Heart vessel blockage symptoms develop when coronary arteries narrow due to atherosclerosis. The most common sign is angina, characterized by chest pain or pressure spreading to the arm, neck, or jaw. Shortness of breath, fatigue, and sweating may also indicate reduced blood flow to the heart.
Early warning signs of coronary blockage include exertional discomfort, irregular heartbeat, and lightheadedness. These symptoms often worsen with stress or physical activity and improve with rest. Ignoring such signs increases the risk of myocardial infarction.
Silent coronary artery disease can present with atypical symptoms such as indigestion, nausea, or extreme fatigue. This is more common in diabetic and elderly patients, making regular cardiac screening essential for early detection.
If severe blockage occurs, it can lead to acute heart attack. Emergency symptoms include intense chest pain, cold sweats, fainting, and difficulty breathing. Immediate medical intervention is crucial to restore circulation and prevent heart muscle damage.
| Definition | Partial or complete obstruction of blood flow in one or more of the coronary arteries supplying the heart |
| Causes | Atherosclerosis (arteriosclerosis), plaque buildup in the vessel wall, blood clot (thrombus), coronary artery spasm |
| Risk Factors | Smoking, hypertension, diabetes, high cholesterol, obesity, advanced age, family history of heart disease, sedentary lifestyle, stress |
| Symptoms | Chest pain (angina), shortness of breath, sweating, weakness, nausea, fatigue, palpitations, sometimes sudden heart attack |
| Diagnostic Methods | ECG, stress test, echocardiography, coronary angiography, CT-angiography, blood tests |
| Treatment Methods | Antiplatelet drugs, statins, beta blockers, ACE inhibitors, balloon angioplasty, stents, coronary bypass surgery, lifestyle changes |
| Complications | Heart attack, heart failure, arrhythmia, sudden cardiac arrest, sudden death |
| Prevention Methods | Smoking cessation, healthy and balanced diet, regular exercise, stress management, blood pressure and cholesterol control, diabetes management, regular use of medications |
What Causes Cardiovascular Blockage?
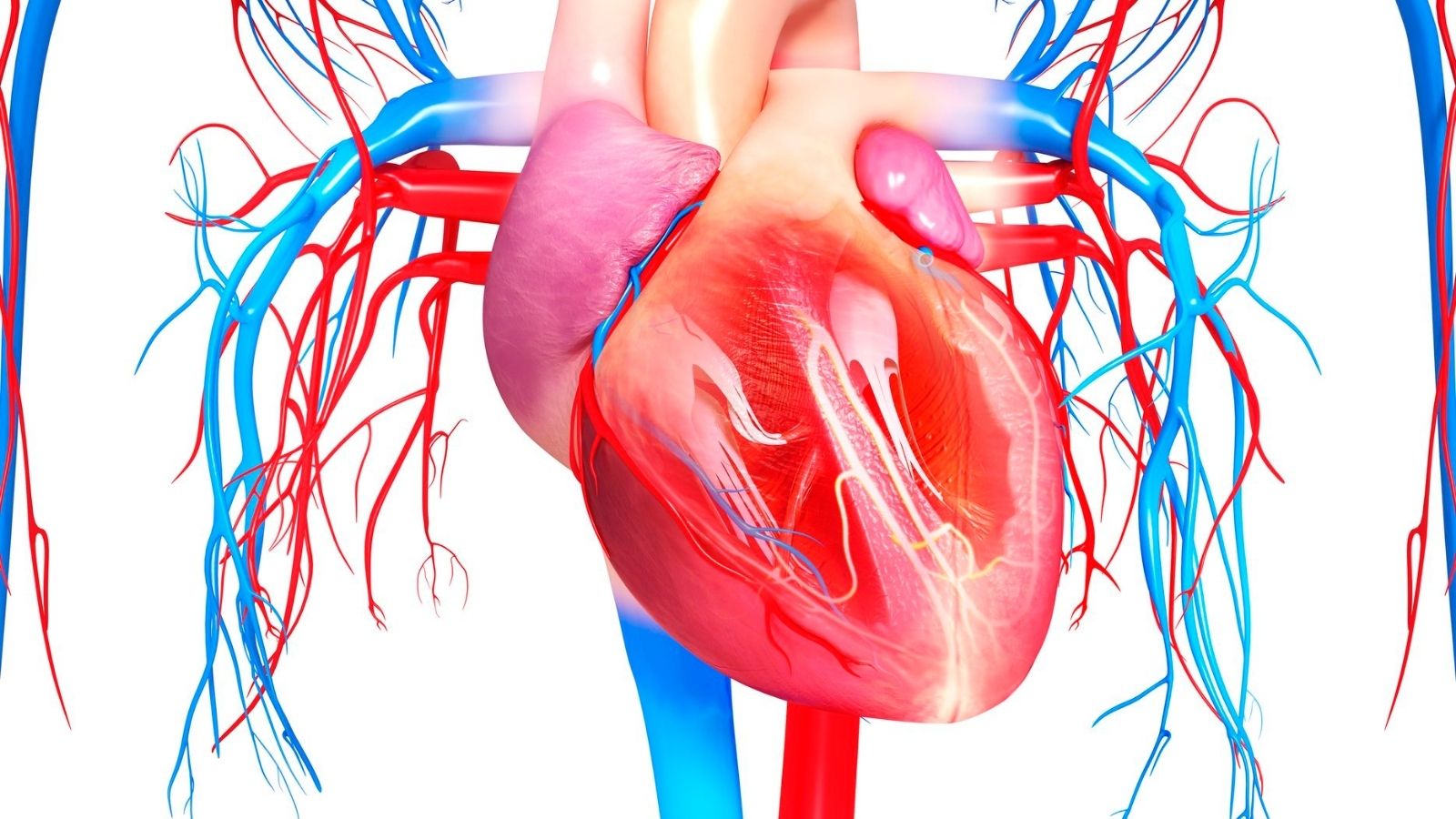
We can think of our arteries like clean water pipes in our homes. Just as lime, rust and sediment accumulate inside the pipes over the years, making it difficult for the water to flow, a similar process takes place inside our arteries. This condition, whose medical name is “atherosclerosis”, is popularly known as “arteriosclerosis” and is the basic answer to the question of why vascular blockage occurs.
This process can actually start at a very early age, even in childhood. It is all triggered by damage to the delicate and miraculous single layer of cells lining the inner surface of the blood vessel, which we call the “endothelium”. A healthy endothelium keeps the blood vessel flexible, blood flowing smoothly and clotting under control. However, when this layer is damaged by some harmful factors, it loses its protective properties. Just as food starts to stick when the surface of a Teflon pan is scratched, damaged endothelium causes bad cholesterol (LDL) and inflammatory cells in the blood to stick to the vessel wall and leak out.
These fat particles seep into the vessel wall, where they change structure and are perceived as a threat to the body. Macrophages, the body’s defense cells, come to the area to clear these fats and engulf them, turning them into fat-filled cells called “foam cells”. Over time, these foam cells, dead cells, cholesterol crystals and calcium accumulate to form a hillock called “plaque”. As these plaques grow, they narrow the lumen, the blood flow path inside the blood vessel. This is what we call cardiovascular narrowing.
Who is more at risk for vascular occlusion?
There are some risk factors that accelerate the development of atherosclerosis and predispose to atherosclerosis. We can divide them into those we cannot change and those we can fight against.
What are the Risk Factors that cannot be changed?
These factors are beyond our control, but knowing them is a warning to hold on tighter to other factors that we can change.
- Advancing age
- Male gender
- Family history (presence of early-onset heart disease in first-degree relatives)
What are modifiable risk factors?
This is our main area of struggle. By controlling these factors, we can protect our vascular health to a great extent.
- High blood pressure (Hypertension)
- High cholesterol (especially LDL – bad cholesterol)
- Diabetes (Diabetes)
- Smoking and use of tobacco products
- Overweight and obesity (especially abdominal fat)
- Sedentary lifestyle
- Unhealthy eating habits
- Intense and unmanageable stress
- Sleep apnea
What are the Symptoms of Vascular Blockage in the Heart?
Blockage in the coronary arteries, the vessels that supply the heart, is the most common and dangerous vascular disease. Symptoms of atherosclerosis in the heart vary depending on the degree of blockage and the nature of the plaque.
What are the Symptoms of Stable Stenosis?
In this case, the stenosis is fixed and is usually symptomatic during exertion. At rest, the heart can cope with the small amount of blood it receives. But when you walk, climb stairs or get excited, the heart’s workload increases and it needs more blood. When the narrowed blood vessel cannot meet this demand, the typical “angina pectoris” (chest pain) occurs. These symptoms include:
- Pressure, squeezing, heaviness or burning sensation in the center of the chest
- This sensation spreads to the left arm, neck, jaw, back or stomach
- Symptoms usually start with exertion
- Relief in a few minutes with rest or sublingual medication
What are the Symptoms of Sudden Congestion (Heart Attack)?
In contrast to the stable state, here the plaque in the vessel suddenly ruptures and a clot quickly forms on it, completely blocking the vessel. This means that that area of the heart muscle is starved of blood and begins to die, requiring urgent medical attention. Symptoms are more severe and do not go away with rest.
- Chest pain that is very severe and lasts longer than 20 minutes
- Cold sweating
- Nausea and vomiting
- Shortness of breath
- Dizziness
- An intense fear of death or anxiety
Can Cardiovascular Blockage Symptoms Be Different in Women?
Yes, this is a very important point. Symptoms of cardiovascular blockage in women may differ from the classic chest pain in men. These atypical symptoms can delay diagnosis. Women, the elderly and people with diabetes should be especially alert to the following symptoms
- Shortness of breath
- Sudden and extreme fatigue, weakness
- Pain in the back, shoulders or jaw
- Discomfort, indigestion or burning sensation in the stomach area
- Dizziness and lightheadedness
What are the Symptoms of Cardiac Capillary Occlusion?
Sometimes patients present with typical chest pain, but angiography does not reveal any significant blockage in the large vessels of the heart. One cause of this is microvascular disease, which affects the much smaller, invisible capillaries of the heart. Symptoms of cardiac capillary blockage can also take the form of typical angina pain, usually on exertion, and can severely impair quality of life. Diagnosis and treatment require specialized approaches.
What are the Symptoms of Vascular Blockage in the Leg?
Peripheral arterial disease, a blockage of the arteries that carry blood to the legs, is also popularly known as “window disease”. This is because after walking for some distance, the patient has to stop and rest because of pain in the legs, especially in the calves, and pretend to look at shop windows. Symptoms of a blocked vein in the leg may include
- Pain, cramping or fatigue in the leg muscles (usually calf, thigh or buttock) with walking
- This pain is relieved in a short time by resting
- Chills or coldness in the feet and legs
- Skin discoloration or bruising
- Hair loss on the legs
- Thickening and slow growth of toenails
When the disease progresses, pain occurs even at rest and the foot may develop non-healing wounds or gangrene. This condition is called “critical leg ischemia” and requires urgent intervention to prevent loss of the leg (amputation).
What are the symptoms of occlusion of the carotid artery feeding the brain?
Blockage in the carotid arteries, which are located on either side of the neck and carry blood to the brain, is one of the most important causes of stroke. A small clot that breaks off from a plaque in this artery can block the brain vessels and cause permanent damage. Sometimes this is temporary and is called a “Transient Ischemic Attack” (TIA). A TIA is a harbinger of a major stroke and must be taken seriously. Stimulating symptoms include:
- Sudden weakness or numbness in one half of the body (face, arm or leg)
- Sudden deterioration in speech, lisp or difficulty understanding what is being said
- Sudden loss of vision or blurred vision in one or both eyes
- Sudden and severe headache
- Loss of balance or dizziness
How to Detect Cardiovascular Blockage without Angiography?
This is one of the most curious topics for our patients. How to detect cardiovascular blockage without angiography? Yes, angiography is the gold standard for imaging the vessels, but it is not the first and only option for diagnosis. There are many harmless and easy tests that we use, especially for risk assessment and initial diagnosis.
The diagnostic process begins with listening to the patient’s complaints and a detailed physical examination. The following tests may then be ordered depending on the area of the suspected vein.
Tests Used for the Heart:
- Electrocardiogram (ECG): Measures the electrical activity of the heart. It can give clues during a heart attack or about previous attacks.
- Effort Test (Treadmill): The patient walks on a treadmill while their ECG and blood pressure are monitored. The aim is to see if a blood supply disorder (ischemia) occurs in the heart during exertion.
- Echocardiography (ECHO): Ultrasound of the heart. It shows the strength of contraction of the heart muscle, heart valves and movement disorders in the heart walls. When performed with exertion (Stress ECHO), it shows how exertion affects heart contraction.
- Myocardial Perfusion Scintigraphy (Thallium Test): A radioactive substance is administered intravenously and a special camera monitors how much blood flows to different parts of the heart, both at rest and after exertion.
Coronary CT Angiography: This is an advanced test performed with medicated (contrast-enhanced) tomography that creates three-dimensional images of the vessels supplying the heart. It shows vascular stenoses with high accuracy and is an important guide in deciding whether angiography is needed.
Tests for the Leg and Carotid Vessels:
- Doppler Ultrasonography: Sound waves are used to measure the speed and direction of blood flow in the vessel. It is a harmless and most commonly used first-line test that provides valuable information about the location and degree of stenosis.
- Ankle-Brachial Index (ABI): A simple test comparing leg and arm blood pressure. It gives an idea about the presence and severity of vascular occlusion in the legs.
What Methods Are There for the Treatment of Cardiovascular Occlusion?
The treatment of cardiovascular occlusion is based on three pillars: lifestyle changes, medication and interventional therapies to open the vessels. The aim of treatment is not only to relieve existing symptoms but also to slow the progression of the disease and prevent serious events such as heart attack, stroke and death.
- The Basis of Treatment: Lifestyle and Medicines
- No matter what interventional treatment is applied, this foundation can never be neglected. As a surgeon, we know that even if we open a vessel with surgery, if our patient does not follow these basic rules, other vessels or the same vessel may become blocked again.
Medication Therapy:
- Blood thinners (antiplatelets): Drugs such as aspirin and clopidogrel prevent blood platelets from sticking together and make clot formation more difficult.
- Cholesterol Lowering Drugs (Statins): Not only lower bad cholesterol, but also reduce inflammation inside the plaque, stabilizing it and reducing the risk of rupture.
- Blood Pressure Medicines: Reduce stress on the vessel wall by keeping blood pressure at ideal levels.
- Blood Sugar Regulators: Controlling blood sugar in diabetics is vital to prevent vascular damage.
Lifestyle Changes:
- Absolute cessation of smoking
- Mediterranean-type, vegetable-fruit-heavy, saturated fat-poor diet
- Regular exercise (such as brisk walking for at least 150 minutes a week)
- Maintaining ideal weight
- Stress management techniques
- Interventional Therapies to Open Vessels
In patients whose complaints persist despite medication and lifestyle changes, or who present with emergencies such as heart attack or critical leg blockage, it is necessary to open the blocked vessel. There are two main methods for this: endovascular (closed) methods and open surgery.
Endovascular Methods (Balloon/Stent): A thin catheter is usually inserted through the groin or arm artery to reach the blocked area.
Balloon Angioplasty: The balloon at the end of the catheter is inflated at the site of the stenosis to crush the plaque and open the vascular access.
Stenting: To prevent the vessel from narrowing again after ballooning, a small wire tube called a stent is inserted into the vessel. These stents act as a scaffold to keep the vessel open. Today, drug-eluting stents that prevent re-narrowing are mostly used.
Open Surgical Methods (Bypass/Endarterectomy): Open surgery offers a more permanent and effective solution, especially in patients with diffuse and complex blockages in multiple vessels or in cases where the endovascular method is not suitable.
Bypass Surgery: We can think of this method as building a new ring road on a congested highway. A new bridge is created by using a vein from another part of the body (intrathoracic artery, artery from the arm or vein from the leg) to bring blood to the blockage. Coronary bypass surgery provides longer-lasting results and a better survival advantage than stenting, especially in patients with diabetes and multivessel disease.
Endarterectomy: In this procedure, the vessel is surgically opened and the plaque inside is removed as a whole, almost like a mold. It is the most common and durable surgical method especially in carotid and groin artery occlusions.
Is Cardiovascular Blockage a Risk of Death?
The answer is yes, blocked arteries carry a risk of death. A sudden heart attack caused by a blocked heart vessel or a large stroke caused by a blocked carotid artery can unfortunately be fatal. But this is not fate. Modern diagnostic and treatment methods have significantly reduced this risk. The important thing is to be aware of the risk factors, to take the signals given by our body (such as chest pain, shortness of breath, leg pain) seriously and to consult a physician on time. With early diagnosis and proper treatment, the majority of our patients can lead a healthy and active life. Remember that atherosclerosis is a consequence; the real fight should be against the causes that lead to it.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.