Life after heart valve surgery involves adaptation to physical and lifestyle changes that support heart health. Patients experience significant symptom relief but require ongoing monitoring, medications, and lifestyle adjustments to ensure long-term success and prevent complications.
Postoperative care includes anticoagulant therapy, especially for those with mechanical valves, to prevent clot formation. Regular check-ups and echocardiography are essential to evaluate valve function and detect possible infections or arrhythmias. Medication adherence is crucial.
Nutrition and physical activity are vital in recovery. Patients are encouraged to follow a heart-healthy diet, avoid excessive salt, and engage in cardiac rehabilitation programs. Controlled exercise improves stamina and reduces cardiovascular risks after surgery.
Psychological well-being plays an important role in recovery after valve surgery. Support from family, regular medical follow-ups, and stress management techniques help patients regain quality of life. Long-term survival rates improve significantly with comprehensive care.
What kind of an environment awaits me when I open my eyes after surgery?
When you wake up after surgery, you will find yourself in the Intensive Care Unit (ICU). This is a special area where your every moment is closely monitored to ensure that your recovery begins as safely as possible. It is normal and expected to feel a little tired at the beginning, to see unfamiliar voices and screens around you, and even to feel a little confused about where you are. This is a natural part of the process and means you are safe.
The monitors around you and the cables connected to your body may seem a bit daunting at first. But each of these are your guardian angels. These devices monitor your body’s most important functions moment by moment and inform our team.
Here are some of your vital functions that are monitored:
- Your heart rate and rhythm
- Your blood pressure (blood pressure)
- Oxygen level in your blood
- Your body temperature
- Respiratory rate
What is the tube that helps me breathe and when is it removed?
You may initially have a breathing tube (endotracheal tube) placed in your throat to help you breathe in and out until the effects of the surgery and general anesthesia wear off. This tube ensures that your lungs rest and your body gets enough oxygen during these first critical hours. Its presence temporarily prevents you from speaking and may feel slightly uncomfortable. However, you should know that this is only temporary. This tube is usually removed within the first few hours after surgery, or no later than 24 hours after surgery, when you can breathe comfortably and safely on your own.
What Are the Other Wires and Tubes in My Body for?
Apart from the breathing tube, you may also have other tubes in your body. Each of these has an important role to play in your recovery and will be gradually removed as your condition improves.
Other equipment you may encounter in intensive care:
- Chest Tubes (Drains): They are inserted through your chest wall to drain out blood or fluid that may build up at the surgery site or between the lung membranes. This is very important for your heart and lungs to work properly.
- Urinary catheter: Used to precisely measure the amount of urine that is passed out of the body. This allows us to monitor how well your kidneys are working and your body’s fluid balance.
- IV Lines (IV drip): These thin tubes, inserted into veins in your arms or neck, are used to give you essential fluids, painkillers, antibiotics and other important medicines.
- Arterial Line: This special vascular access, usually placed in your wrist, allows us to measure your blood pressure accurately, moment by moment, and take a blood sample if necessary.
How to Manage Postoperative Pain?
Pain after heart surgery is to be expected. However, modern medicine aims to keep this pain at a tolerable level for you. Your pain will be controlled with effective painkillers, which will be administered intravenously or later orally. You play the most important role in this process: Do not hide your pain, do not wait until it becomes unbearable. Honestly telling your nurse about your pain level allows us to provide you with the most appropriate and effective treatment. Having your pain under control directly speeds up your recovery by helping you to breathe, cough and move more easily.
What Does Transition to Normal Service Mean and What Can I Expect?
Usually, after 1 to 2 days in the Intensive Care Unit and after your condition has stabilized, you will be transferred to the regular surgical ward, which is a quieter environment. This is good news that you have overcome an important hurdle in the healing process and that you will now begin to participate more actively in the healing process.
At this stage, you will get to know your care team better. In addition to your surgeon and cardiologist, your nurses and physiotherapists will be your closest supporters during this process.
The main objectives of the service are:
- Early mobilization: Your team will encourage you to sit on the edge of the bed as soon as possible, then take short walks around the room and corridor. Early mobilization stimulates blood circulation and plays a vital role in preventing clots in the leg veins and serious problems such as lung infection.
- Breathing Exercises: Your physiotherapist or nurse will fit you with a special breathing exercise device (commonly known as a triflow) and teach you how to cough effectively. These exercises reduce the risk of pneumonia by removing secretions that build up in your lungs. Supporting the surgical wound in your chest with a small pillow while coughing will significantly reduce the discomfort you will feel.
- Starting Nutrition: You will start with liquid foods and gradually transition to solid foods. It is normal that your appetite is not restored immediately, be patient.
Being discharged from hospital is one of the most exciting steps in your recovery. However, you should remember that the real healing marathon begins at home. It is very important to be patient, understanding and kind to yourself and your body during this period and to accept that healing will take time.
How Long Will My Recovery at Home Take and What Can I Expect?
Like a fingerprint, recovery is a personal and gradual process. Having realistic expectations will help you go through this process in a more stress-free and positive way.
When is a full recovery?
Most of the physical recovery after traditional open heart surgery is usually completed within 4 to 8 weeks. However, it may take 1 to 2 months before you feel fully energized and “like your old self”. One of the most important factors in this process is the union of your breastbone (sternum), which was cut during surgery. It takes about 4 weeks for this bone to heal and consolidate. The main reason for physical activity restrictions at home is to ensure healthy healing of this bone.
Is it normal to feel tired all the time?
Definitely yes. The most common and longest lasting complaint after surgery is fatigue. Your body expends an enormous amount of energy to repair and reconstruct itself from a major surgical trauma. During the first few weeks, it is natural to feel tired after even the simplest activities (e.g. showering, dressing) and to feel the need to rest frequently throughout the day. Your energy level will gradually increase, usually within 3-4 weeks. Don’t compare yourself to others and listen to your body’s signals to “rest”.
How to Care for a Surgical Wound and What are the Symptoms of Infection?
Clean and proper care of your surgical incision is critical to prevent infection and allow the wound to heal better aesthetically.
Follow the instructions given to you exactly. It is essential to keep the wound area clean and dry. Unless your doctor tells you otherwise, you can usually shower a few days after discharge. You can wash the wound gently with warm, soapy water and pat dry with a clean towel, without rubbing. Do not apply any cream, lotion, powder or ointment on the wound without your doctor’s advice. During the first few weeks, you should avoid immersing the wound in water in the bathtub, jacuzzi or pool.
If you notice any of the following symptoms, it could be a sign of an infection and you should call your doctor immediately:
- Increased redness around the wound
- Swelling or increased temperature
- Increased sensitivity to touch
- Yellow-green discharge from the wound
- Foul smelling discharge
- Progressively worsening pain
- Opening of the wound lips
- fever or chills above 38°C
What kind of diet should I follow?
To speed up the healing process, you should adopt a heart-friendly diet rich in protein, vitamins and minerals. It is very important to significantly reduce your salt intake to prevent fluid accumulation in the body (edema) and to keep blood pressure under control.
What should be on your table:
- Fresh vegetables (spinach, broccoli, tomatoes)
- Fruits (especially those with fiber)
- Whole grains (oats, whole wheat bread, bulgur)
- Lean protein sources (skinless chicken, fish, legumes)
- Healthy fats (olive oil, avocado, walnuts)
How Can I Cope with Loss of Appetite and Taste Changes?
Loss of appetite and even changes in the taste of food (e.g. a metallic taste in the mouth) are very common after surgery and can last for several weeks, sometimes several months. Do not let this discourage you. Try to eat small and frequent meals instead of large portions. Healthy snacks, soups and freshly squeezed juices are good options.
What Can I Do for Sleep Problems and Constipation?
Insomnia is one of the most common complaints after surgery. Pain, anxiety and position discomfort can interrupt your sleep. To protect your breastbone, it is recommended to sleep on your back, especially in the first weeks. Try to find a comfortable position by supporting your body with pillows. It is important to know that this condition is temporary and to establish good sleep hygiene (going to bed and getting up at the same time every day, avoiding caffeine and heavy meals before bedtime). Painkillers and inactivity can also cause constipation. Drinking plenty of fluids and adding fibrous foods (dried apricots, oats, green vegetables) to your diet will help solve this problem. If necessary, your doctor may recommend a mild stool softener.
The Invisible Face of Recovery: Are Emotional Fluctuations Normal?
Undergoing major surgery has a profound effect not only on the body but also on the psyche. Accepting the emotional ups and downs you will experience during this period as normal and not hesitating to seek support is as important a part of your overall recovery as physical recovery. It is expected that you will experience sudden changes in your mood after surgery, cry more easily than usual, feel angry or anxious for no reason. These feelings are caused by a combination of many factors such as the stress of the surgery, anesthesia, pain, fatigue and the slow healing process and can last for weeks.
These emotional reactions are completely normal:
- Sudden mood swings
- Crying spells
- Irritability or impatience
- Worry and anxiety
- Forgetfulness or difficulty concentrating
- Temporary loss of interest in previously enjoyed activities
Do not hesitate to talk to your family, friends and care team to help you cope with these feelings. If these feelings do not diminish over time, but instead turn into sadness, hopelessness or helplessness that interferes with your daily life, be sure to tell your doctor. Untreated depression can slow your physical recovery and lower your motivation. Asking for help is not a weakness but an important part of your healing process.
What is the Best Exercise?
The best and safest exercise during recovery is walking. Aim to walk a little more each day than the day before. Start with short walks around the house and as your strength increases, continue outside on a flat surface. Over time, increase both the time and distance you walk. You should not be out of breath while walking, and you should be able to converse comfortably with the person next to you.
What is the Most Critical Restriction (Weight Lifting)?
This is the golden rule of the healing process and must be strictly adhered to. For the first 6-8 weeks, you should not lift, push or pull anything heavier than 5 kilograms (think of two 2.5-liter water bottles) so that your breastbone (sternum) heals completely.
Some daily activities included in this restriction.
- Full grocery bags
- Young children or grandchildren
- Pet food bags
- A full laundry basket
- A heavy backpack or handbag
- Pushing a stuck window
- Pushing open a heavy door
- Using a vacuum cleaner
- Pushing yourself with your arms when getting out of bed or chair
Which Sports and Movements Should I Avoid?
During the first 3 months, you should avoid any sudden and strong strain on your chest and upper arm muscles. During this period, activities such as the following are generally prohibited:
- Tennis
- Golf
- Swimming
- Weight training
- Push-ups or pull-ups
- Mowing the lawn
- Chopping wood
When Can I Drive Safely?
For the safety of your sternum and your ability to react to sudden situations in traffic, you should not drive for the first 4-6 weeks after surgery. To be able to get behind the wheel again, you should feel strong and pain-free enough to brake or steer suddenly and, most importantly, you should not be taking narcotic painkillers (which can cause drowsiness and drowsiness). It is wise to make your first attempts at short distances when traffic is calm and you have someone with you.
How long will my return to work take?
The timing of your return to work depends entirely on the physical requirements of your job. If you have a job that does not require physical effort, such as a desk job, you can usually return to work after 6-8 weeks. However, if you have a physically demanding job that requires heavy lifting, such as construction, agriculture or heavy industry, this may take up to 3 months. This decision should not be rushed and should be made in consultation with your doctor.
Can I Make Travel Plans?
There is no harm in traveling as a passenger in a car after the surgery. However, it is very important to take a break every 1-2 hours and take a short walk to ensure blood circulation on long journeys. Air travel is usually permitted after full recovery, i.e. after about 6-8 weeks and after your doctor has given his/her approval.
What is Cardiac Rehabilitation and Why Should I Attend?
Cardiac rehabilitation is the gold standard in modern medicine for recovery after cardiac surgery and is a step that should never be skipped. It is not just an exercise program; it is also a comprehensive education, counseling and support system designed specifically for you under the supervision of a team of physicians, physiotherapists, dieticians and psychologists.
The benefits of this program are as follows:
- Restore your strength and stamina in the safest way
- Exercise under medical supervision (with monitoring of heart rhythm and blood pressure)
- Learning to manage heart disease risk factors (high blood pressure, cholesterol, weight)
- Adopting heart-healthy eating habits
- Learning stress management techniques
- Find invaluable social and emotional support by meeting other patients going through similar processes as you
Scientific studies clearly show that patients who participate in cardiac rehabilitation programs have a much higher quality of life, a lower risk of developing a new heart problem in the future, and reduced hospital readmission rates.
Which medicines will I need for my new heart valve?
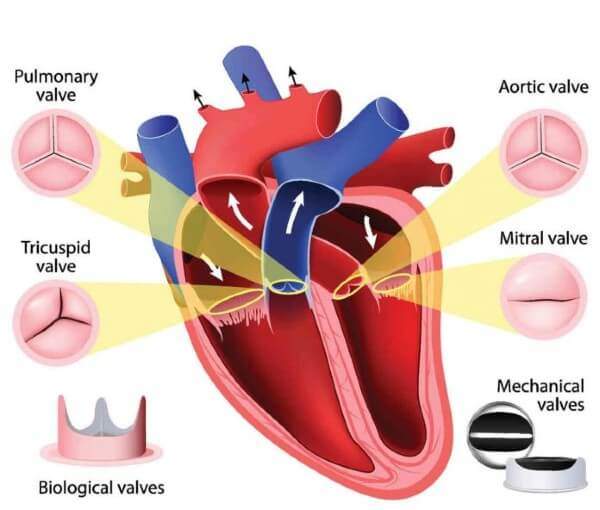
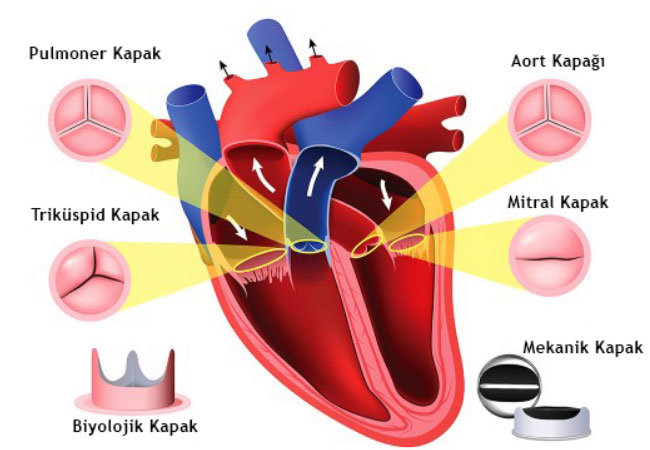
The medicines you will take differ fundamentally depending on the type of valve you have (mechanical or biological). These medicines are vital to protect your new valve and keep your heart working at its most efficient.
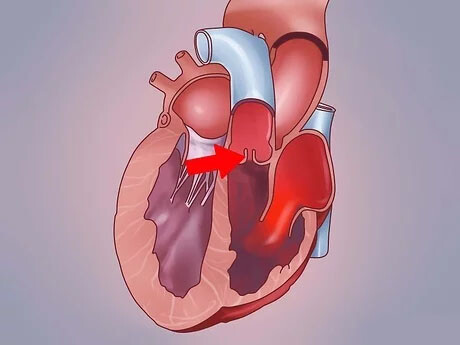
Which Blood Thinner Should I Take If I Have a Mechanical Heart Valve?
Mechanical (metal) lids are preferred because they are extremely durable and long-lasting. However, because they have a metal surface, they carry the risk of blood clots forming on them. To prevent this clot formation and to prevent the clot from being thrown into the brain or other organs and causing serious problems (e.g. stroke), you will need to take a lifelong blood thinner (anticoagulant). The standard and most reliable medicine for this purpose is Warfarin, a Vitamin K Antagonist (VKA). To make sure that the dose of this medicine is in the right and safe range for you, it is imperative that you have a regular INR test, which measures the clotting time of your blood. Your doctor will set a target INR range for you (usually between 2.5 and 3.5) depending on the position of the valve (aortic or mitral). Your medication dose will be fine-tuned according to the results of this test.
Very Important Safety Warning: NOAC/DOAC group drugs known as new generation blood thinners (such as dabigatran, rivaroxaban, apixaban, edoxaban) are not used in patients with mechanical heart valves. These drugs are ineffective in this patient group and their use is dangerous. Your treatment should be with Warfarin only and with regular INR monitoring.
Do I Need Blood Thinners If I Have a Biological (Tissue) Valve?
Because biological (bioprosthetic) valves are made from bovine or porcine heart tissue, they are more compatible with blood and have a much lower risk of forming clots. Therefore, they usually do not require a strong blood thinner such as Warfarin for life. However, during the first 3-6 months of recovery after surgery, a temporary blood thinner (usually low-dose aspirin or sometimes short-term Warfarin) may be required to minimize the risk of clots while the valve suture line and tissue adapt to your body. Once this initial period is over, blood thinners are usually not needed unless you have another heart rhythm disorder that requires the use of blood thinners, such as atrial fibrillation.
How often will my doctor visits and follow-up tests be?
Regular follow-up is essential to ensure that this important investment in your health pays off and is protected. Having surgery does not mean the end of follow-ups, but rather the beginning of a regular follow-up process.
A typical control schedule is usually as follows:
- First check-up in the first 1-2 weeks after discharge
- Second follow-up 6-8 weeks after surgery
- If all is well, a cardiology check-up at least once a year thereafter
In addition to these checks, an Echocardiogram (ECHO), an ultrasound of the heart, is the most important, painless and harmless test used to see how well your new valve is working and whether there are any leaks or narrowing. In the first months after surgery, a baseline ECHO is performed to assess the basic function of your new valve. Thereafter, annual follow-up ECHOs are usually performed, especially to monitor the condition of the biological valves. This test can be repeated earlier if you have any complaints or if there is a change in the examination findings.
You are the best observer of your own health. Learning to listen to your body and recognizing the warning signs of potential problems is vital to detect and intervene at an early stage.
When should I call my doctor or ask for emergency help?
If you experience any of the following symptoms, do not take it lightly, do not wait for it to “go away” and contact your doctor immediately or go to the nearest emergency room.
Symptoms requiring urgent medical attention.
- Chest Pain A feeling of pressure, tightness, burning or heaviness in the chest, different from the pain in your surgical wound.
- Shortness of breath: Shortness of breath that occurs at rest or with very light exertion, increases gradually and makes you unable to talk.
- Palpitations: Feeling that your heartbeat is too fast, too slow or irregular with a misfire.
- Dizziness and fainting: Severe dizziness, blackouts or fainting that occurs when you stand up or suddenly.
- Sudden Weight Gain: Gaining more than 2-3 kilograms in one or two days.
- Swelling: Significant, new swelling in your legs, ankles or abdomen.
- Stroke Symptoms: Sudden weakness or numbness on one side of the body, slurred speech, sliding of the mouth, sudden loss of vision. If you have these symptoms, call 112 immediately.
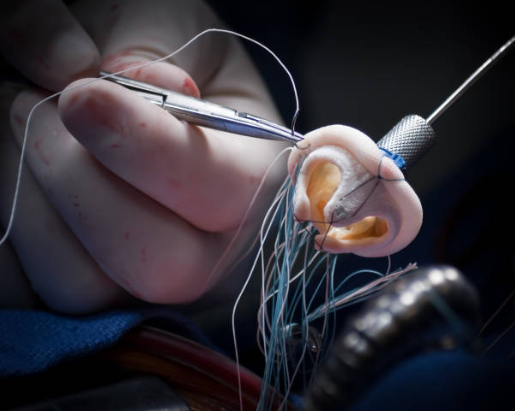
What is Infective Endocarditis and How Can I Avoid This Risk?
Infective endocarditis is a condition in which bacteria that enter the bloodstream, especially on prosthetic heart valves, settle and cause a serious and life-threatening heart infection. Patients with prosthetic heart valves are at a higher lifetime risk for this infection than the normal population. But the ways to avoid this serious risk are simple and must be strictly followed.
What is the Most Important Prevention Method?
The most important, most effective and simplest method of prevention is excellent oral and dental health. Regular brushing, flossing and periodic dental check-ups (usually every 6 months) minimize the risk of bacteria from your mouth entering your bloodstream. Remember, the most common source of endocarditis is untreated tooth and gum problems.
When do you need preventive antibiotics?
Yes, in some cases it is necessary. You need to take prophylactic antibiotics before certain medical procedures where there is a possibility that bacteria in your body can get into the bloodstream.
The most common procedures that require antibiotic protection are:
- All dental treatments (tooth extraction, scaling, root canal treatment, implants)
- Tonsil or adenoid surgery
- Some interventions for the respiratory tract
- Surgical interventions on infected skin or tissues

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.