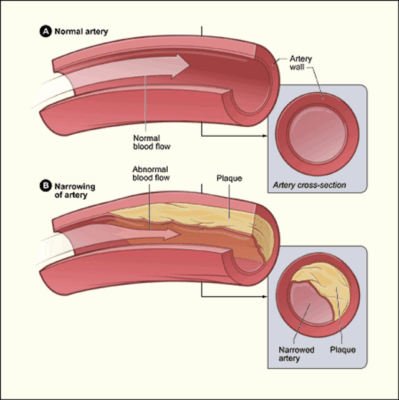
Atherosclerosis is a chronic condition characterized by the accumulation of lipids, cholesterol, and fibrous tissue within arterial walls, leading to plaque formation. This process narrows the arteries, reduces blood flow, and significantly increases the risk of cardiovascular diseases such as heart attack and stroke.
The causes of atherosclerosis include high cholesterol, smoking, diabetes, and hypertension. Over time, these risk factors contribute to endothelial damage, which accelerates plaque buildup. Early prevention through lifestyle modifications and medical follow-up is crucial to slow disease progression.
Symptoms of atherosclerosis often remain silent until advanced stages. Chest pain, shortness of breath, or leg pain during walking may indicate significant arterial obstruction. In severe cases, sudden vascular events like myocardial infarction or stroke may occur, requiring urgent medical intervention.
Treatment of atherosclerosis involves both lifestyle changes and pharmacological therapy. Statins, antihypertensives, and antiplatelet drugs play a central role in management. In advanced cases, surgical options such as angioplasty or bypass surgery may be required to restore blood flow and prevent life-threatening complications.
| Definition | Thickening, hardening and loss of elasticity of the arterial wall due to the accumulation of fat, cholesterol, calcium and other substances on the inner surface of the arteries |
| Causes | High cholesterol, hypertension, smoking, diabetes, obesity, sedentary lifestyle, genetic predisposition, unhealthy diet |
| Risk Factors | Advanced age, male gender, family history of cardiovascular disease, hypertension, high cholesterol, diabetes, smoking, obesity |
| Symptoms | In the early period, usually asymptomatic; in the later period, chest pain, pain in the legs, shortness of breath, dizziness, stroke, heart attack, loss of organ function |
| Diagnostic Methods | Blood tests (lipid profile), ECG, Doppler ultrasonography, CT-angiography, coronary angiography |
| Treatment Methods | Lifestyle changes, healthy diet, exercise, smoking cessation, cholesterol and blood pressure regulating drugs, antiplatelet therapy, stent or bypass surgery in advanced cases |
| Complications | Coronary artery disease, heart attack, stroke, peripheral artery disease, aneurysm, organ damage |
| Prevention Methods | Healthy and balanced diet, regular exercise, avoidance of smoking, control of blood pressure and cholesterol, good management of diabetes, regular medical check-ups |
What Is Atherosclerosis and How Does It Differ from Arteriosclerosis?
When we say “arteriosclerosis” in everyday speech, we usually mean atherosclerosis, but these two terms do not actually mean the same thing. Arteriosclerosis is a more general term meaning “hardening of the arteries”. The natural loss of some elasticity of the veins with age is also included in this definition.
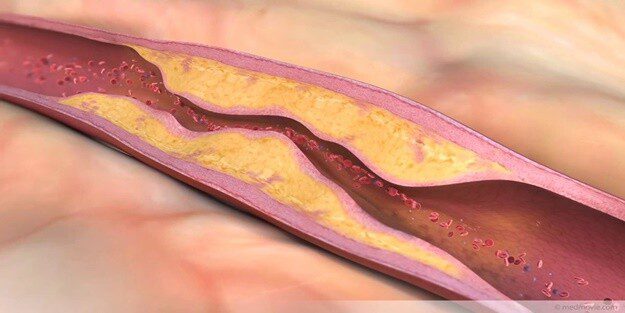
Atherosclerosis is the most common and dangerous type of hardening. In this condition, the vessel wall not only hardens, but deposits of fat, cholesterol, calcium and cellular waste, called “plaques”, form on its inner surface. These plaques grow over time, like a layer of lime in a water pipe, narrowing the inner diameter of the vessel and preventing blood from flowing freely. Therefore, all atherosclerosis is atherosclerosis, but not all atherosclerosis is atherosclerosis. The main problem that is important for us clinically and that we focus on treating is atherosclerosis caused by these plaques.
How and Why Do Atherosclerosis Plaques Form?
The formation of an atherosclerotic plaque is a much more complex story than a simple blockage of an artery. It is a process of inflammation that the body initiates in response to an injury, but which gets out of control over time. We can think of this process as a step-by-step movie strip.
It all starts with damage to the delicate single layer of cells called “endothelium” that lines the inside of our blood vessels and keeps the blood flowing smoothly. The main culprits are the constant pressure of high blood pressure on the blood vessel wall, the toxic chemicals in cigarette smoke, high blood sugar and too much “bad” cholesterol (LDL) in the bloodstream.
When the endothelium is damaged and its permeability increases, LDL cholesterol particles circulating in the blood seep through this crack and enter the vessel wall. The body’s defense system recognizes this as an invasion and sends scavenger cells called “macrophages” to the area. The macrophages begin to engulf the cholesterol that has infiltrated the vessel wall in order to clean it up. However, the amount of cholesterol is so high that after a while the macrophages fill up and turn into fat-filled, swollen cells called “foam cells”. The accumulation of these foam cells forms “fatty streaks”, the first visible step in atherosclerosis.
As the process progresses, the body calls in smooth muscle cells from the vessel wall to repair and control the damaged area. These cells weave a tough “fibrous cap” of substances such as collagen around the accumulated fatty core. The aim is to isolate this dangerous content from the blood stream. This structure – a fatty core and a hard shell surrounding it – becomes a mature atherosclerotic plaque.
The most dangerous scenario is when this plaque ruptures. If the inflammation inside the plaque continues, the fibrous cap that protects it can weaken and one day suddenly rupture. When the fatty and coagulation-inducing substances in the plaque come into contact with the blood, the body immediately forms a blood clot (thrombus) in the area. If the already narrowed blood vessel is completely blocked by this clot, the tissue that the blood vessel feeds cannot receive blood. If this happens in the heart, it causes a heart attack; if it happens in the brain, it causes a stroke.
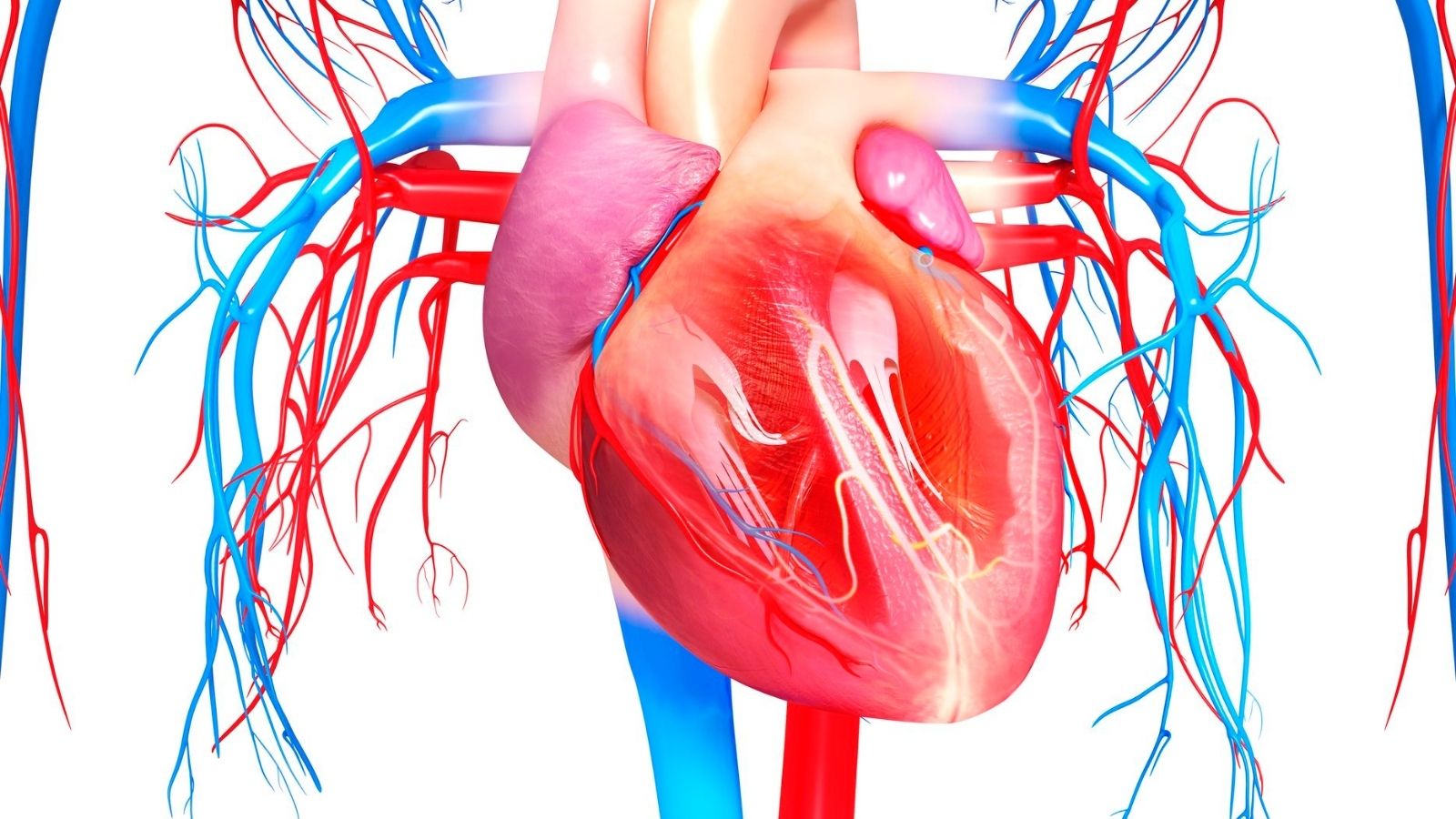
Which arteries in the body are affected by atherosclerosis?
Atherosclerosis is a systemic disease, meaning that it can affect highways in different parts of the body at the same time. The symptoms and the problems caused by the disease depend entirely on which artery is involved. The arteries where atherosclerosis is most commonly localized are:
- Coronary arteries (vessels that feed the heart)
- Carotid and vertebral arteries (carotid arteries supplying blood to the brain)
- Peripheral arteries (vessels that carry blood, usually to the legs, sometimes to the arms)
- Renal arteries (Kidney vessels)
- Aorta (main artery of the body)
- Mesenteric arteries (vessels supplying the intestines)
What Are the Non-Modifiable Risk Factors Leading to the Development of Atherosclerosis?
Some factors in the development of atherosclerosis are beyond our control. We cannot change them, but knowing they exist should be a warning sign to pay more attention to other factors that we can control. These risk factors are as follows:
- Advanced age
- Male gender (risk increases rapidly after menopause in women)
- Family history of early heart disease
- Genetic predisposition (conditions such as familial high cholesterol)
What Are the Controllable Factors That Increase the Risk of Atherosclerosis?
Our real power in the fight against atherosclerosis comes from managing the risk factors we can change. With healthy lifestyle choices and proper medical follow-up, it is possible to slow or even stop the progression of this disease. Here are our main enemies that accelerate the process of atherosclerosis and that we can intervene against:
- High levels of LDL (“bad”) cholesterol
- Low HDL (“good”) cholesterol levels
- High blood pressure (Hypertension)
- Smoking and use of other tobacco products
- Diabetes and insulin resistance
- Overweight and especially abdominal fat (obesity)
- Physical inactivity (sedentary life)
- Unhealthy eating habits
How Diabetes, Obesity and Inflammation Accelerate the Atherosclerosis Process
These three conditions form a “devil’s triangle” for atherosclerosis. They often coexist and multiply each other’s negative effects.
High blood sugar in diabetes is like poison for the endothelial cells in the lining of blood vessels. Sugar molecules adhere to proteins in the vessel wall, disrupting the vascular structure, hardening it and triggering inflammation.
Obesity, especially visceral fat around the waist, is not a passive fat storage. On the contrary, it is a highly metabolically active organ, constantly releasing inflammatory chemicals called “cytokines” into the bloodstream. It’s like having a constant, low-level fire in the body, and that fire is constantly damaging the vessel walls.
When these factors come together, we have what we call “Metabolic Syndrome”. A person with this syndrome is sitting on a ticking time bomb in terms of atherosclerosis and the associated risk of heart attack or stroke. Targeting a risk factor can actually have a positive effect on this harmful web. For example, just losing weight can improve blood pressure, blood sugar and cholesterol at the same time.
When Does Atherosclerosis Usually Start to Show Symptoms?
The most insidious aspect of atherosclerosis is that it progresses completely silently over many years. Until the plaque in an artery has narrowed it by p-80, there are usually no symptoms. Because at rest, the reduced blood flow may be enough to meet the organ’s needs.
Symptoms usually occur when the body needs more oxygen. For example, when climbing stairs, walking fast, playing sports or in times of intense stress, the narrowed blood vessel is unable to keep up with the increased demand and the organ it supplies begins to send distress signals. Unfortunately, for some people, the first symptom can be a heart attack or stroke. This is why it is so important to know the risk factors and have them checked without waiting for symptoms.
What Symptoms Occur When Atherosclerosis Affects the Heart Vessels?
When the coronary arteries that supply the heart narrow, the heart muscle does not get enough oxygen. The symptoms caused by this condition are usually the following:
- Feeling of pressure, tightness, burning or heaviness in the chest (angina pectoris)
- Chest pain radiating to the left arm, shoulder, back, jaw or neck
- Shortness of breath that comes with exertion and passes with rest
- Fatigue and weakness more quickly than usual
- In case of a heart attack, severe chest pain that does not go away with rest, cold sweats, nausea and fear of death
What Symptoms Occur When Atherosclerosis Affects the Arteries of the Brain, Legs and Kidneys?
The symptoms of atherosclerosis vary greatly depending on which organ’s highway is blocked.
Brain Vessels (Carotid Artery Disease): When carotid artery stenoses momentarily reduce blood flow to the brain, they cause warning symptoms called “Transient Ischemic Attack” (TIA). These symptoms can be a harbinger of an impending stroke. Symptoms of arteriosclerosis in the neck or signs of cerebral arteriosclerosis may include
- Sudden numbness, tingling or weakness in the face, arm or leg (usually on one side of the body)
- Sudden speech impairment (lisping, inability to find words)
- Sudden difficulty in understanding what is being said
- Sudden loss of vision or blurred vision in one or both eyes
- Facial slippage or sagging
- Sudden dizziness and loss of balance
Leg Veins (Peripheral Arterial Disease): The most common symptoms of arteriosclerosis in the legs occur when walking:
- Cramp-like pain when walking, especially in the calf, thigh or buttock muscles
- The pain goes away in a few minutes with rest (Showcase disease)
- Chills and coldness in the feet and legs
- Skin discoloration or bruising
- Loss of leg hair
- Slow growth and thickening of toenails
- Non-healing wounds (ulcers) on the feet or fingers in advanced stages
- Rest pain that occurs when lying down at night and is relieved when the leg is lowered
Renal Arteries (Renal Artery Stenosis): It is usually very insidious and asymptomatic for a long time:
- High blood pressure that occurs at a young age or is difficult to control
- “resistant” hypertension that cannot be reduced despite three or more medications
- Unexplained renal dysfunction
What Serious Complications Can Untreated Atherosclerosis Lead To?
When atherosclerosis is allowed to progress, the consequences can often be sudden and life-threatening. The main complications are:
- Heart attack (Myocardial infarction)
- Stroke (Paralysis)
- Aneurysm (ballooning of the vessel wall) and rupture (tearing)
- Critical leg ischemia and gangrene (limb loss, amputation)
- End-stage renal failure (need for dialysis)
- Sudden cardiac death
How is Atherosclerosis Diagnosed?
Diagnosing atherosclerosis is like putting the pieces of a puzzle together. The process starts with listening to the patient’s story and understanding their risk profile. Your complaints, lifestyle, habits and family history are the first and most important pieces of the puzzle. In the physical examination that follows, your blood pressure is measured and your pulses (especially those in the legs and feet) are checked. When the blood flow through a narrowed vessel is listened to with a stethoscope, an abnormal buzzing sound called a “murmur” can be heard. After these initial assessments, further tests are carried out to confirm suspicions and map the disease.
Which Blood Tests and Imaging Methods are Used in the Diagnosis of Atherosclerosis?
There are many modern technologies we use to confirm the diagnosis. These tests provide a wide range of information, from identifying risk factors to seeing inside the vein.
The main blood tests are:
- Lipid panel (LDL, HDL, Triglycerides)
- Fasting blood glucose and HbA1c
- High-sensitivity C-reactive protein (hs-CRP)
Imaging and functional tests include
- Electrocardiogram (ECG)
- Exertional ECG (Exercise stress test)
- Echocardiography (ECHO)
- Doppler Ultrasonography
- Computed Tomography (CT) Angiography
- Coronary Calcium Scoring
Doppler ultrasound provides quick and harmless information about stenoses by using sound waves to assess blood flow, especially in the veins of the neck and legs. CT angiography, on the other hand, uses a contrast medium injected intravenously to create a detailed, three-dimensional map of the vessels, clearly showing the location and structure of the plaques (soft, calcareous) and the degree of stenosis.
Why Angiography is Considered the Gold Standard in Atherosclerosis Diagnosis
Although all other tests give us valuable information, angiography gives us the clearest, most precise and detailed view of the inside of the arteries. Especially in coronary artery disease, angiography is considered the “gold standard” because it not only tells us what the problem is, but also opens the door to a solution.
During the procedure, a catheter, a thin, flexible tube, is inserted through an artery, usually in the wrist or groin, and advanced under X-ray visualization to the mouth of the vessels supplying the heart. As a special dye (contrast medium) is injected through the catheter and fills the inside of the vessels, the angiography device takes a series of X-rays. Like a road map, these films show all the stenoses, blockages, kinks and their severity in percentage terms. The biggest advantage is that if a critical stenosis is detected during the procedure, it can be treated with a balloon or stent procedure in the same session. This makes angiography both a diagnostic and therapeutic procedure.
What is the Role of Lifestyle Changes in Atherosclerosis Treatment?
The cornerstone, roof and walls of atherosclerosis treatment are lifestyle changes. No matter how sophisticated the drugs and surgeries, if this foundation is not solid, treatment cannot be successful in the long term. These changes target the root causes of the disease. Here are the essentials of treatment.
Heart-Friendly Nutrition: You should reduce some things on your table and increase others.
What needs to be reduced:
- Red meat and processed meat products (salami, sausage)
- Saturated fats such as butter, tail fat
- Packaged foods, biscuits, crackers (Trans fat)
- Sugary drinks and sweets
- Salt and salty foods
What needs to be increased:
- Olive Oil
- Fish (especially fatty fish such as salmon and sardines)
- Nuts such as walnuts and almonds
- Plenty of vegetables and fruit
- Legumes and whole grains
Regular Physical Activity: Aim for at least 5 days a week, 30-45 minutes a day of brisk walking, swimming or cycling.
Quitting Smoking Quitting smoking is the single most important step you can take to reduce your risk of heart attack.
Maintaining Ideal Weight: Even a 5-10% reduction in body weight can have miraculous effects on blood pressure, cholesterol and blood sugar.
Which Drug Groups Are Used in Atherosclerosis Treatment?
Drug therapy is designed to support lifestyle changes and stop the progression of atherosclerosis, reducing the risk of complications. The main weapons we use in this treatment are:
- Statins: These drugs not only lower cholesterol, but also reduce inflammation in the vessel wall and “stabilize” existing plaques, reducing the risk of rupture. They are the backbone of atherosclerosis treatment.
- Antiplatelet Drugs: Known as blood thinners, these drugs (Aspirin, Clopidogrel, etc.) prevent clot formation by preventing blood platelets from sticking together.
- Antihypertensive Drugs: By controlling high blood pressure, they reduce stress on the vessel wall and prevent damage.
- Other Cholesterol Drugs: Drugs such as ezetimibe and PCSK9 inhibitors come into play when statins are insufficient or cannot be used.
What Interventional and Surgical Treatments Are Available for Advanced Atherosclerosis?
If the patient’s symptoms persist despite medication and lifestyle changes, or if there is an emergency such as a heart attack, further treatments are needed to physically restore blood flow. Which method is chosen at this point depends on the location, number, length and general condition of the patient.
- Angioplasty and Stenting: This is a minimally invasive procedure usually preferred for simpler, single and short stenoses. The area of stenosis is widened with a balloon and a metal cage called a “stent” is permanently implanted to prevent the vessel from closing again.
- Atherectomy: This is a procedure that can also be described as “intravascular shaving”. It is used especially when very hard, calcified and petrified plaques cannot be opened with a balloon. A rotating drill bit or a sharp knife at the end of the catheter scrapes or shreds the hard plaque. This usually leads to more successful stent placement.
- Endarterectomy: This is the surgical opening of the blood vessel and the removal of the plaque by peeling it off as a whole. It is most commonly performed on the carotid artery in the neck (carotid endarterectomy) to reduce the risk of stroke. It is a highly successful surgery with proven effectiveness in stroke prevention.
- Coronary Artery Bypass Grafting (CABG): This is open heart surgery and usually offers the best and most permanent solution for the most advanced forms of atherosclerosis. Bypass surgery is especially preferred when there are severe stenoses in multiple vessels in the heart, when the stenoses are located in the main branches of the vessels or when the patient has diabetes. In this surgery, the blockage is overcome by bridging. New blood vessels from another part of the body (the inner chest wall, arm or leg) are sewn ahead of the blockage. This allows the blood to “bypass” the blocked area and reach the heart muscle directly, restoring the heart’s nutrition.
Is it Possible to Prevent or Slow the Development of Atherosclerosis?
Definitely yes. The most effective strategy to fight atherosclerosis is to ensure that the disease never starts or progresses. It is not a fate and we can greatly influence the course with our lifestyle choices. Prevention is always easier, cheaper and more effective than treatment. Since the foundations of atherosclerosis are laid in childhood, it is critical to adopt healthy lifestyle habits at the earliest possible age.
Modern medicine offers extraordinary possibilities to repair the damage caused by atherosclerosis. However, the best results are always achieved in patients who combine these cutting-edge treatments with basic lifestyle changes. Remember that a healthy lifestyle is the most important insurance for the success and longevity of any medical and surgical intervention.
The basic principles of prevention are simple:
- Do not smoke.
- Keep moving.
- Eat a healthy diet.
- Keep your weight under control.
- Have your blood pressure, cholesterol and blood sugar checked regularly.
Frequently Asked Questions
What is atherosclerosis?
It is the narrowing and hardening of the arteries as a result of the accumulation of fat, cholesterol and other substances on the inner surface of the arteries, forming plaque.
What is it popularly known as?
It is commonly known as “arteriosclerosis” or “atherosclerosis”.
Which blood vessels does it affect?
It can affect all arteries, including heart vessels, brain vessels, leg vessels and kidney vessels.
What are the symptoms?
It depends on the area affected by the vessel: Chest pain, leg pain, high blood pressure, stroke, shortness of breath.
What is the main cause of atherosclerosis?
High cholesterol, high blood pressure, smoking, diabetes and obesity are the most common causes.
At what age does this disease start?
Plaque deposition can begin in childhood; clinical symptoms usually appear in middle age and beyond.
How is it diagnosed?
It can be diagnosed with methods such as blood tests, ECG, effort test, Doppler ultrasound, CT angiography.
Can atherosclerosis be completely cured?
Plaques cannot be reversed, but their progression can be halted and controlled with lifestyle changes.
What complications can it cause?
It can lead to serious consequences such as heart attack, stroke, leg gangrene and kidney failure.
How to prevent it?
It can be prevented with a healthy diet, regular exercise, smoking cessation, blood pressure and cholesterol control.
Is drug treatment effective?
Yes, medicines such as cholesterol-lowering drugs (statins), blood pressure medicines and aspirin can control atherosclerosis.
Is surgical treatment necessary?
If the vessel is severely blocked, surgery such as bypass, stenting or endarterectomy may be necessary.
Is atherosclerosis genetic?
Individuals with a family history of early heart disease may have a genetic predisposition.
Are women or men more affected?
It occurs at an earlier age in men, but postmenopausal women are also at increased risk.
Which specialty deals with this disease?
Cardiology, vascular surgery and internal medicine specialists follow up together.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.