Heart failure symptoms develop when the heart cannot pump blood effectively to meet the body’s needs. This condition results in fluid buildup and reduced oxygen delivery, leading to significant physical limitations.
Common symptoms include persistent fatigue, shortness of breath, and swelling in the legs or abdomen. These signs indicate impaired cardiac function and often worsen over time if left untreated.
Advanced heart failure may present with irregular heartbeat, dizziness, and difficulty performing daily activities. Recognizing early warning signs is essential for timely medical evaluation and treatment initiation.
Treatment of heart failure symptoms includes lifestyle changes, medications such as ACE inhibitors and beta-blockers, and in some cases device implantation or heart transplantation. Comprehensive management improves survival and quality of life.
| Definition | Inability of the heart to pump enough blood to meet the needs of body tissues |
| Causes | Coronary artery disease, hypertension, heart valve diseases, cardiomyopathy, myocarditis, damage after heart attack, congenital heart diseases |
| Risk Factors | Advanced age, hypertension, history of heart attack, diabetes, obesity, smoking, alcohol use, kidney disease, familial predisposition |
| Symptoms | Shortness of breath, swelling in the legs and feet (edema), weakness, fatigue, shortness of breath that increases at night, palpitations, loss of appetite, weight gain or loss |
| Diagnostic Methods | Physical examination, ECG, echocardiography, chest radiography, blood tests (BNP, troponin), exercise test |
| Treatment Methods | Lifestyle changes, diuretics, ACE inhibitors, beta blockers, ARB, aldosterone antagonists, digoxin, device therapies (pacemaker, ICD), heart transplantation in advanced cases |
| Complications | Acute attack of heart failure, arrhythmia, renal failure, pulmonary edema, liver failure, decreased quality of life |
| Prevention Methods | Control of risk factors (hypertension, diabetes, cholesterol), regular exercise, healthy diet, avoidance of smoking, regular use of medications, doctor control |
What is Heart Failure and How Does It Fundamentally Affect the Body?
Heart failure can be likened to a water pump system. If the pump is weakened, not enough water gets to the furthest parts of the garden and at the same time water starts to accumulate at the inlet of the pump. This is what happens in heart failure. When the heart’s pumping power decreases, two main problems arise in the body.
- The first is what we call “forward flow failure”. This means that the heart cannot send enough oxygen-rich blood to the organs and tissues. Your muscles, brain and other organs don’t get the energy they need. This is why people with heart failure experience constant fatigue, weakness and exhaustion. Even the simplest daily tasks, such as climbing stairs or carrying shopping bags, can feel like a marathon.
- The second is “back pooling”, or “congestion” in medical terms. Because the pump cannot push the blood forward, it begins to pool behind the heart, in the veins. This is similar to a traffic jam. The blood builds up inside the vessels and the increased pressure causes fluid to leak out of the vessels and into the tissues. If this fluid builds up in the lungs, the person will experience shortness of breath. This is like the lungs being “submerged” and is especially pronounced when lying on the back or during exertion. If fluid accumulation occurs in other parts of the body, such as the legs, ankles or abdomen, swelling (edema) occurs in these areas.
Initially, our body tries to compensate for this. An “emergency mode” kicks in to support the weakened heart. The heart starts beating faster, blood vessels constrict and the body retains more fluid. In the short term, these mechanisms can be life-saving, but in the long term they put even more strain on a tired heart. This becomes a vicious circle and over time leads to worsening heart failure.
What Are the Different Types of Heart Failure?
Heart failure is not a uniform disease; there are subtypes with different characteristics. It is very important to correctly identify these types for proper heart failure treatment. Classification is usually based on three main criteria: the pumping power of the heart, the side of the heart affected and the speed of onset of the disease.
To measure the pumping power of the heart, we use a value called “Ejection Fraction (EF)”. This is a percentage of how much blood the heart pumps with each beat. According to this value, the main types of heart failure are:
- Heart Failure with Low Ejection Fraction (HFrEF)
- Heart Failure with Preserved Ejection Fraction (HFpEF)
- Heart Failure with Mildly Reduced Ejection Fraction (HFmrEF)
The first type, HFrEF or systolic failure, is the more “classic” type of failure, in which the heart’s contractile force is reduced. The heart muscle is weakened and, like a loose rubber ball, cannot squeeze and pump blood forward strongly enough. This type usually occurs after a heart attack. The second type, HFpEF or diastolic failure, is different. Here the heart’s contractile force may be normal, but the heart muscle has become so stiff and rigid that it cannot relax and let enough blood in. It is like a rigid balloon that has lost its elasticity and cannot be inflated. Even if the percentage of blood being pumped seems normal, the body still does not get enough blood because there is not enough blood filling it. This type is usually seen in people who have had high blood pressure or diabetes for many years. HFmrEF describes patients who fall in a “gray area” between these two types.
Heart failure is also classified according to which side of the heart is more affected:
- Left-sided Heart Failure
- Right-sided Heart Failure
Left-sided heart failure is the most common type. The left side of the heart is responsible for pumping clean blood throughout the body. When this side weakens, blood begins to pool in the lungs, leading to respiratory symptoms such as shortness of breath. Right-sided heart failure is usually a progression of left-sided failure. The right side of the heart is responsible for sending dirty blood to the lungs. As the pressure in the lungs increases, the right side begins to strain and blood pools in the body itself, in the legs, feet and abdomen, causing edema.
What are the Most Important Symptoms of Heart Failure?
So what are the symptoms of heart failure in a person? These symptoms usually start gradually and can worsen over time. Recognizing these signals your body is giving you is vital for early diagnosis and treatment. The most common symptoms are:
- Shortness of breath, especially with exertion or when climbing stairs
- Breathlessness when lying flat on the back and the need to increase the number of pillows
- Waking up suddenly at night with shortness of breath
- Visible swelling of the feet, ankles, legs or abdomen (edema)
- Rapid and unexplained weight gain within a few days
- Persistent fatigue and low energy to the point of not being able to perform even daily activities
- Loss of appetite, bloating or nausea
- Persistent cough or wheezing that does not go away, especially when lying down
- Feeling that the heart is beating fast or irregularly, i.e. palpitations
- Forgetfulness, confusion or difficulty organizing thoughts
The logic behind these symptoms is quite simple. Shortness of breath and coughing are caused by blood pooling in the lungs. Swelling of the feet and abdomen and rapid weight gain are the result of fluid retention throughout the body. Fatigue and weakness are caused by insufficient oxygenated blood supply to muscles and organs. Loss of appetite and nausea can be caused by reduced blood flow to the digestive tract, while confusion can be a sign that blood flow to the brain is affected.
If you are experiencing one or more of these symptoms, you should not take the situation lightly and should consult a physician. Especially sudden onset and severe shortness of breath, chest pain, fainting or expectoration of pink foamy sputum require urgent medical attention.
What are the Main Causes of Heart Failure?
Heart failure is usually not a disease that appears out of thin air; it is often the result of another problem that has already damaged or overtaxed the heart. Knowing these root causes is the first step towards prevention and treatment. The most important conditions that predispose to heart failure are the following:
- Coronary Artery Disease
- Previous Heart Attack
- High Blood Pressure (Hypertension)
- Heart Valve Diseases
- Heart Muscle Diseases (Cardiomyopathy or Myocarditis)
- Congenital Heart Defects
- Abnormal Heart Rhythms (Arrhythmias)
Coronary artery disease and its most dramatic consequence, heart attack, is the number one cause of heart failure. When the arteries that supply the heart (coronary arteries) become blocked, the heart muscle does not receive enough oxygen and is damaged. This damaged area can no longer contract as before and the heart’s pumping power is reduced.
High blood pressure, hypertension, is an insidious enemy. Years of high blood pressure cause the heart to constantly work against a high resistance. Just like driving a car uphill all the time, this tires the heart engine over time. The heart muscle may first thicken (harden), then weaken and enlarge.
Valvular heart disease is also an important cause. The four valves in the heart are like one-way doors that allow blood to flow in the right direction. When these valves are stenotic (incompletely open) or insufficient (incompletely closed), the blood either has difficulty moving forward or escapes backwards. In both cases, the heart has to work much harder to do its normal work and becomes tired over time. The good news is that heart failure, especially due to valve disease, can be significantly improved, sometimes even completely reversed, with successful valve repair or replacement surgery. This is one of the best examples of how life-changing the intervention of a cardiovascular surgeon can be.
In addition, viruses, excessive alcohol consumption, certain medications or genetic causes, cardiomyopathies in which the heart muscle itself is directly affected, congenital heart holes or structural defects and untreated rhythm disorders can also tire the heart over time and lead to failure.
How is Heart Failure Diagnosed?
When you consult a physician with suspected heart failure, a series of investigations are carried out to reach a diagnosis. This process is similar to a detective piecing together clues to reach a conclusion. Each step determines the next step and finally clarifies both the presence and the underlying cause of the disease.
The diagnostic process starts with a detailed conversation with you. The most important clues are your complaints, when they started, what makes them worse or worse, your past health problems, the medications you take and your family history of heart disease. In the physical examination that follows, your doctor will listen to your heart and lungs with a stethoscope to look for abnormal sounds or fluid accumulation (rales). The prominent neck veins, enlarged liver and edema in your legs are important physical signs of heart failure.
After these first steps, some tests are needed to confirm and elaborate the diagnosis. These tests include:
- Blood Tests (especially BNP or NT-proBNP)
- Electrocardiogram (ECG)
- Echocardiogram (Heart Ultrasound or ECHO)
- Chest X-ray
- Effort Test (Stress Test)
- Cardiac Magnetic Resonance (MRI)
- Coronary Angiography
Among the blood tests, the hormones called BNP or NT-proBNP are particularly valuable. The heart releases these hormones when it is under stress and strain. High levels in the blood are strong evidence that complaints such as shortness of breath are caused by the heart. An ECG records the electrical activity of the heart, giving insight into problems such as arrhythmias or previous heart attacks.
However, the “gold standard” and most important tool for diagnosing heart failure is the Echocardiogram. This test uses sound waves to create a live video of the heart. It clearly shows the size of the heart chambers, how well the walls contract and relax, the condition of the valves and, most importantly, the pumping power of the heart (Ejection Fraction – EF). This is the most basic test that allows us to determine the type of heart failure.
A chest X-ray gives an overview of the size of the heart and whether there is fluid accumulation in the lungs. If we suspect that the underlying cause is a blood vessel blockage, we may need a stress test or a more advanced coronary angiography. Angiography provides a kind of road map of the heart vessels, showing blockages precisely and allowing us to decide whether treatments such as bypass surgery are needed.
How to Assess the Severity of Heart Failure?
Once heart failure is diagnosed, we use a staging system to understand how advanced the disease is. This is important both to shape the treatment plan and to make a prediction about the patient’s condition. There are two main classification systems: one based on the structural status of the disease (ACC/AHA Staging) and the other based on the patient’s limitation in daily life (NYHA Functional Classification).
You can think of ACC/AHA staging as a damage report on a building. Once the damage is done, it cannot be undone, but it can be prevented from getting worse with the right interventions. In this system, patients cannot go backwards between stages.
- Stage A: In this stage, there is no heart disease yet, but the person is at high risk of heart failure due to high blood pressure, diabetes or a family history. The aim is to prevent the disease from ever developing.
- Stage B: The person has structural heart disease, such as a previous heart attack or a valve problem, but has not yet developed symptoms of heart failure. The aim is to delay the onset of symptoms.
- Stage C: This is the stage at which most patients are diagnosed. The person has both structural heart disease and symptoms of heart failure such as shortness of breath and edema. The aim of treatment is to control symptoms, reduce hospitalizations and improve quality of life.
- Stage D: This is advanced heart failure. The patient has severe symptoms even at rest, despite all available medication. Symptoms of heart failure stage 4 include persistent shortness of breath, severe fluid retention and extreme fatigue. In this situation, also known as end-stage symptoms of heart failure, advanced treatment options such as heart transplantation or an artificial heart come to the fore.
The NYHA functional classification is more indicative of the patient’s current “fitness”. With effective treatment, a patient’s NYHA class can improve (e.g. from Class III to Class II). Class I refers to the absence of any limitations; Class IV refers to the presence of symptoms even at rest. When these two systems are used together, we get a complete picture of both the structural severity of the disease and its impact on the patient’s daily life. This staging gives a clear idea of the stages of heart failure and helps us plan the treatment journey.
What is the Importance of Lifestyle Changes in Heart Failure Treatment?
Although medicines and advanced technologies are very important in the treatment of heart failure, the foundation and the most solid ground for treatment is lifestyle changes. Without these changes, even the most powerful medications or the most successful surgeries have limited effect. These steps enable the patient to be the captain of their own treatment.
The most basic lifestyle adjustments are:
- Daily weight monitoring
- Severely restricting salt (sodium)
- Keeping fluid intake at the level recommended by the doctor
- Definitely quit smoking
- Stop or severely limit alcohol consumption
- Regular physical activity approved by the doctor
Weighing yourself every morning, after using the toilet and before breakfast, in the same clothes, is the easiest way to notice fluid accumulation in the body. An increase of more than 1.5-2 kilos in a day or 2.5 kilos in a week may be a sign that the body is collecting fluid and the condition is worsening and should be reported to the doctor immediately.
Salt causes water retention in the body. Cutting salt reduces the amount of fluid the heart has to pump, easing its workload. This is one of the most effective ways to control edema and shortness of breath. It is not enough to remove salt from the table; you also need to avoid hidden sources of salt such as processed foods, canned foods, pickles and ready-made sauces. Similarly, your doctor may ask you to limit your daily fluid intake (including water, tea, soup), especially in advanced failure.
Smoking and alcohol are like poison for the heart muscle. Smoking constricts blood vessels and increases the heart’s load, while alcohol can directly weaken the heart muscle. Breaking these habits is a non-negotiable part of the treatment plan.
the idea that “heart patients should not move” is completely wrong. On the contrary, mild-to-moderate exercise, such as regular walking, as permitted by your doctor, strengthens the heart muscle and improves overall fitness and quality of life. Cardiac rehabilitation programs are a great opportunity to learn how to perform these exercises in a safe and supervised manner.
Which medicines are used in the treatment of heart failure?
The answer to the question of how to treat heart failure in modern medicine is an approach known as “guideline-based medical therapy” (GDMT). This means using a combination of several key groups of drugs that have been proven effective in thousands of patients. These drugs play a team game, acting on different mechanisms of the disease. For those wondering if there is a cure for heart failure, the answer is definitely yes, and these drugs are the backbone of treatment.
The main groups of medicines used in treatment are as follows:
- ACE Inhibitors, ARBs or ARNIs
- Beta Blockers
- Aldosterone Antagonists
- SGLT2 Inhibitors
- Diuretics (Diuretics)
ACE inhibitors, ARBs and a newer group of ARNIs reduce the heart’s workload by relaxing blood vessels and blocking harmful hormones. They allow the heart to work more easily. Beta blockers, on the other hand, ease the “stress pedal” on the heart. They slow the heart rate, lower blood pressure and protect the heart from the damaging effects of stress hormones such as adrenaline. These drugs have been proven to prolong life, especially in heart failure with low ejection fraction.
Aldosterone antagonists and SGLT2 inhibitors are groups of drugs that have revolutionized the treatment of heart failure in recent years. Aldosterone antagonists help to remove harmful fluid from the body and prevent scar tissue formation (fibrosis) in the heart. SGLT2 inhibitors, on the other hand, were originally developed as diabetes medication, but have been shown to reduce hospitalizations and deaths due to heart failure, even in patients without diabetes. They are now a cornerstone of treatment.
Diuretics, i.e. diuretics, remove excess salt and fluid from the body through the kidneys. These medications quickly relieve symptoms such as shortness of breath and edema, allowing the patient to “breathe”. However, they do not stop the progression of the disease on their own, but rather are used to control symptoms. The combination of these essential medicines is carefully adjusted by a cardiologist according to the patient’s condition and the type of heart failure.
What Surgical Options Are Available for Advanced Heart Failure?
When medication and lifestyle changes are not enough, or when there is an underlying mechanical problem underlying heart failure that can be corrected, surgical and interventional treatments come into play. These advanced treatments can offer hope, especially in advanced patients, and can sometimes offer a definitive solution to heart failure. As a cardiovascular surgeon, we aim to fix problems in the heart’s “plumbing” or “electrical” system so that the pump can work efficiently again.
The main surgical and interventional options are as follows:
- Coronary Bypass Surgery
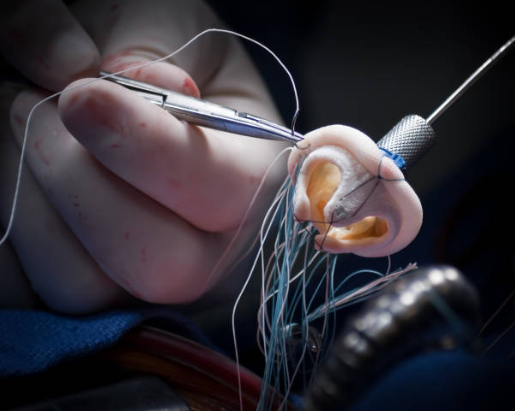
- Heart Valve Repair or Replacement Surgery
- Specialized Pacemakers (ICD and CRT)
- Artificial Heart Assist Devices (VAD)
- Heart Transplant
If the cause of heart failure is severe blockages in the arteries supplying the heart, we create new pathways around these blockages with coronary bypass surgery. As blood supply improves, the heart muscle can become stronger again and signs of failure may regress.
If the problem is a defective heart valve, repairing or replacing it with a new one (mechanical or biological) removes the excessive strain on the heart. After a successful valve surgery, patients’ quality of life and heart function can improve dramatically. This is one of the most positive answers to the question “will heart failure go away?”.
Patients with heart failure are at increased risk of dangerous arrhythmias and sudden cardiac arrest. Special pacemakers called ICDs detect these deadly rhythms and deliver shocks to save lives. Another type of battery, called CRT, corrects the incompatible contraction of the ventricles of the heart, allowing the heart to work more synchronously and efficiently.
In end-stage (Stage D) patients who do not respond to all these treatments, two important options remain: artificial heart assist devices (VADs) and heart transplantation. VADs are mechanical pumps that take over the work of a weakened heart. They can be used as a bridge for patients waiting for a heart transplant, or as a permanent treatment (“destination therapy”) for patients who are not eligible for transplant. Heart transplantation is the ultimate treatment for heart failure, where the diseased heart is replaced with a healthy donor heart.
How to Live with Heart Failure and Long-Term Management?
Being diagnosed with heart failure means turning over a new leaf in your life. It is a chronic condition that needs to be managed, but with modern treatments and the right approach, many patients can live full and active lives. Success in this journey depends on a strong partnership between the patient, their family and the healthcare team.
One of the most common questions asked by patients and their relatives is: “How long does heart failure last?” There is no clear and universal answer to this question. Life expectancy in heart failure varies greatly depending on the stage of the disease, the underlying cause, the patient’s age, other health problems and, most importantly, how well they comply with treatment. For example, the life expectancy of a patient diagnosed at an early stage (Stage B or C, NYHA Class I-II) and who does not interrupt treatment is very different from that of a patient at an advanced stage (Stage D). Compared to the past, today’s treatment options have significantly prolonged life expectancy in heart failure stage 2 and heart failure stage 3. Although life expectancy in heart failure stage 4 is more limited, technologies such as heart transplantation and artificial hearts offer new hope for these patients as well. It is important to remember that statistics are not personal predictions.
There are some key points for successful management in the long term:
- Taking medicines every day, as prescribed, without interruption
- Never neglect doctor and nurse check-ups
- Learn about your disease, your symptoms and the rationale for your treatment
- Establish a support system (family, friends, patient support groups)
- Not hesitating to seek psychological support if necessary
- To evaluate palliative care support to improve quality of life in advanced stages
Compliance with treatment is the key. You should not stop taking medication even when you feel well, as it slows down not only the symptoms but also the progression of the disease. Regular check-ups are essential to make sure your treatment is on track and to make adjustments if necessary.
It is normal to experience feelings of fear, anxiety, anger or depression. Sharing these feelings with people you trust or a professional will ease your burden. Finally, it is important to understand the concept of palliative care correctly. Palliative care is not just end-of-life care. Its aim is to alleviate symptoms such as shortness of breath, pain and fatigue at every stage of the disease and to maximize the quality of life of the patient and family.
Living with heart failure is a marathon. In this marathon, we physicians are your coaches and your biggest supporters. With the right steps, it is possible to successfully complete this race and maintain your quality of life.
Frequently Asked Questions
What is heart failure?
The heart is unable to pump enough blood around the body. This leads to a lack of oxygen and nutrients for the organs.
What causes heart failure?
Many causes can lead to heart failure, including heart attack, hypertension, valve disease, heart muscle disease (cardiomyopathy) and arrhythmias.
What are the symptoms of heart failure?
The most common symptoms are shortness of breath, edema in the legs, fatigue, night cough, abdominal swelling and palpitations.
What are the types of heart failure?
There are three main types: left heart failure, right heart failure and congestive heart failure, which includes both.
Is heart failure chronic?
Usually yes. The disease is progressive and requires long-term treatment.
Is heart failure fatal?
Life expectancy can be prolonged with early diagnosis and appropriate treatment, but can be life-threatening if left untreated.
How is heart failure diagnosed?
It is diagnosed with tests such as ECG, ECHO, chest X-ray, blood tests (BNP), angiography and sometimes MRI of the heart.
Is a cure possible?
A complete cure is usually not possible, but symptoms can be controlled and the progression of the disease can be slowed.
What medicines are used?
ACE inhibitors, beta-blockers, diuretics (diuretics), aldosterone antagonists and in some cases digitalis are used.
How should nutrition be in heart failure?
Salt and fluid intake should be restricted, fatty and processed foods should be avoided, and a heart-friendly Mediterranean diet should be preferred.
Can I exercise?
Mild to moderate exercise is recommended, under the supervision of a doctor. Strenuous activities should be avoided.
Does heart failure progress?
Yes, without treatment or regular follow-up, the disease can progress and heart function can deteriorate.
Could a heart transplant be necessary?
In advanced cases and in treatment-resistant patients, heart transplantation may be an option.
What is the life expectancy?
Life expectancy depends on the severity of the disease, comorbidities and adherence to treatment. Quality of life can be improved with appropriate treatment.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.