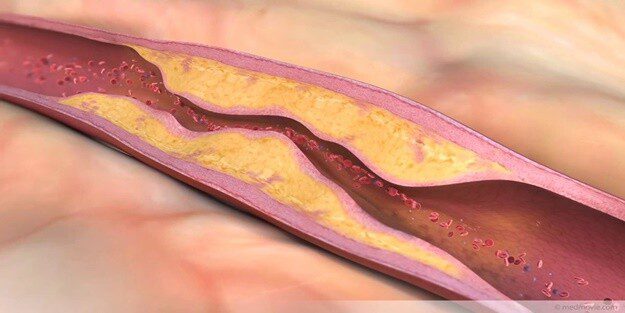
Atherosclerotic plaque is a pathological formation inside arteries, consisting of fat, cholesterol, calcium, and cellular waste. These deposits narrow the vessel lumen, reduce blood flow, and may cause cardiovascular diseases. Plaque rupture can trigger clot formation, leading to heart attack or stroke.
Plaque development is a slow process influenced by risk factors such as high cholesterol, hypertension, diabetes, and smoking. Genetic predisposition and unhealthy lifestyle further accelerate vascular damage. Early detection through imaging and laboratory tests is crucial for prevention and treatment planning.
Symptoms of vascular plaque depend on the affected artery. Coronary artery involvement may cause chest pain or shortness of breath, while leg arteries may lead to claudication. Asymptomatic progression is common, making routine cardiovascular screening important, especially in high-risk individuals.
Treatment strategies include lifestyle modification, medication, and in advanced cases, interventional procedures such as angioplasty or bypass surgery. Lowering cholesterol, controlling blood pressure, and quitting smoking significantly reduce progression. Comprehensive management improves long-term cardiovascular health and life expectancy.
| Medical Name | Atherosclerotic Plaque |
| Common Symptoms | – May initially be asymptomatic – Chest pain (angina) – Shortness of breath – Exertional fatigue or chest tightness |
| Causes | – Cholesterol and fat accumulation in the vessel wall – Inflammation – Smoking – High blood pressure – Diabetes |
| Risk Factors | – High cholesterol- Hypertension- Diabetes- Smoking- Obesity- Advanced age- Family history of early heart disease |
| Complications | – Coronary artery disease – Heart attack (myocardial infarction) – Stroke – Peripheral artery disease |
| Diagnostic Methods | – ECG- Effort test- Coronary angiography- CT angiography- Blood tests (cholesterol, lipid profile) |
| Treatment Methods | – Lifestyle changes (diet, exercise)- Cholesterol-lowering drugs such as statins- Blood thinners- Angioplasty or stent placement if necessary |
| Prevention Methods | – Healthy diet- Regular exercise- Quitting smoking and alcohol use- Blood pressure and sugar control |
Why and How Does Plaque Formation Start in My Veins?
Imagine the arteries that nourish your body as flexible tubes covered with a smooth, slippery inner layer. This slippery inner surface allows blood to flow freely and without getting stuck. However, some factors begin to damage this delicate surface. There are major risk factors that trigger plaque formation in the vessel wall and accelerate the process:
Some of these risk factors include:
- High levels of “bad” cholesterol (LDL)
- High blood pressure (Hypertension)
- Cigarette smoking
- Diabetes (Diabetes)
- Family history of early heart disease
- Sedentary lifestyle
- Unhealthy eating habits
- Overweight or obesity
- Intense and chronic stress
These risk factors cause tiny, invisible injuries to the smooth inner wall of the blood vessel. As with any injury, the body’s defense system immediately wants to intervene in this area. The “bad” cholesterol (LDL) particles in the blood easily leak through these damaged areas into the vessel wall and begin to accumulate there.
The body recognizes this deposit as a foreign substance and assigns white blood cells called “macrophages” to clean it up. However, as the macrophages try to swallow the cholesterol, they become so full that they get out of control and turn into fat-filled cells called “foam cells”. As these foam cells accumulate in the vessel wall, they initially form early-stage lesions called “fatty streaking”. This process is so silent that it can start in the teenage years or even in childhood without us even realizing it.
Over the years, the body tries to cover this damaged and fat-filled area with a kind of “scab” to contain it. This scab is made up of collagen fibers and smooth muscle cells. We call this structure of fatty core and the crust over it the atherosclerotic plaque. As the plaque grows, it narrows the pathway through which the blood flows, leading to what we know as cardiovascular blockage.
What Are the Symptoms of Plaque in the Heart and How Does It Feel in My Body?
Arteriosclerosis, or atherosclerosis, can progress completely silently for many years. As the plaques grow slowly and the vessels try to compensate by stretching a little, you may not feel anything until blood flow is severely impeded. Symptoms of plaque in the heart usually manifest themselves when the narrowing of the vessel exceeds p or, more importantly, when a plaque suddenly ruptures and forms a clot.
Symptoms vary depending on which organ the plaque is in the blood vessel supplying which organ.
If your heart vessels (coronary arteries) are affected, these are the symptoms you may experience:
- Pressure, tightness or burning sensation in the chest (angina)
- Pain radiating to the left arm, shoulder, jaw or back
- Shortness of breath, especially with exertion
- Tired more quickly than usual
- Palpitations
Symptoms you may experience if your blood vessels to the brain (carotid arteries) are affected:
- Sudden weakness or numbness on one side of the body
- Percentage shift
- Speech difficulty or lisping
- Sudden and temporary loss of vision
- Severe dizziness or loss of balance
Symptoms you may feel if your leg veins (peripheral arteries) are affected:
- Cramp-like pain in the legs, especially in the calves, when walking
- Pain that goes away at rest but recurs when you start walking
- Coldness or pallor of the feet
- Discoloration (bruising) of the toes
- Non-healing wounds on the legs and feet
Is Every Arterial Plaque Equally Dangerous?
This question is one of the most critical points about vascular plaque. Contrary to popular belief, the danger of a plaque depends less on how much it constricts the vessel and more on how “robust” its structure is. Like a volcano, some plaques are dormant and calm, while others are active and ready to erupt at any moment.
Stable records: These are “good” records. They are covered with a thick and strong crust. The fatty core inside them is smaller and there are fewer inflammatory cells. These plaques grow slowly over time and narrow the arteries. They cause predictable symptoms that usually occur when you exert yourself (e.g. your chest hurts when climbing hills) and go away when you rest. Thanks to their thick shells, they are less likely to rupture and form a sudden clot.
Vulnerable (Sensitive/Unstable) Plaques: These are the “sneaky” and dangerous ones. Since they usually do not narrow the vessel very much (less than P), they can even be missed in standard controls. But their structure is extremely fragile. They have a very thin shell and are filled with an almost liquid, fatty, inflamed core. Triggers such as high blood pressure or sudden stress can easily tear this weak shell.
As soon as a vulnerable plaque ruptures, the substances inside it with high clotting potential come into contact with the blood. The body recognizes this as a major bleeding and tries to stop the bleeding by forming a giant clot in the area within seconds. However, this giant clot suddenly and completely blocks the already narrow vessel. If this happens in a blood vessel supplying the heart, a heart attack occurs, and if it happens in a blood vessel going to the brain, a stroke occurs. Sudden rupture of these vulnerable plaques is the mechanism behind the vast majority of heart attacks and strokes today.
How to Diagnose Plaque in My Veins?
To find out if you have plaque in your veins, an assessment process is carried out in a series of steps. This process starts with a simple conversation and, if necessary, involves advanced technologies that go inside your blood vessels. The aim is not only to see if there is a stenosis, but also to understand how much risk that stenosis poses to you.
The evaluation process usually includes the following steps:
Doctor’s Interview and Physical Examination: First of all, you will be interviewed in detail. Your complaints, lifestyle, eating habits and family history of illness are listened to. Your blood pressure is measured and your heart and blood vessels are listened to with a stethoscope.
Blood Tests A simple blood test looks at your cholesterol (LDL, HDL), triglyceride and blood sugar levels. Tests such as hs-CRP can also help determine your risk of heart disease by giving you an idea of the general state of inflammation in your body.
Non-invasive Tests: These tests, which are performed without any instruments entering your body, are the first steps in finding the source of the problem.
- Electrocardiogram (ECG)
- Effort ECG (treadmill test)
- Echocardiography (Heart ultrasound)
- Doppler Ultrasound
- Coronary Calcium Scoring (Tomography)
- CT Angiography
Interventional tests (angiography): If there is a serious suspicion from previous tests or if treatment is to be planned, angiography is needed to get a clear view of the inside of the arteries. This is done by inserting a thin tube (catheter) through an artery in the groin or wrist. Through this catheter, a so-called “contrast dye” is injected into your blood vessels and X-rays are taken. This provides a road map of your blood vessels, clearly identifying the location, number and severity of stenoses. Angiography is considered the gold standard for diagnosing cardiovascular blockages.
How to Prevent Plaque Formation in Arteries?
“Once the disease has started, is it reversible?” or “How can plaque formation in the arteries be prevented?” are the questions we hear most often. The most powerful weapon in the treatment of this disease is to stop the progression of the disease and prevent new plaques from forming. It rests on two pillars: lifestyle and medication.
Steps You Can Take to Improve Your Lifestyle:
Changes you can make to your diet:
- Processed meats (salami, sausage, pepperoni)
- Fried foods and packaged products containing trans fats
- Sugary and carbonated drinks
- Refined carbohydrates such as white bread, rice
- Reduce salt consumption.
Recommended foods to consume:
- Plenty of green leafy vegetables
- Fruits
- Legumes (chickpeas, lentils, beans)
- Whole grains (oats, buckwheat, whole wheat bread)
- Nuts such as walnuts, hazelnuts, almonds
- Olive Oil
- Fish (especially those rich in omega-3 such as salmon and sardines)
Other habits you should incorporate into your life are:
- Brisk walking for at least 150 minutes a week
- Quit smoking completely
- Limiting alcohol consumption
- Maintaining your ideal weight
- Stress management techniques (yoga, meditation, hobbies)
Medication Therapy:
When lifestyle changes alone are not enough or if your risk is high, medication is mandatory.
Statins: These cholesterol-lowering drugs are the backbone of treatment. Not only do they lower cholesterol, but they also reduce inflammation within the plaque, making it more stable.
Blood Pressure Drugs: They reduce stress on the vessel wall by keeping blood pressure at ideal levels.
Blood Thinners (Antiplatelet Agents): Drugs such as aspirin reduce the risk of clots forming on the plaques. It is especially vital in patients who have had a previous heart attack, stroke or stent.
Diabetes Medicines: Keeping blood sugar under tight control prevents the devastating effects of diabetes on blood vessels.
Are There Really Drugs That Dissolve Vascular Plaque?
This is one of the biggest hopes of our patients and one of the most frequently asked questions: “Hodja, isn’t there a medicine that will completely dissolve and clean the plaque in my arteries?” There are many claims on the internet or among the general public about “vascular plaque dissolving drugs” or various “vasodilator cures”. It is very important to clarify this issue. In the light of the available scientific evidence, there is no medicine that magically removes, completely “dissolves” or “cleanses” vascular plaque once it has formed and hardened.
So what are the drugs for? The main goal of drug therapy (especially the powerful statin therapies) is not to destroy plaque, but to “neutralize” and “calm” it. The drugs transform a dangerous and “fragile” plaque that is ready to rupture into a “stable” plaque with a thicker crust that does not tear easily. By lowering the cholesterol in the blood very low, they prevent the plaque from growing further and extinguish the inflammation inside. Although some reduction in plaque size has been shown to be possible with very intensive and long-term treatment, the main benefit is to render the plaque non-hazardous. In other words, the medical answer to the question of how to remove plaques in the blood vessels is to control them with medication and lifestyle and transform them into a harmless, calm structure.
How is Petrified Calcific Plaque Treatment Performed?
If you have seen something like “calcified atheroma plaques in the aorta” on your CT scan or angiography report, it means that some of the plaque in your blood vessels has calcified, i.e. hardened, over time. Calcification is an advanced stage of plaque. The body deposits calcium in the area to limit chronic inflammation and the plaque becomes “petrified”. On the one hand, this may be a sign that the plaque is becoming more stable, but on the other hand, it complicates matters when treatment is needed.
Because it’s a calcified, rock-hard plaque;
- It cannot be easily dilated with a standard balloon.
- It prevents the stent from opening and sticking to the vessel wall.
- It makes it difficult for the drug in medicated stents to reach the vessel wall.
This is why the treatment of calcific plaque requires special techniques. This is where the so-called “atherectomy”, intravascular shaving or sanding methods come into play. With these methods, the vessel is prepared for treatment by removing the hard layer of lime with special tools before stent or balloon placement.
Some of the atherectomy methods are as follows:
Rotational Atherectomy: It is the process by which a wire with a diamond head at the end rotates at very high speed to pulverize calcareous plaque.
Orbital Atherectomy: It rotates with a different mechanism and grinds the calcareous plaque in an orbital movement.
Laser Atherectomy: The hard plaque is vaporized using laser energy.
When is Cardiovascular Surgery Inevitable?
Despite all the advances in intravascular treatments such as stents and balloons, in some cases cardiovascular surgery is the best and most permanent solution. The decision to operate is never made by a single person. A “Heart Team”, consisting of a cardiologist and a cardiovascular surgeon, examines the patient’s condition in detail and decides together which is the best way forward for that patient.
Surgery is usually indicated in the following cases:
- If there are severe stenoses in multiple vessels supplying the heart (multivessel disease).
- If there is a critical stenosis in the left main coronary artery, the main artery of the heart.
- In diabetic patients, surgery may give better results because vascular disease is usually more widespread and involves thin vessels.
- The structure of the stenosis is not suitable for stent treatment.
- If another heart problem, such as a heart valve, needs to be treated at the same time.
The most common surgical procedure is coronary artery bypass surgery. The idea of this surgery is that instead of opening the blocked artery, new pathways, or “bridges”, are built to allow blood to travel around the blockage and reach the heart. The most valuable material for these bridges is the artery from the patient’s own chest wall (LIMA). Due to its structure, this artery is very resistant to re-narrowing and remains open for many years, increasing the quality and duration of life of the patient. If necessary, arteries from the arm or veins from the leg can also be used for these bridges.
Is Vascular Health a Whole as Arteries and Veins?
Yes, vascular health is a whole, but arterial and venous diseases occur through different mechanisms. The topics we have discussed so far, such as plaque, calcification, treatment of cardiovascular narrowing, are all related to atherosclerosis, a disease of the arteries.
However, the swelling, purple veins and pain in the legs that our patients frequently ask about are usually associated with varicose veins, a vein disease. Varicose veins are caused by the deterioration of the valves in the veins that carry blood back to the heart. The cause is a mechanical failure, not plaque.
A cardiovascular surgeon treats the circulatory system as a whole. For this reason, he is the right address for your arterial problems as well as for your vein complaints such as varicose veins. Today, there are very effective methods for the treatment of varicose veins. Most of the time, great results can be achieved aesthetically and functionally with methods such as laser, radiofrequency or foam therapy (sclerotherapy), known as non-surgical varicose vein treatment. For thinner veins, capillary varicose veins can also be treated with these methods. Remember, your circulatory system is a whole and both arterial and venous health are critical to your overall quality of life.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.