Pulmonary embolism, commonly known as pulmonary embolism, is when a blood clot, which usually forms in the deep veins of the legs, breaks loose and travels through the bloodstream to block the pulmonary arteries. This is a serious blood vessel blockage that requires urgent medical attention. the term “embolus” refers to a substance that travels through the bloodstream and blocks a blood vessel; in pulmonary embolism, this substance is most often a blood clot. This blockage makes it difficult for the heart to pump and can prevent the body from getting enough oxygen, which can suddenly endanger vital functions.
| Types | Massive Pulmonary Embolism, Sub-Massive Embolism, Non-Massive (small) Embolism |
| Causes | Deep vein thrombosis (DVT), clot formation after prolonged immobility, trauma, surgery |
| Risk Factors | Prolonged bed rest, cancer, birth control pills, obesity, pregnancy, genetic factors |
| Symptoms | Sudden shortness of breath, chest pain, rapid breathing, palpitations, fainting, bruising |
| Diagnostic Methods | CT pulmonary angiography, D-dimer test, lung scintigraphy, echocardiography, Doppler USG |
| Treatment Options | Anticoagulant drugs (heparin, warfarin, DOACs), thrombolytic therapy, surgical embolectomy, filter placement (IVC) |
| Complications | Right heart failure, pulmonary hypertension, recurrent embolism, sudden death |
| Protective Measures | Prevention of prolonged immobilization, use of compression stockings, low dose anticoagulant prophylaxis |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What Conditions Increase the Risk of Pulmonary Embolism?
Pulmonary embolism does not usually occur by chance. Usually when there is a slowing of blood flow, an increase in the tendency of blood to clot or damage to the vessel wall, there is a “perfect storm” for clot formation. Certain conditions and habits that can cause your body to work like a clot factory can significantly increase the risk of pulmonary embolism. Knowing these risk factors makes you more alert and prepared for a potential danger.
The main conditions that predispose to clot formation are as follows:
- Prolonged inactivity
- Major surgeries (especially hip and knee replacement)
- Cancer disease and treatments
- Pregnancy and the first six weeks after delivery
- Inherited (genetic) coagulation disorders
- Heart failure
- Obesity (being overweight)
- Cigarette smoking
- Advanced age (60 years and older)
- Estrogen-containing hormone therapies
- History of deep vein thrombosis or pulmonary embolism
- Serious injuries and trauma
When you look at this list, you can see that many factors play a role, which can occur at different stages of life and under different conditions. For example, being immobile for hours during a long airplane ride slows down blood flow in the leg veins, creating an ideal environment for clots. Similarly, a patient undergoing major surgery is at increased risk, both from the surgery itself and from bed rest afterward. Cancer can trigger the clotting system both by the disease itself and by treatments such as chemotherapy. Sometimes a pulmonary embolism of unknown cause can even be the first harbinger of a cancer hidden in the body. It is therefore particularly important to investigate such underlying risk factors in people who suffer from clots for no apparent reason.
Which Symptoms Should Suggest Pulmonary Embolism?
The symptoms of pulmonary embolism can vary greatly from person to person, depending on the size of the clot and the importance of the location in the lung that it blocks. Sometimes a very small clot can be dissolved by the body without any symptoms, while sometimes a large clot can be life-threatening within seconds. Recognizing these symptoms is vital for early intervention. You should be alert to these “emergency” signals your body sends.
The most common symptoms that strongly suggest the possibility of pulmonary embolism are:
- Sudden onset and unexplained shortness of breath
- Stabbing sharp chest pain when breathing deeply, coughing or bending over
- Coughing up blood or pink foamy sputum
- Very fast or irregular heartbeat (palpitations)
- Fainting, feeling lightheaded or severe dizziness
- An intense anxiety or fear of death that arises for no reason
- Cold and damp sweating
- Pallor or bruising of the skin (cyanosis)
Remember that pulmonary embolism is usually a consequence and the main event starts in the legs. Therefore, in addition to the above lung symptoms, the following symptoms may also be seen in the legs, which are the source of the clot:
- Swelling that usually occurs in one leg
- Pain, cramping or tenderness in the calf or thigh
- A different redness or discoloration of the skin in the affected area than usual
- A significant increase in temperature in the affected leg compared to the other
If you experience any of these symptoms, especially sudden onset of shortness of breath, chest pain and fainting, you should never take it lightly. thinking “it will pass if I rest a little” may mean wasting time, which is the most valuable thing to lose. It is critically important that you seek medical attention immediately by calling 112 or contacting the emergency department of the nearest hospital.
Which methods are used to diagnose pulmonary embolism?
When you go to the emergency room with a suspected pulmonary embolism, doctors start working like a detective. The aim is to establish once and for all whether it is indeed a clot that is causing your symptoms. Because there are many other conditions that can cause similar symptoms, such as heart attack, pneumonia and panic attacks. To reach the correct diagnosis, the patient’s history, risk factors and physical examination findings are brought together and the pieces of this puzzle are put together with various tests.
There are main tests and imaging methods we use in the diagnostic process:
- D-dimer blood test
- Leg vein ultrasound (Doppler USG)
- Computed Tomography Pulmonary Angiography (CTPA)
- Ventilation/Perfusion (V/Q) scintigraphy
- Chest radiography (X-ray)
- Electrocardiogram (ECG)
- Echocardiography (ECHO)
The gold standard among these tests today is CT Pulmonary Angiography (BTPA). During this test, a special dye (contrast medium) is injected into a vein in your arm. As soon as it reaches your pulmonary arteries through your bloodstream, a quick computed tomography scan is performed. The result is a detailed three-dimensional map of your pulmonary arteries. This map allows the doctor to see clearly whether there is a clot inside the arteries and, if so, where and how big it is. Simpler tests such as chest X-rays and ECGs usually do not show the clot directly, but are used to rule out other heart and lung diseases that may cause similar symptoms. An ultrasound of the leg can significantly help the diagnosis by detecting DVT, which is the source of the problem.
Which Drugs are Used in Pulmonary Embolism Treatment?
Once the diagnosis of pulmonary embolism is confirmed, the goal of treatment is clear. To stop the existing clot from growing larger and further obstructing blood flow, to prevent new clots forming elsewhere in the body and to allow the body’s own mechanisms to dissolve the clot over time. The drugs used for this purpose form the backbone of treatment.
The blood thinners (anticoagulants) that form the basis of treatment are divided into different groups:
- Injectable heparins (in needle form)
- Low molecular weight heparins (DMAH)
- Warfarin (known by trade names such as Coumadin™)
- New generation oral anticoagulants (NNOAs)
Treatment usually starts in the hospital with a fast-acting blood thinner, such as heparin, which is administered by injection. This initial intervention aims to stop the clot from growing immediately. Afterwards, oral medication in pill form is used for long-term treatment. Warfarin is an effective drug that has been used for many years, but it has challenges such as adjusting the dose with regular blood tests (INR monitoring) and interactions with certain foods. New generation drugs (NNTs) are usually used in fixed doses, do not require routine blood monitoring and have fewer food interactions. For this reason, they are preferred more often today. The length of treatment (usually at least 3-6 months, sometimes for life) is determined by your doctor depending on the cause of the clot and your risk of recurrence.
Thrombolytic drugs, which are much more powerful and actively dissolve the clot, are only used in specific, life-threatening situations:
- Persistent and severe low blood pressure (hypotension)
- Shock picture of circulatory system collapse
- Echocardiographic evidence of severe insufficiency on the right side of the heart
These drugs break up the clot like dynamite, but they also carry the risk of serious bleeding elsewhere in the body. Their use therefore requires a very careful risk-benefit assessment and is only administered under intensive care conditions by an experienced team.
What are Advanced Pulmonary Embolism Treatments?
In some patients, the situation is more complicated. The clot is so large that it can cause the heart to fail, or there is a critical situation where clot-dissolving drugs cannot be used because of the risk of bleeding. At such moments, advanced methods that go beyond standard drug therapies and aim to directly intervene in the clot come into play. These methods are sensitive interventions that fall within the specialty of a Cardiovascular Surgeon, combining technology and experience.
These interventional and surgical treatments are considered especially in cases of “submassive” and “massive” embolism, where the clot burden is high and the patient’s hemodynamic status (blood pressure, circulation) is impaired or at risk of impairment.
Catheter-directed therapies: This is a minimally invasive procedure similar to angiography. A thin catheter is inserted through a vein in the groin or neck and, under X-ray guidance, reaches the heart of the clot in the lung. The interventions that can be done in this method are as follows:
- Giving a very low dose of clot dissolving medication directly on the clot
- Breaking up the clot with sound waves using a catheter that emits special ultrasound waves
- Physically breaking up the clot with a rotating mechanical device
- Suctioning out the clot with a kind of vacuum system
- The aim of these methods is to quickly restore blood flow without the need for open surgery, with less risk.
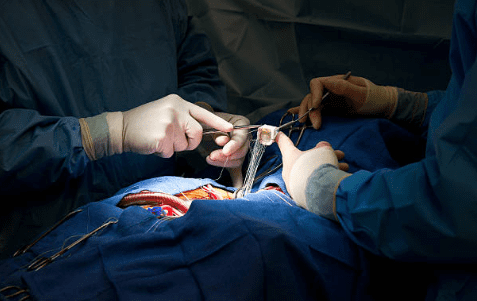
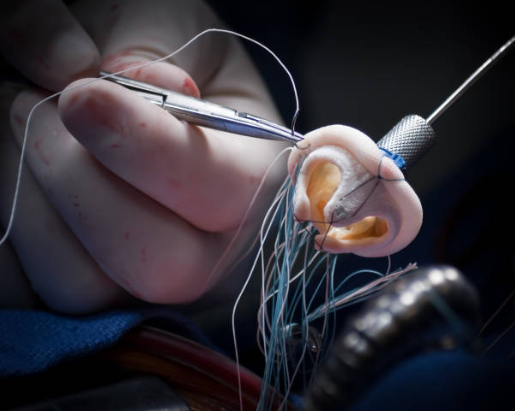
Surgical Embolectomy: This is an open-heart surgery that is reserved for the largest and most dangerous clots. In this procedure, the surgeon opens the chest, connects the patient to a heart-lung machine and temporarily stops the heart. In this bloodless and immobilized environment, the surgeon opens the pulmonary artery and visually and meticulously removes the clot. Surgical embolectomy becomes a life-saving option when
- Cases of massive embolism in which clot dissolving therapy is inadvisable due to the high risk of bleeding
- Failure of the applied clot dissolving treatment
- The presence of the clot inside the right chambers of the heart in addition to the pulmonary vessels
Although this surgery is a major intervention, when performed at the right time and by an experienced surgical team, it has the highest potential to rapidly heal the patient and prevent permanent damage.
Which Complications May Develop After Pulmonary Embolism?
Even in patients who successfully survive an episode of acute pulmonary embolism, the story does not always have a happy ending. In some cases, the event can lead to long-term and serious consequences. Therefore, follow-up after treatment is very important. Despite early and correct treatment, there are serious complications that can occur in some patients:
- Chronic thromboembolic pulmonary hypertension (CTEPH)
- Right heart failure (cor pulmonale)
- Permanent damage to lung tissue (pulmonary infarction)
- Recurrent pulmonary embolisms
- Post-thrombotic syndrome (after DVT in the legs)
The most insidious and serious of these complications is CTEPH. In this condition, the clots in the lung vessels do not dissolve despite treatment. Over time, these old clots adhere to the vessel wall and form a hard, scar tissue-like layer. This layer permanently narrows and blocks the blood vessels. As a result, the blood pressure in the lungs becomes chronically high (pulmonary hypertension). This means that the right side of the heart has to constantly pump blood against a high pressure. Over time, this overload causes the right heart to fatigue, enlarge and eventually fail (right heart failure). If your shortness of breath on exertion persists or increases months after treatment, CTEPH should be suspected. The diagnosis and surgical treatment of CTEPH, especially the special surgical treatment called “Pulmonary Thromboendarterectomy (PTE)”, is performed under the management of Cardiovascular Surgery Specialists specialized in this field.
What can be done to prevent recurrence of pulmonary embolism?
Once you have had a pulmonary embolism, one of the biggest goals is to never have this experience again. This is a process that requires more than just taking medication, it is a process in which you need to take an active role. Some lifestyle changes and precautions can significantly reduce the risk of clots.
There are some important steps you can take to reduce the risk of clots and live a healthier life:
- Taking the prescribed blood thinners regularly and without interruption
- Staying as active as possible during the day, taking regular walks
- Getting up and walking around every hour on long car or plane rides
- Doing exercises that work the ankles and legs while sitting
- Maintaining ideal weight by eating a healthy and balanced diet
- If you are a smoker, quit smoking once and for all
- Drink plenty of water during the day to keep the body hydrated
- Keeping the follow-up and control appointments recommended by your doctor
These steps are golden rules to protect not only the clot, but also your overall cardiovascular health. Pulmonary embolism is undoubtedly a serious and potentially life-threatening condition. However, it is also a preventable and treatable disease. Listening to your body’s signals, being proactive by knowing your risk factors and seeking specialized medical help without hesitation in suspicious situations are your most powerful weapons in this fight. In this process, a trusting partnership between patient, physician and healthcare team is key to achieving the best outcomes.
After Pulmonary Embolism Surgery
| Type of Surgery | Open surgical pulmonary embolectomy or endovascular intervention (catheter-assisted embolus removal). |
| Recovery Time | Average 4-8 weeks; depends on the general condition of the patient, the size of the embolus and the method of surgery. |
| Physical Activity | Light mobilization is recommended from the first days; immobility increases the risk of new emboli. |
| Medication Use | Long-term anticoagulant therapy (warfarin, DOACs, etc.) is required after surgery. In addition, oxygen support and, if necessary, supportive cardiac medications are given. |
| Radiologic and Clinical Monitoring | Pulmonary pressures and right heart function are monitored by CT angiography and echocardiography. |
| Complications | There are risks such as re-embolism, bleeding, pulmonary hypertension, right heart failure, infection, rhythm disturbances. |
| Wound and Catheter Site Care | The surgical incision or catheter entry site should be monitored for infection. |
| Respiratory Support | Oxygen therapy, deep breathing exercises and the use of a spirometer are recommended. |
| Nutrition | Foods that may interact with blood thinners (especially those containing vitamin K) should be avoided. |
| Smoking and Alcohol | Strongly discouraged; increases risk for vascular health and clots. |
| Sexual Activity | It is usually possible after 3-4 weeks, when the physical condition improves. |
| Psychological Support | Stress, anxiety may be common after a sudden life-threatening event; counseling is recommended. |
| Vehicle Use | Usually after 2-4 weeks, when the level of consciousness, reflexes and oxygenation becomes appropriate. |
| Controls | Frequent in the first 3 months; thereafter hematology/cardiology follow-up should be continued according to the duration of anticoagulant therapy. |
Frequently Asked Questions
Is there a risk of death from pulmonary embolism?
Yes, pulmonary embolism is a serious condition that can be life-threatening. The risk increases if a large clot blocks the main arteries or if treatment is delayed. However, thanks to modern diagnostic and therapeutic methods, this risk is greatly reduced if it is treated early and treated correctly. When suspected, it is vital to go to hospital immediately.
How many days does pulmonary embolism last?
The clot appears suddenly, but treatment can take weeks to months. Blood thinners usually last at least 3-6 months, in some cases for life. It takes time for the clot to dissolve and be cleared by the body.
Does a pulmonary embolism leave permanent damage?
In most patients, the clot dissolves completely and the lungs return to normal and no permanent damage occurs. However, in cases of very large clots or delayed treatment, problems such as persistent high pulmonary arterial pressure (pulmonary hypertension) can develop. Effective treatment minimizes this risk.
Does a pulmonary embolism heal completely?
Absolutely yes, the vast majority of patients recover completely and return to a normal life. Treatment dissolves the clot and prevents new clots from forming. Compliance with medication and lifestyle recommendations is key to success.
What are the risk factors for pulmonary embolism?
The main risk factors are prolonged immobility (major surgeries, long journeys), cancer, genetic clotting disorders, pregnancy, birth control pills, smoking. The risk is increased in people with more than one risk factor.
Can pulmonary embolism show up on X-ray?
The clot itself is usually not visible on a standard chest X-ray, but it is useful to exclude other diseases. CT scan and angiography are necessary for definitive diagnosis.
Which doctor treats pulmonary embolism?
The initial diagnosis is usually made in the Emergency Department. Treatment and follow-up is carried out by Pulmonology and Cardiology specialists. In rare cases, Cardiovascular Surgery may be involved to remove the clot.
How is pulmonary embolism diagnosed?
First, complaints and risk factors are evaluated. Blood tests such as D-dimer provide clues, while the definitive diagnosis is made by Computed Tomography Pulmonary Angiography.
Can clots form while taking blood thinners?
Although very rare, it is possible. If the dose of medication is not sufficient or if there is a strong risk factor (e.g. active cancer), the clot may form again. For this reason, it is very important to keep up with your medication and have regular medical check-ups.
What should people with pulmonary embolism pay attention to?
Take full blood thinners, have regular check-ups and be aware of the risk of bleeding. Avoid prolonged immobilization and always consult your doctor before any planned procedures.
What should embolism patients not eat?
Warfarin (Coumadin) users should pay attention to vitamin K-rich foods (such as spinach, kale, broccoli) and keep their daily intake in balance. New generation blood thinners usually do not require any special dietary restrictions.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Heart diseases are conditions that impair the structure and function of the heart, leading to [...]
Aug
How the Heart Works
The heart functions as a muscular pump that circulates blood throughout the body. It consists [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Heart valve surgery duration varies depending on the complexity of the case and the valve [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Coronary bypass surgery duration depends on the number of blocked arteries and patient-specific factors. On [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Kalp kapakçığı değişimi, kapakların ileri derecede daralması (stenoz) veya yetersiz kapanması (yetmezlik) durumlarında, onarımın mümkün [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Kalp kapakçığı tamiri, mevcut kapağın korunarak yapısal bozukluklarının düzeltilmesi işlemidir. Kapak yaprakçıkları, kordonları veya halka [...]
Aug
Life After Heart Valve Surgery
Life after heart valve surgery involves a structured recovery period, with gradual improvement in physical [...]
Aug
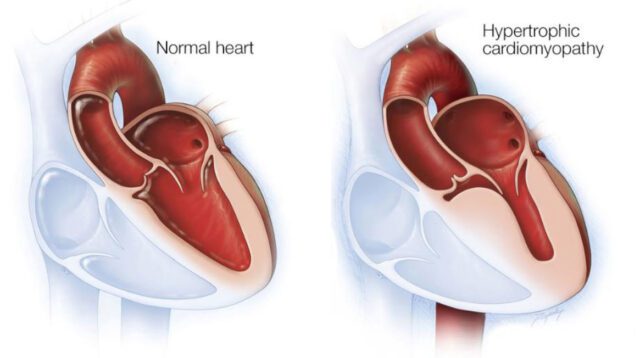
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, [...]
Aug