Heart diseases are conditions that impair the structure and function of the heart, leading to circulation problems. The main types include coronary artery disease, arrhythmias, heart valve disorders, and heart failure, each carrying specific risk factors and clinical manifestations.
Coronary artery disease results from narrowing of the heart’s vessels due to atherosclerosis. This reduction in blood flow may cause chest pain, shortness of breath, or myocardial infarction. Preventive measures such as healthy nutrition, exercise, and medical follow-up play a vital role.
Arrhythmias represent rhythm disturbances that may cause palpitations, dizziness, or fainting. They can be benign or severe, requiring detailed diagnosis through electrocardiography and treatment with medication, ablation, or device implantation depending on the severity.
Valve diseases and heart failure constitute advanced forms of heart disease. Valve dysfunction alters blood circulation within the heart, while heart failure occurs when pumping capacity declines. Both conditions necessitate cardiological evaluation and may require surgical treatment.
What Are Heart Diseases and How Are They Different from Cardiovascular Diseases?
Although often used interchangeably in everyday life, there is an important difference between “heart disease” and “cardiovascular disease”. Cardiovascular disease is like a big umbrella. Under this umbrella are all conditions that affect not only the heart but also the arteries and veins in the brain, legs and other parts of the body. For example, a stroke affecting the blood vessels in the brain or narrowing of the blood vessels in the legs (peripheral arterial disease) are also cardiovascular diseases.
“Heart disease” refers to a more specialized group under this larger umbrella and describes conditions that directly affect the heart itself, i.e. the heart muscle, valves or the electrical system that regulates its rhythm. In short, every heart disease is also a cardiovascular disease, but not every problem involving the vascular system is directly a heart disease. Knowing this distinction will help you interpret your body’s signals more accurately and consult the right specialist.
What Symptoms Does Heart Disease Generally Cause?
Heart disease can manifest itself through various signals in the body. But one of the most worrying situations is that the disease can remain completely “silent” until it leads to a serious event. It is therefore important to take any of the symptoms listed below seriously, especially if you have risk factors. The most common symptoms of heart disease are:
- Pressure, tightness, heaviness or burning sensation in the chest
- Shortness of breath (especially with exertion or lying down)
- Above normal fatigue that does not go away with rest
- Palpitations (irregular, rapid or “racing” heartbeat)
- Dizziness or lightheadedness
- Blackout or fainting (syncope)
- Swelling in the ankles, legs or abdomen (edema)
- Pain radiating to the left arm, neck, jaw, back or stomach
- Cold sweating
- Nausea
It should be noted that women, the elderly and diabetics in particular may experience more subtle signs of heart problems, such as indigestion, extreme fatigue or back pain, instead of these classic symptoms. Unexplained and emerging changes in your body are an important reason to consult a specialist.
Which Risk Factors Increase the Chances of Heart Disease?
Some risk factors are with us regardless of our lifestyle or choices. While we cannot change them, knowing them is like a warning sign to focus more on other areas we can control. These factors are not a fate but a guide to be more careful. Major risk factors that cannot be changed:
- Advancing Age: As we age, blood vessels lose their elasticity and plaque build-up becomes easier. over 65 years of age is the period when the risk is most pronounced.
- Gender: In men, the risk usually starts to increase after the age of 45. In women, the risk level increases rapidly after menopause, starting at about 55 years of age.
- Family History: This is one of the strongest indicators. If a first-degree relative, such as a mother, father or sibling, is diagnosed with heart disease at an early age (before the age of 55 in men and 65 in women), your risk increases due to your genetic predisposition. This makes it necessary to be more vigilant for signs of heart disease at a young age.
- Ethnicity: It has been scientifically shown that some ethnic groups are more prone to heart disease due to a combination of genetic and environmental factors.
If you have one or more of these factors, it makes regular health check-ups and healthy living habits even more important for you.
What Are Lifestyle Modifiable Heart Disease Risk Factors?
The most important area where you can take control over your heart health is through your lifestyle habits. These factors often create a domino effect; the presence of one triggers the other. For example, an unhealthy diet and inactivity can lead to obesity, and obesity can lead to high blood pressure and diabetes. Breaking this chain is possible even with the smallest steps. Here are the main risk factors you can control:
- High blood pressure (Hypertension)
- High blood cholesterol
- Smoking and use of other tobacco products
- Diabetes (Diabetes)
- Overweight and obesity
- Physical inactivity
- Unhealthy eating habits
- Excessive alcohol consumption
- Intense and unmanageable stress
- Untreated sleep apnea
The first three of these factors in particular – high blood pressure, high cholesterol and smoking – are considered the “key triad” for heart disease and affect a significant proportion of the population.
How Does Coronary Artery Disease, the Most Common Type of Heart Disease, Develop?
Coronary artery disease (CAD) is the most common disease in modern societies and the number one cause of heart attacks. At the heart of this disease is “atherosclerosis”, or hardening of the arteries. This process can be likened to a water pipe that gradually becomes clogged. Over the years, bad cholesterol, fat and other waste materials circulating in the blood stick to the inner walls of the arteries that feed the heart, forming layers called “plaque”.
As these plaques grow over time, they narrow the inside of the artery and restrict the passage of blood. The heart needs more oxygen, especially during moments of exertion such as walking or climbing stairs. When the narrowed vessel is unable to meet this need, the typical chest pain called “angina” occurs. This is the chronic and slowly progressive side of the disease.
But the real danger comes when one of these plaques suddenly ruptures. The body sends clot cells to the area to repair the tear and a blood clot forms. This clot suddenly and completely blocks the already narrow vessel, cutting off the blood supply to the heart muscle. This is known as a “heart attack” (myocardial infarction) and is one of the most dangerous forms of heart disease. For this reason, CAD is like an insidious enemy that can progress without warning and it is vital to keep risk factors under control.
How Heart Diseases Associated with Heart Failure Affect the Body
Contrary to its name, heart failure is not a condition in which the heart completely “stops” or “dies”. Rather, it is a chronic condition in which the heart loses its power as a pump, unable to circulate enough blood efficiently to meet the body’s needs. It is often the result of another disease (such as uncontrolled high blood pressure, previous heart attack, valvular disease) that has damaged the heart over the years and has not been treated well.
When the pumping function of the heart weakens, blood begins to pool backwards in the system. If the problem is on the left side of the heart, blood pools in the lungs, leading to shortness of breath, which is particularly severe when lying down or during exertion. If the problem is on the right side, blood pools in the legs, ankles and abdomen, causing swelling (edema). This condition of fluid accumulation is also called “congestive heart failure”. The most obvious signs are persistent fatigue, reduced exertional capacity and shortness of breath.
Why Do Arrhythmias, Heart Diseases Affecting Heart Rhythm, Occur?
Our heart is an organ with a perfect rhythm, beating about 100,000 times every day. This rhythm is governed by a complex electrical system within the heart itself. This system has a conductor: the sinoatrial node. The electrical impulses initiated by this conductor spread through specific pathways throughout the heart muscle, ensuring regular and coordinated contraction. Arrhythmias are caused by a malfunction at any point in this electrical system. Signals may start in the wrong place, may be too fast or slow, or may not be transmitted properly over normal paths.
Arrhythmias can either be a symptom of an existing heart disease (such as coronary artery disease, heart failure) or they can cause other problems (such as heart failure, stroke) by exhausting the heart on their own. The most common symptoms are:
- Palpitations
- Feeling of “misfire” in the chest
- the feeling of “flapping bird wings”
- Dizziness
- Eye darkening
- Fainting
- Shortness of breath
- Fatigue
What Problems Are Caused by Heart Diseases Affecting the Heart Valves?
Inside our heart, there are four valves that allow blood to flow in one direction, between the chambers and from the heart to the body. We can think of them as mechanical doors that only open in one direction. Valvular heart disease occurs when the mechanism of these valves breaks down. This deterioration basically takes two forms:
- Stenosis (Stenosis): Just as doors rust and calcify over time, the valves harden and cannot open. The heart has to exert much more force than normal to push the blood through this narrowed door. Over time, this fatigues and thickens the heart muscle.
- Regurgitation (regurgitation): In this condition, the doors do not close and some blood leaks backwards with each closure. To meet the body’s needs, the heart works harder to compensate for this leaking blood. This causes the heart to enlarge and fatigue over time.
Valvular diseases can be congenital heart disease or may develop later in life due to aging, rheumatic fever or infections. Usually the first sign is an abnormal sound called a “murmur”, which the doctor hears with a stethoscope during the examination.
What are Cardiomyopathies, Diseases of the Heart Muscle?
Unlike many other heart problems, cardiomyopathy is a group of diseases in which the problem lies directly in the structure or function of the heart muscle (myocardium). In these cases, the coronary vessels or valves may be normal, but the motor itself, the heart muscle, is diseased. These diseases cause the heart muscle to become weak, abnormally thick or stiff. This prevents the heart from doing its job of pumping blood.
Some forms of cardiomyopathy are genetically inherited, while others can develop later in life due to long-term high blood pressure, viral infections or excessive alcohol consumption. The main types are:
- Dilated Cardiomyopathy
- Hypertrophic Cardiomyopathy
- Restrictive Cardiomyopathy
In Dilated Cardiomyopathy, the most common type, the heart’s pumping chambers expand like a balloon and become thinner, which severely reduces the force of contraction. In Hypertrophic Cardiomyopathy, the heart muscle becomes abnormally thick. This thickening makes it difficult for the heart to relax and fill with blood and is one of the most common causes of sudden death, especially in young athletes. In Restrictive Cardiomyopathy, the rarest type, the heart muscle loses its elasticity, becomes stiff and cannot fill with enough blood.
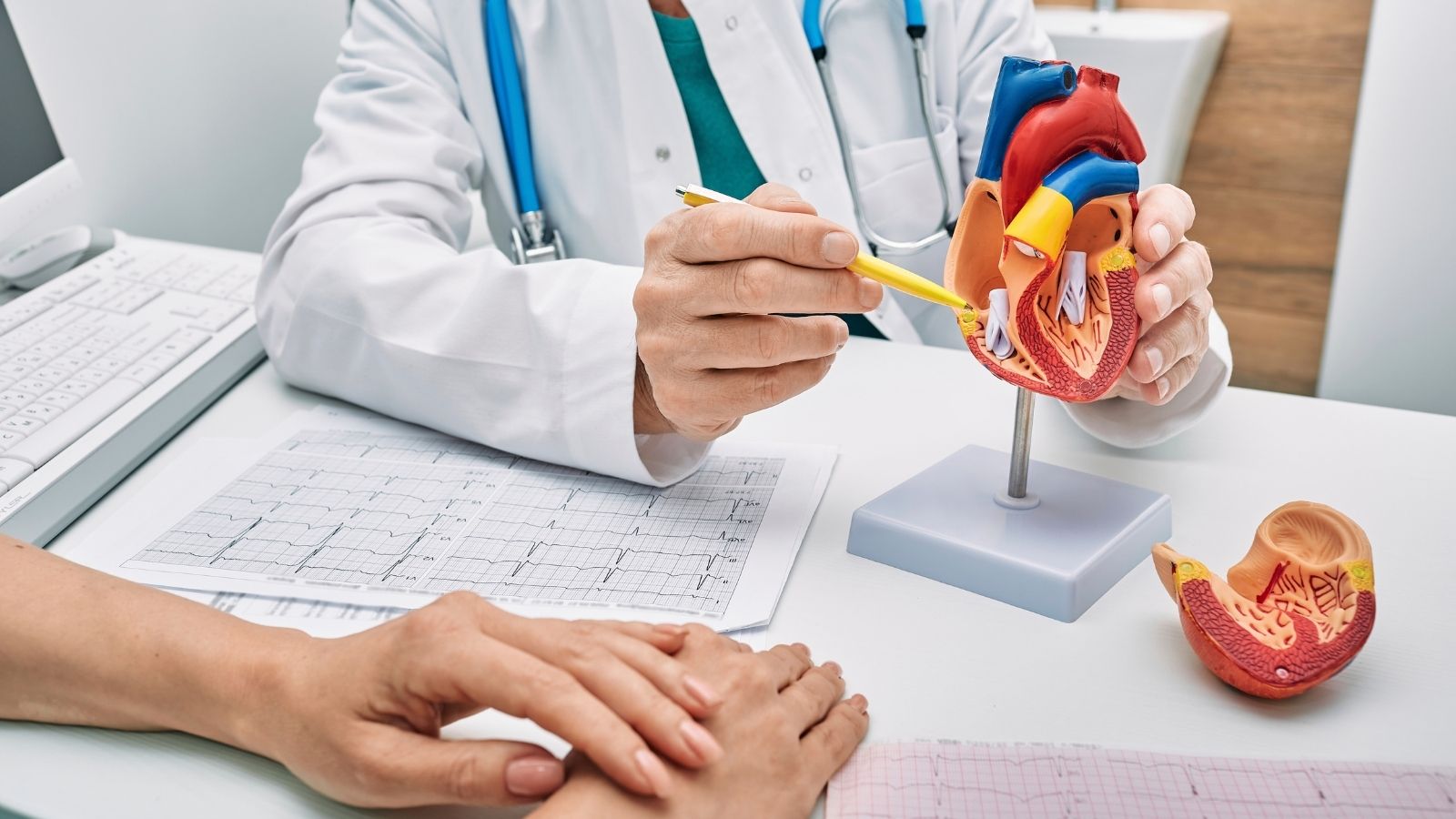
Which Basic Diagnostic Tests Are Performed in Suspected Heart Disease?
The right diagnosis is the first step to the right treatment. When a physician is consulted with a suspicion of heart disease, the process usually begins with listening to the patient’s history and a detailed physical examination. After these first steps, some basic tests are performed to clarify the diagnosis. These tests are usually simple, painless and give quick results.
- Electrocardiogram (ECG): The most basic test that transcribes the electrical activity of the heart on a piece of paper through electrodes attached to the body.
- Blood Tests: Levels of certain markers in the blood, such as cholesterol, sugar and troponin, give important clues about heart health and possible damage.
- Holter Monitoring: It is a portable ECG device that continuously records the heart rhythm for 24 or 48 hours to catch symptoms that don’t always occur, such as palpitations.
What Role Do Imaging Methods Play in the Diagnosis of Heart Diseases?
When basic tests point to a problem, more advanced imaging is used to get a snapshot of the heart’s structure, function and blood flow. These tests play a key role in confirming the diagnosis.
- Echocardiogram (ECHO): Also known as ultrasound of the heart. It uses sound waves to create moving images of the heart and provides invaluable information about the strength of the heart muscle, the condition of the valves and the size of the chambers.
- Stress (Effort) Test: A controlled strain on the heart (usually on a treadmill) that aims to reveal problems such as atherosclerosis that are hidden at rest.
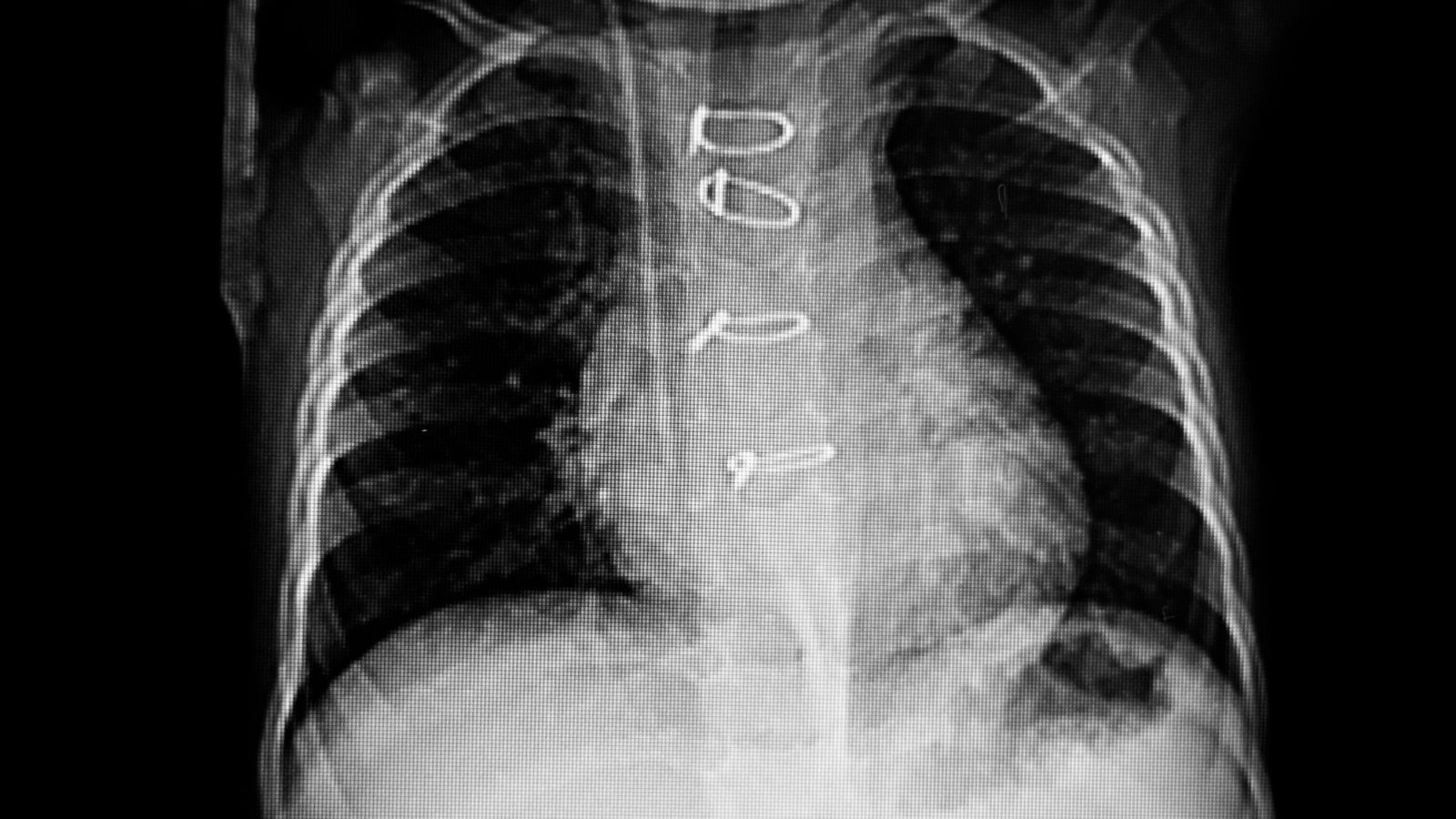
- Cardiac Computed Tomography (CT): Creates detailed, three-dimensional images of the heart and coronary arteries using X-rays. “Coronary CT angiography” is particularly effective in showing stenoses in the arteries.
- Cardiac Magnetic Resonance (MRI): It is a very detailed, radiation-free imaging method used to evaluate heart muscle diseases, congenital anomalies and damage to heart tissue.
When Is Angiography, an Advanced Method, Used to Diagnose Heart Diseases?
When all other tests raise a strong suspicion that there may be a serious blockage in the coronary arteries, angiography comes into play. Angiography is the “gold standard” procedure used to “roadmap” the coronary arteries. This procedure is not only a diagnostic tool, but could also be the beginning of a potential treatment modality.
During the procedure, a very thin catheter (tube) is inserted through an artery, usually in the groin or wrist, to access the heart vessels. A special dye is injected through the catheter, which makes the vessels visible on X-rays, and serial films are taken. These films clearly show the location, number and severity of the stenosis. Based on this map, the most appropriate treatment (medication, stent or bypass surgery) for the patient is decided.
How Effective Are Lifestyle Changes in Managing Heart Disease Risk?
Despite all the medicines and surgeries available in modern medicine, the cornerstone of heart health is always a healthy lifestyle. These changes are the most powerful interventions you can make, both to never get heart disease (primary prevention) and to stop the progression of existing disease (secondary prevention).
It is important to adopt a heart-healthy diet. Here are some basic principles to enrich your table:
- Fresh fruits
- Colorful vegetables
- Whole grains (whole wheat bread, bulgur, oats)
- Legumes (chickpeas, lentils, beans)
- Healthy fats (olive oil, avocado)
- Fatty fish (salmon, sardines)
- Nuts (walnuts, almonds)
Regular physical activity is like a workout that strengthens your heart. Your goal should be at least 150 minutes of moderate-intensity aerobic exercise (brisk walking, cycling, swimming) per week. Quitting smoking is the best decision you can make for your heart health. The risk starts to decrease from the first day after quitting smoking. Maintaining a healthy weight, managing stress and getting enough sleep are also integral parts of this holistic approach.
Which Drug Groups Are Used in the Treatment of Common Heart Diseases?
Medication is another pillar that supports lifestyle changes and plays a vital role in the management of heart disease. These medicines control symptoms, slow disease progression and help prevent serious events such as heart attacks. Main groups of commonly used medicines:
- Statins: Lower bad cholesterol (LDL) and slow the buildup of plaque in the arteries.
- Beta Blockers: Slow the heart rate and reduce the workload of the heart.
- ACE Inhibitors / ARBs: Lower blood pressure by relaxing blood vessels.
- Antiplatelets (e.g. Aspirin, Clopidogrel): Prevent clot formation by preventing the adhesion of blood platelets.
- Anticoagulants (e.g. Warfarin, New Generation Drugs): Slow down the blood clotting mechanism.
- Diuretics: Relieve the burden on the heart by removing excess salt and water from the body.
- Nitrates: It is used to relieve attacks of chest pain (angina).
What is Angioplasty and Stenting, a Heart Disease Treatment to Open Blocked Arteries?
When stenoses in the coronary vessels reach a critical level, interventional methods are used to restore blood flow. Angioplasty and stenting is the most common and effective procedure in this field. It is called “minimally invasive” because it does not require a large surgical incision.
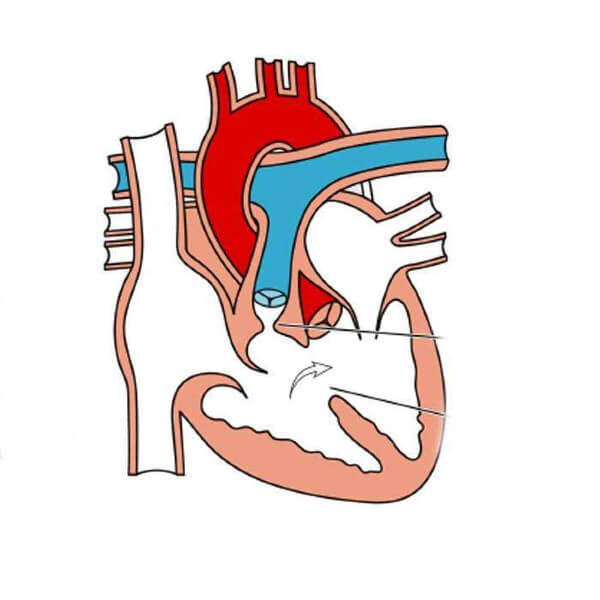
In this procedure, a catheter is inserted into the blocked vessel, as in angiography. A deflated balloon at the tip of the catheter is inflated at the site of the stenosis. This inflation crushes the plaque blocking the vessel against the vessel wall and widens the bloodway. Usually immediately after this procedure, a small wire mesh tube called a “stent” is placed in the same area to prevent the vessel from narrowing again. The stent acts as a scaffold that supports the vessel from the inside, keeping it open. This method can be life-saving by quickly opening the blocked vessel, especially in the event of a heart attack.
How is Bypass Surgery, a Heart Disease Treatment for Severely Blocked Arteries, Performed?
Sometimes the stenoses in the arteries may be widespread, numerous or unsuitable for stenting. In such cases, “coronary artery bypass surgery” offers the most effective and permanent solution. We can liken this surgery to opening a new side road, an alternative to a traffic-clogged highway.
In the operation, a healthy piece of blood vessel from another part of the body (usually from the chest wall or leg) is sewn to the part of the blocked coronary artery after the blockage. The blood then “bypasses” the blocked area, i.e. goes around it, and reaches the heart muscle through the newly opened vessel. Bypass surgery is an extremely safe procedure with excellent long-term results, especially for patients with diabetes with multiple blocked arteries or severe stenosis of the main arteries of the heart.
What does valve surgery for deteriorating valves as a treatment for heart disease?
Mechanical malfunctions of the heart valves cannot be corrected with medication. When the disease progresses and starts to impair the heart’s function, surgical intervention becomes inevitable. The main surgical approach is to repair or replace the valve.
Whenever possible, the first choice is to repair the patient’s own valve. Valve repair offers important advantages, such as a lower risk of infection and usually eliminates the need for lifelong blood thinners. However, if the structure of the valve has deteriorated too much due to calcification or infection, repair is not possible and valve replacement is required. There are two main options for cover replacement:
- Mechanical Covers: They are extremely durable and last a lifetime. However, in order to prevent clot formation on their surface, the patient must take blood thinners for life.
- Biological Valves: They are usually made from bovine or porcine heart tissue. They do not require blood thinners but may wear out over time (usually in 10-20 years) and require re-operation.
The appropriate valve type and surgical method (open, minimally invasive or non-surgical methods such as TAVI through the groin) are decided by evaluating many factors such as the patient’s age, general condition and lifestyle.
Frequently Asked Questions
What is heart disease?
Any disorder that affects the structure, function or blood vessels of the heart is called heart disease. These diseases can be life-threatening.
What are the most common types of heart disease?
Coronary artery disease, heart failure, rhythm disorders (arrhythmia), valvular diseases and congenital heart diseases are the most common.
What are the symptoms of heart disease?
Chest pain, shortness of breath, palpitations, fatigue, dizziness, bruising, edema and fainting are among the most common symptoms.
Do women have different symptoms of heart disease?
Symptoms. In women, atypical symptoms such as nausea, back pain, weakness and emotional breakdown may predominate.
Is heart disease genetic?
Yes, family history is an important risk factor for many heart diseases. But lifestyle also plays a big role.
Who is more prone to heart disease?
Smokers, people with hypertension, diabetes and high cholesterol, sedentary individuals and those who lead stressful lives are more at risk.
How is heart disease diagnosed?
The diagnosis is made with tests such as ECG, exercise test, echocardiography, blood tests (troponin), rhythm holter and coronary angiography.
Can heart disease be prevented?
Yes, it can be prevented. It can be prevented with a healthy diet, regular exercise, quitting smoking and alcohol, and controlling blood pressure and cholesterol.
Are heart attack and heart disease the same thing?
Answer. A heart attack (myocardial infarction) is a heart disease and is a consequence of coronary artery disease.
Can children get heart disease too?
Yes, it is possible. Especially congenital heart diseases can be seen in children. These are congenital defects in heart structures.
Is heart disease fatal?
Yes, it is one of the most common causes of death in the world. However, early diagnosis and treatment can prolong life.
What medicines are used in heart disease?
Blood pressure regulators, blood thinners, beta-blockers, statins, rhythm regulators and diuretics are the most commonly used drugs.
Is surgery necessary for all heart disease?
No, it is not. Many heart diseases can be controlled with medication and lifestyle changes. If necessary, stenting or surgery is considered.
Can heart patients play sports?
Appropriate exercise can be done with a doctor’s approval. However, intense and uncontrolled physical activity can be risky.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.