Venous insufficiency is a circulatory disorder in which the veins in the legs are unable to effectively pump blood back to the heart. The main symptoms of this condition, also known as chronic venous insufficiency, include pain in the legs, swelling that increases at the end of the day, a feeling of heaviness, night cramps and visible varicose veins. The underlying cause of this problem, which seriously affects quality of life, is usually dysfunction of the vein valves. Today, venous insufficiency treatment offers effective and permanent solutions by targeting this underlying problem with modern and minimally invasive methods.
| Types | Chronic Venous Insufficiency (CVI), Acute Venous Insufficiency, Deep Venous Insufficiency, Superficial Venous Insufficiency |
| Causes | Venous valve insufficiency, deep vein thrombosis (DVT), vein wall weakness, previous venous thrombosis |
| Risk Factors | Prolonged standing, inactivity, obesity, pregnancy, advanced age, family history, female gender |
| Symptoms | Swelling, pain, feeling of heaviness, varicose veins, skin discoloration, ulcers around the ankle |
| Diagnostic Methods | Doppler ultrasonography, physical examination, venography (rare), plethysmography |
| Treatment Options | Lifestyle changes (exercise, leg elevation), compression stockings, sclerotherapy, laser therapy, surgery (stripping, endovenous ablation) |
| Complications | Venous ulcers, skin infections (cellulitis), thrombophlebitis, chronic leg pain and swelling |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What Causes Venous Insufficiency?
To understand the underlying mechanism of venous insufficiency, we can think of our leg veins as an intelligent plumbing system. The job of this plumbing is to move blood from the bottom to the top, in the opposite direction to gravity. For this challenging task, nature has placed wonderful valves inside the veins that work in one direction. These valves open when the blood is flowing upwards and close immediately when the flow stops to prevent the blood from escaping backwards.
Venous insufficiency begins when these valves fail or when the vein wall expands and prevents the valves from making contact with each other. Because of the malfunctioning valves, blood escapes backwards (this is called “reflux” in medicine) and pools in the lower legs. This increases the pressure inside the blood vessel, just as the pressure inside a garden hose increases when the end is squeezed. Over time, this increased pressure causes more vessels to dilate and more valves to fail, creating a vicious cycle.
So what disrupts these valves? There are some main causes that predispose to the development of venous insufficiency. Some of these are:
- History of Deep Vein Thrombosis (DVT)
- Genetic predisposition (family history of varicose veins)
- Congenital vascular structure disorders
- Advanced age
- Previous leg trauma or surgery
- Superficial vein inflammation (phlebitis)
- Vascular compression such as May-Thurner Syndrome
When one or more of these factors come together, the delicate balance in our vascular system can be disturbed and the disease process can begin.
What are the Symptoms of Venous Insufficiency Disease?
[dk_youtube_shortcode url=”https://www.youtube.com/watch?v=1qDrTQebDOc”]Venous insufficiency does not always manifest itself with large, purple varicose veins. Sometimes it starts with much more insidious and seemingly simple complaints. Recognizing these symptoms early is the most important step to prevent the disease from progressing. In order to correctly read the signals your body is sending you, you should pay attention to the following symptoms.
Common complaints usually include the following:
- Pain (aching, throbbing or burning)
- Feeling of heaviness and fullness
- Fatigue
- Swelling (especially at the end of the day)
- Night cramps
- Itching
- Restlessness and constant desire to move the legs
- Numbness or tingling
In addition to these sensations, there may also be some visible changes in your legs. These visible signs are usually the following:
- Spider web of fine capillaries
- Varicose veins that bulge from the skin
- Discoloration of the ankle (red-brown appearance)
- Dryness and flaking of the skin (varicose eczema)
- Hardening and thickening of the skin
- Non-healing or recurrent wounds (venous ulcers)
If you are experiencing one or more of these symptoms, it is critical to not accept it as “normal” and to consult a specialist to protect your quality of life.
What are the Risk Factors for Venous Insufficiency Disease?
Some people are more prone to venous insufficiency disease due to their lifestyle or genetic heritage. Knowing these risk factors can help you be proactive and take the necessary precautions. We can divide these factors into two main groups: what we cannot control and what we can change with our lifestyle.
Risk factors that are beyond our control and cannot be changed are:
- Family history (genetic inheritance)
- Advanced age (over 50 years)
- Female gender
- Previous deep vein thrombosis (DVT)
- Congenital vascular anomalies
Fortunately, there are also risk factors that we can influence or manage through lifestyle changes. The most important of these are as follows:
- Overweight (obesity)
- Pregnancy (especially multiple pregnancies)
- Standing for long periods of time
- Sitting for a long time
- Living a sedentary life
- Cigarette smoking
- Preferring tight and tight clothing
- Wearing high-heeled shoes
How Does the Diagnosis Process of Venous Insufficiency Disease Progress?
The first and most important step to effective treatment is an accurate and complete diagnosis. Venous insufficiency is diagnosed through a process that involves several simple and painless steps. This process is designed to address the patient’s concerns and chart the best course of treatment.
The diagnostic process is usually led by a cardiovascular surgeon and consists of three main stages. The first involves a detailed conversation with you. Information is gathered about your symptoms, how long they have been present, your family history and your lifestyle. The second is a simple standing physical examination. This examination evaluates visible veins, swelling or skin changes in the legs.
The third and most critical stage is “Color Doppler Ultrasonography”. This is the gold standard of diagnosis. This test uses sound waves to create a map of your leg veins. Like a road map, it clearly shows in which vessels the blood flows in the right direction, in which vessels it flows backwards (reflux) and whether there are any clots or blockages in the vessels. The procedure is completely painless, radiation-free and takes about 20-30 minutes. This detailed information enables the most appropriate and effective treatment method to be selected for you.
What Problems Does Untreated Venous Insufficiency Cause?
Unfortunately, venous insufficiency is not a condition that gets better on its own over time. On the contrary, when left untreated, it follows a progressive course and can cause complications that seriously reduce quality of life and can even be dangerous. At this point, one of the questions that patients are most curious about is “can venous insufficiency kill?”. This question requires a clear answer: Venous insufficiency is not a directly fatal disease. However, some serious complications can be life-threatening.
The main problems that untreated disease can cause in the future are as follows:
Chronic Pain and Swelling: It is one of the most basic consequences of the disease. Over time, these complaints become permanent and make it difficult for the person to walk, work, in short, to maintain their daily life.
Permanent Skin Changes: Due to the increased pressure, the skin around the ankle becomes darker in color, hard, dry and itchy (stasis dermatitis or lipodermatosclerosis). This makes the skin vulnerable and open to infections.
Venous Ulcer (Varicose Wound): It is the most advanced and troublesome stage of the disease. They are painful wounds on the inside of the ankle that open spontaneously or with minor trauma, heal very difficult and recur constantly. These wounds can take over a person’s life.
Superficial Thrombophlebitis It is the formation and inflammation of a clot inside varicose veins. This condition is characterized by a sudden redness, stiffness and severe pain in the leg.
Deep Vein Thrombosis (DVT): This is the most dangerous complication. Blood pooling in the superficial veins increases the risk of clots forming in the deeper main veins. DVT not only causes pain and swelling in the leg, but also carries the risk of the clot breaking off and traveling to the lungs (pulmonary embolism). Pulmonary embolism is a serious and life-threatening condition that requires urgent intervention.
Bleeding Especially thinned varicose veins close to the skin can bleed easily with a small impact. This bleeding can sometimes be difficult to stop.
What Treatment Methods Are Available for Venous Insufficiency?
Today’s medicine offers revolutionary advances in the treatment of venous insufficiency. This problem is no longer the fearful dream of patients, but has become a manageable condition with comfortable and effective methods. The answer to the question “Is there a definitive solution to venous insufficiency?”, which patients are most curious about, is hidden in the high success of modern treatment approaches. When the underlying problematic vein is eliminated with the right method, the symptoms disappear permanently and this means a “definitive solution” for patients. Treatment is planned individually according to the stage of the disease and the patient’s condition.
- Basic Steps Lifestyle Changes and Conservative Treatments
- These methods form the basis of each patient’s treatment plan and are often necessary to improve the success of other treatments.
- Compression Stockings: These special stockings promote blood circulation by applying controlled pressure to the legs from the outside. They are extremely effective in reducing swelling and pain.
- Exercise: Activities that work the calf muscles, such as regular walking, help pump blood back to the heart.
- Weight Control: Extra pounds put extra strain on your leg veins. Being at a healthy weight eases this burden.
- Elevating the Legs: Raising the legs above the level of the heart whenever you have the opportunity during the day provides instant relief.
- Medications: Some medications that strengthen the vascular wall and reduce edema can be used to relieve symptoms.
- Modern and Comfortable Approaches: Minimally Invasive (non-surgical) Treatments
- These are extremely comfortable and effective methods that form the backbone of venous insufficiency treatment today, do not require hospitalization, and are performed under local anesthesia.
- Endovenous Laser Ablation (EVLA): A thin laser wire is inserted into the problematic vein under ultrasound guidance and the vein is closed from the inside.
- Radiofrequency Ablation (RFA): It works in a similar way to laser, but uses radiofrequency energy as the heat source.
- Medical Adhesive (VenaSeal / Bioadhesive): One of the newest and most comfortable methods. A special medical adhesive is injected into the vein and the vein is closed instantly. It is usually not even necessary to wear socks after the procedure.
- Sclerotherapy (Foam Therapy): It is the process of drying smaller varicose veins or capillaries by injecting a special drug into them.
- In Necessary Cases Surgical Treatments
With the widespread use of modern methods, classical varicose vein surgeries (ligation and stripping) are less and less needed. However, they may still be an option in some special and advanced cases. For blockages in deep veins, a procedure called “venous stenting”, in which the blocked vein is opened with a stent, can be life-saving.
How to Personalize Venous Insufficiency Disease Treatment?
With so many treatment options available, how do you decide which one is right for you? The answer lies in the “personalized treatment” approach. The information you read on the internet or a friend’s experience may give you an idea, but only a cardiovascular surgeon who examines you and examines your Doppler ultrasound results in detail can make the best decision.
Many factors are taken into account when creating your treatment plan. Some of these are as follows:
- Stage of your disease (CEAP classification)
- The severity of your symptoms and their impact on your quality of life
- In which vein the problem is located (superficial or deep)
- The diameter of your vein and whether it is tortuous
- Reflux, i.e. the degree of valve leakage
- Your general health and age
- Your expectations from the treatment
For example, sclerotherapy may be sufficient for a patient with a capillary complaint for aesthetic purposes only, while a patient with a serious leak in the main vein and scars on the legs may require more effective methods such as laser (EVLA) or medical adhesive (VenaSeal). Your doctor will discuss all these factors with you, explain the advantages and disadvantages of each option and draw the most appropriate treatment roadmap for you.
What Can You Do to Prevent the Progression of Venous Insufficiency Disease?
Whether you have been treated or are simply at risk, there are many simple but effective steps you can take to maintain your leg health and slow the progression of the disease. When these steps become a lifestyle, they can both alleviate your current symptoms and help prevent future problems. Remember that your legs carry you for life, it is up to you to take good care of them.
Here are some suggestions that you can easily incorporate into your daily life:
Move, Don’t Stay Still: Avoid staying in the same position for long periods of time. If you work in an office, get up and take a short walk every hour. Even simple ankle exercises stimulate blood circulation. Make it a habit to take regular daily walks.
Watch Your Weight: Every extra pound is an extra burden on your legs. Try to maintain your ideal weight.
Rest Your Legs: In the evening, while watching TV or reading a book, place a pillow under your legs and elevate them above heart level. This simple movement helps to drain the blood that has accumulated throughout the day.
Choose the Right Shoes and Clothes: Tight pants, belts and high-heeled shoes that squeeze your body negatively affect blood circulation. Choose comfortable, loose-fitting clothes and low-heeled shoes.
Take Care of Your Table (Venous Insufficiency and Nutrition): Your eating habits also affect your vascular health. You should pay particular attention to the following:
- Reduce salt (excess salt increases swelling by retaining water in the body).
- Drink plenty of water.
- Eat fibrous foods (prevent constipation and lower intra-abdominal pressure).
- Avoid processed foods and packaged products.
Eliminate Smoking from Your Life: Smoking is one of the biggest enemies of your entire vascular system.
After Venous Insufficiency Surgery
| Recovery Time | 2-6 weeks; depends on the method used and the individual healing process. |
| Physical Activity | Walking is recommended in the early period; prolonged standing or sitting should be avoided. |
| Compression Socks | Recommended for 2-4 weeks after surgery; promotes venous return, reduces swelling and bruising. |
| Medication Use | Analgesics, anti-inflammatories if necessary; short-term anticoagulant therapy may be given in some patients. |
| Wound Care | Incision sites should be checked regularly; signs of infection (redness, increased temperature, discharge) should be monitored. |
| Complications | Hematoma, bruising, nerve damage, infection, skin discoloration, rarely deep vein thrombosis. |
| Leg Position | During rest, the legs should be kept above the level of the heart; this reduces edema. |
| Nutrition | A low-salt, balanced diet is recommended, which has a positive effect on edema and circulation. |
| Smoking and Alcohol | Smoking should be stopped; alcohol consumption should be limited. |
| Sexual Activity | It is usually possible within 1-2 weeks, after the pain and tenderness have subsided. |
| Psychological Support | An increase in quality of life is expected with relief from chronic leg disorders; support can be offered to patients experiencing anxiety. |
| Vehicle Use | If the general condition is good and there is no severe pain in the legs, it can usually be started within 2-3 days. |
| Controls | Surgical control is performed in the first 1-2 weeks, followed by vascular patency and reflux control with Doppler ultrasound at 1-3 month intervals. |
Frequently Asked Questions
Does venous insufficiency heal?
Venous insufficiency cannot be completely reversed, but with modern treatments and lifestyle changes, your symptoms can be eliminated, the progression of the disease can be stopped and your quality of life can return to its previous level. Although it cannot be completely eliminated, it is possible to have a healthy and comfortable life.
Is venous insufficiency dangerous?
It is usually not directly life-threatening. However, if left untreated, it can seriously impair quality of life. Constant pain, cramps and swelling make daily life difficult. In advanced cases, non-healing wounds (venous ulcers) and rarely clot formation (thrombosis) may develop. Therefore, it must be kept under control.
Are venous insufficiency and varicose veins the same thing?
No, they are not the same. Venous insufficiency is when the valves in the veins fail to function. Varicose veins are the visible result of this condition; the veins become dilated and tortuous. All varicose veins are caused by venous insufficiency, but not all venous insufficiency may cause varicose veins.
Does venous insufficiency throw clots?
Venous insufficiency slightly increases the risk of thrombosis. As blood flow slows down, there is a favorable environment for clots. A clot (DVT), especially in the deep veins, can lead to serious problems if it is thrown into the lung. Compliance with recommendations and treatment is crucial to reduce this risk.
Does venous insufficiency affect sexuality?
Yes, it can. Venous insufficiency, especially in the pelvic area, can cause pain during or after intercourse in women and men. Pain, swelling and aesthetic concerns in the legs can also negatively affect sexual life and self-confidence. It is nothing to be ashamed of; it is largely solvable with treatment.
Which doctor treats venous insufficiency?
The department you should consult for venous insufficiency is Cardiovascular Surgery. Diagnosis, follow-up and treatment (medication, interventional methods or surgery) are performed by specialists in this field. If necessary, tests such as Doppler ultrasound are also performed.
What happens if I don't have venous insufficiency surgery?
If interventional treatment has been recommended, delaying it can exacerbate the problem. Complaints may increase, permanent discoloration and hardening of the skin may occur, and worst of all, non-healing, painful sores (venous ulcers) may develop on the ankle. Modern treatments are comfortable; it is best not to delay.
What should people with venous insufficiency do?
Be active, take walks, do not stand still for a long time. Stretch your feet while sitting, get rid of excess weight and use compression stockings regularly. These both stop the progression of the disease and reduce symptoms.
What is good for venous insufficiency herbal?
Horse chestnut extract (aescin), which has been partially scientifically shown to be effective, can strengthen the vascular wall and relieve edema and pain. However, this is not a medicine, it only relieves symptoms. Always consult a doctor before use and do not expect miracles.
How many mm should venous insufficiency be?
The diagnosis is based not on the diameter of the vein, but on how long the valves hold back the blood. If this time exceeds half a second (0.5 s) with Doppler ultrasound, it is called “venous insufficiency”. The diameter of the vessel is also important, but the main diagnostic criterion is the duration of the retraction.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Heart diseases are conditions that impair the structure and function of the heart, leading to [...]
Aug
How the Heart Works
The heart functions as a muscular pump that circulates blood throughout the body. It consists [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Heart valve surgery duration varies depending on the complexity of the case and the valve [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Coronary bypass surgery duration depends on the number of blocked arteries and patient-specific factors. On [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Kalp kapakçığı değişimi, kapakların ileri derecede daralması (stenoz) veya yetersiz kapanması (yetmezlik) durumlarında, onarımın mümkün [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Kalp kapakçığı tamiri, mevcut kapağın korunarak yapısal bozukluklarının düzeltilmesi işlemidir. Kapak yaprakçıkları, kordonları veya halka [...]
Aug
Life After Heart Valve Surgery
Life after heart valve surgery involves a structured recovery period, with gradual improvement in physical [...]
Aug
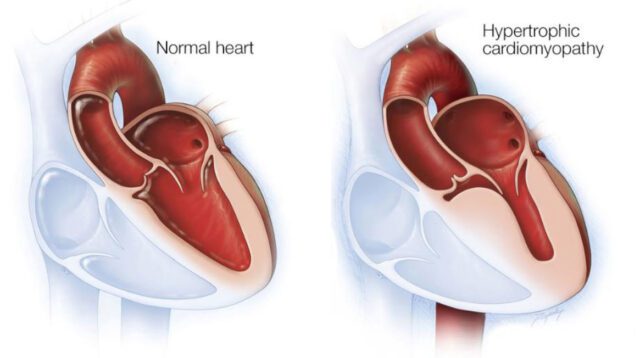
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, [...]
Aug