heart and manage the symptoms of heart failure.
What Symptoms Does Hypertrophic Cardiomyopathy Cause?
The symptoms of Hypertrophic Cardiomyopathy can vary greatly from person to person. Some people may not feel anything for years, while others may have symptoms that seriously affect their quality of life.
The most common symptoms are as follows:
- Shortness of breath, especially during physical activity
- Chest pain or tightness with exertion
- Feeling that the heart is beating fast, strong or irregularly (palpitations)
- Dizziness or feeling dizzy
- Sudden loss of consciousness (fainting)
- Abnormally fast fatigue and constant exhaustion
- Heat in the feet, legs or abdomen (edema)
These symptoms usually appear gradually and patients may adapt over time. For example, without realizing it, a person may start to avoid climbing stairs or walk more slowly and attribute this to aging or deconditioning. Fainting (syncope), especially if it occurs during exertion, is an alarm sign that must be taken seriously as it may indicate a serious underlying problem. This is why it is so important for people with a family history of HCMP or sudden death at a young age to have regular check-ups, even if they do not feel any symptoms.
How is Hypertrophic Cardiomyopathy Diagnosed?
Diagnosing Hypertrophic Cardiomyopathy is like putting the pieces of a puzzle together. A definitive diagnosis is not made with a single test, but by combining a series of assessments.
The main methods used in the diagnostic process are as follows:
- Detailed Medical and Family History
- Physical Examination
- Echocardiogram (ECHO)
- Electrocardiogram (ECG)
- Cardiac Magnetic Resonance (Cardiac MR)
- Effort Tests
- Genetic Tests
The process starts with a detailed interview with you. We will try to understand your symptoms, when they started and how they affect your life. Even more important is your family’s health history. Asking about a known family history of heart disease or a sudden loss at a young age allows us to suspect a genetic background. On physical examination, the “murmur” that we can hear when listening to your heart with a stethoscope, a sign of turbulence in the blood flow, is an important clue to obstructive HCMP.
Our most valuable diagnostic aid is the Echocardiogram (ECHO). This is an ultrasound of the heart. Using sound waves, we obtain vivid, moving images of your heart. With an ECHO, we can measure millimeter by millimeter how thick the heart walls are, assess the heart’s contractile and relaxation functions and, most importantly, get a clear picture of whether there is a blockage (obstruction) in the blood flow pathway. An electrocardiogram (ECG) is a simple test that records the electrical activity of the heart and often gives the first clues about thickening of the heart muscle.
Sometimes, especially when ECHO fails, we turn to a more advanced imaging method such as Cardiac MRI. Cardiac MRI produces a much more detailed, three-dimensional map of the heart. Its biggest advantage is that it can show scar tissue (fibrosis) within the heart muscle. The amount of this scar tissue gives us valuable information about the risk of future arrhythmias.
What are the Risks of Hypertrophic Cardiomyopathy?
Most patients with HCMP lead a normal life with proper follow-up and treatment. However, the disease comes with some potential risks. Recognizing these risks is the first step to managing them.
The main risks associated with the disease are:
- Atrial Fibrillation (AFib)
- Stroke (Felç)
- Heart Failure
- Sudden Cardiac Death (SCD)
Atrial fibrillation is a common rhythm disorder in which the upper chambers of the heart (the atria) contract irregularly and rapidly, and is more common in patients with HCMP. This can predispose to blood stasis and clot formation in the ear canals. If a clot travels to the brain, it can cause a stroke. Therefore, anticoagulant therapy is vital in HCMP patients with atrial fibrillation.
Over time, the thickened and stiffened heart muscle can become tired and unable to pump enough blood to meet the body’s needs. We call this condition heart failure. This is usually encountered in advanced stages of the disease.
The most feared risk is Sudden Cardiac Death (SCD). This is a sudden cardiac arrest due to a life-threatening rhythm disturbance. This risk is quite low in the general population of HCMP (less than 1% per year) and is only concentrated in a small group of patients with certain high-risk factors. We can identify these high-risk patients by looking at factors such as a family history of sudden death, frequent fainting, and an excessively thick heart wall (usually >30 mm). For these patients, we can almost completely eliminate this risk with implantable cardioverter defibrillators (ICDs), which work like a lifesaver, correcting the rhythm by shocking the heart when needed.
What are the Options for the Treatment of Hypertrophic Cardiomyopathy?
Our goal in treating HCMP is to control symptoms, improve your quality of life and prevent serious risks. Treatment is not like “one size fits all”; it is tailored to the individual with the precision of a tailor. We take many factors into account when creating your treatment plan, such as the type of your disease, the severity of your symptoms, your age and your general health. Treatment usually proceeds in a stepwise approach, starting with the simplest and least invasive methods and progressing to more advanced options if necessary.
What Are Non-Surgical Treatments for Hypertrophic Cardiomyopathy?
The first step in treatment is always lifestyle modifications and medication. For many patients, control of symptoms can only be achieved through these steps.
Here are some positive changes you can make to your lifestyle:
- A balanced, salt-poor diet
- Maintaining ideal weight
- Smoking cessation
- Restricting alcohol consumption
- Doctor-approved regular exercise
Exercise is particularly important. In the past, almost all sports activities were forbidden to patients with HCMP. But our modern approach is much more balanced. Avoiding competitive and high-exertion sports such as heavy lifting and sprinting is usually fine. But we know that regular, moderate-intensity aerobic exercise such as brisk walking, swimming and cycling is safe and even beneficial for many patients and improves quality of life. Together we should determine the best exercise plan for you.
The main agents we use in the treatment of herpes are:
- Beta Blockers
- Calcium Channel Blockers
- Cardiac Myosin Inhibitors (such as Mavacamten)
- Antiarrhythmic Drugs
- Anticoagulants (Blood Thinners)
Beta blockers and calcium channel blockers are the cornerstones of treatment. They slow the heart rate and reduce the force of contraction. This gives the heart more time to relax and fill with blood, relieves congestion in the outflow tract and reduces symptoms such as chest pain. Cardiac myosin inhibitors are newer, smarter drugs that act on the underlying mechanism of the disease. They help the heart to relax by preventing excessive contraction of heart muscle proteins. Antiarrhythmic drugs are added if there is an arrhythmia, and blood thinners if there is a risk of stroke.
What is Septal Myectomy Surgery in Hypertrophic Cardiomyopathy and Who Is It Performed?
The “gold standard” treatment for obstructive HCMP patients who, despite drug treatment and lifestyle changes, continue to have severe symptoms (shortness of breath, chest pain, fainting) that interfere with daily life is septal myectomy surgery. It is an open heart surgery and its purpose is to surgically remove the excess muscle tissue that is blocking the blood flow.
In the operation, the heart is stopped with the help of a heart-lung machine and the part of the thickened septum muscle that blocks the blood flow is carefully cut out through the aortic valve. This process can be likened to a sculptor chiseling away the excess from a block of marble to create a masterpiece. The aim is to create a wide and smooth pathway through which blood can flow freely. During this surgery, mitral valve problems that often accompany it can also be repaired in the same session.
Septal myectomy is a technically precise operation and its success is directly dependent on the surgeon’s experience. When performed in an experienced center and by a surgeon who has performed a high number of operations in this field, the success rates are above ‘and the risks are low. An experienced surgeon knows where and how much muscle to remove. The most common reason why symptoms persist after an inadequate surgery is not that the muscle has regrown, but that not enough muscle tissue was removed in the initial surgery. Therefore, choosing the right center for this surgery is the most critical step in treatment. The recovery process is usually rapid and patients can return to normal activities within a few months.
What Are Other Interventional Methods for Hypertrophic Cardiomyopathy?
There are other interventional methods that we use as an alternative to surgery or as a complement to surgery.
These methods are:
- Alcohol Septal Ablation (ASA)
- Implantable Cardioverter Defibrillator (ICD)
Alcohol Septal Ablation (ASA) may be an alternative for some patients who are at high risk for open heart surgery (e.g. advanced age or serious comorbidities). In this method, a catheter inserted through the groin, like an angiogram, is used to find a small vessel that supplies the thickened septum muscle. A very small amount of pure alcohol is injected into this vessel to create a controlled heart attack in that area. This tissue, which has lost its vitality, thins and shrinks over time, reducing the tightness. Although less invasive than myectomy, it is associated with higher inherent risks, such as the need for a permanent pacemaker.
The Implantable Cardioverter Defibrillator (ICD) is a protective shield, not a treatment method. Its purpose is to save lives by detecting dangerous arrhythmias that can lead to sudden cardiac death within seconds and delivering an electric shock to the heart. The ICD does not treat symptoms; it is only implanted to provide protection, like a “lifesaver”, to patients identified as being at high risk of sudden death.
What Is the Long-Term Life Expectancy of Hypertrophic Cardiomyopathy Patients?
In modern medicine, a diagnosis of Hypertrophic Cardiomyopathy is no longer a cause for despair. With the correct diagnosis, personalized treatment and regular follow-up, the overwhelming majority of patients enjoy a normal or near-normal life expectancy and quality. Annual mortality rates have dropped to as low as 0.5% in patients followed in specialized centers.
This positive picture in no way diminishes the importance of regular follow-up throughout life. As CDMP can be a progressive disease, it is important to monitor the condition closely, be prepared for possible changes and update the treatment plan as needed.
What a typical follow-up plan should include:
- Annual or personalized cardiologist check-ups
- Periodic ECHO to monitor the structure and function of the heart
- Periodic ECG to check the electrical condition of the heart
- Holter (rhythm) monitoring in suspected arrhythmia
Your strongest tool in this journey is knowledge. Understanding your disease, knowing the treatment options and working as a partner with your treatment team will put you in control. CDMP is a condition that can be successfully managed with the right guidance, a proactive approach and the opportunities offered by modern medicine.
Frequently Asked Questions
What is hypertrophic cardiomyopathy?
It is a genetic heart muscle disease characterized by abnormal thickening of the heart muscle walls (hypertrophy).
Which part of the heart does HCMP affect?
Usually the left ventricular wall is affected; sometimes the entire heart muscle may be thickened.
What are the symptoms of HCMP?
Chest pain, palpitations, dizziness, fainting and shortness of breath on exertion may occur. Some people may have no symptoms at all.
Is this disease dangerous?
Yes, it can lead to arrhythmias that can cause sudden cardiac arrest, especially important in young people and athletes.
Is it Genetic?
Yes, it is an autosomal dominant genetic disease. Family members should also be screened.
How is HCMP diagnosed?
It is diagnosed by ECG, echocardiography (ECHO), cardiac MRI and genetic testing.
Does CDMP always give symptoms?
No, many people can live without symptoms for a long time; some go to the doctor with sudden symptoms.
Is there a cure?
There is no definitive cure, but drug therapy, ablation, surgery and device treatments are used to control symptoms.
Is drug treatment enough?
Symptoms can be alleviated with beta-blockers, calcium channel blockers and antiarrhythmic drugs.
Is surgical treatment necessary?
The obstructive form may require surgical intervention called septal myectomy.
What is alcohol septal ablation?
It is a non-invasive treatment method in which alcohol is injected into the thickened heart muscle to shrink it.
Do I need a pacemaker or ICD?
Implantable cardioverter defibrillators (ICDs) may be recommended for patients at risk of sudden death.
Is it safe to exercise?
Heavy exercise and competitive sports are risky. Light-moderate exercises should be performed under the supervision of a doctor.
Is HCMP progressive?
Yes, over time the heart muscle can become thicker and heart function can be affected.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.