VSD surgery is performed to correct a congenital heart defect where an abnormal opening exists between the ventricles. This operation closes the septal defect, preventing blood from mixing and ensuring the heart functions more efficiently. Early intervention improves prognosis significantly.
The indications for VSD surgery include severe symptoms such as shortness of breath, recurrent lung infections, or poor growth in children. The timing of surgery is determined by the defect size, the patient’s age, and the severity of pulmonary hypertension. Surgical closure reduces long-term complications.
Postoperative care after VSD surgery involves close monitoring of cardiac rhythm, pulmonary function, and overall recovery. Patients may require temporary medications to support heart function and reduce fluid retention. Early mobilization and nutrition support play a crucial role in healing.
Long-term follow-up after VSD surgery is essential to evaluate heart performance and detect possible arrhythmias or valve disorders. Regular echocardiography and cardiology consultations help ensure a stable outcome. Most patients achieve normal growth, exercise tolerance, and quality of life after surgery.
| Other Names | VSD, interventricular wall defect |
| Affected System | Cardiovascular System (heart) |
| Causes | Congenital; developmental defect of the ventricular septum |
| Types | Perimembranous (most common), Muscular, Inlet, Outlet (supracrystalline) |
| Symptoms | In small defects, usually asymptomatic; in large defects, shortness of breath, growth retardation, frequent respiratory infections, sweating, feeding difficulties |
| Diagnostic Methods | Hearing a murmur (physical examination), ECG, echocardiography, chest x-ray, cardiac catheterization |
| Complications | Pulmonary hypertension, heart failure, endocarditis, Eisenmenger syndrome |
| Treatment Methods | Small defects can be followed; minimally invasive surgical closure in large defects, percutaneous device closure in some cases |
| Age at Intervention | Early in symptomatic patients; can be expected in asymptomatic small VSDs |
| Follow-up and Monitoring | Regular cardiologic evaluation, growth and development monitoring, infective endocarditis prophylaxis |
| Prognosis | In small VSDs, it is usually benign and can close spontaneously; in large VSDs, it is very good after surgery. |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
Stages of VSD Surgery
Closing a ventricular septal defect (VSD) in the heart are the stages of VSD surgery, typically performed with open heart surgery. The first stage of VSD surgery begins with the patient receiving general anesthesia. This ensures that the patient remains painless and immobilized during the VSD surgery. After anesthesia, the surgeon can reach the heart directly by carefully opening the sternum.
In the second stage, you will be connected to a heart-lung machine. This machine pumps oxygen and blood into the body during VSD surgery. In the third stage, the surgeon reaches the septum that separates the right and left ventricles of the heart to find the area of the VSD. Once the surgeon has located the disruption, he or she uses patches or sutures. These patches are usually made from the patient’s tissue or biocompatible materials and adapt to the structure of the heart.
In the fourth stage, the heart is removed from the heart-lung machine and circulation is normalized. In the final stage of the procedure, the surgeon closes the sternum and removes the sutures. After the patient is admitted to intensive care, the heart and blood flow are closely monitored and the recovery process begins. When the stages of VSD surgery are carefully followed, the patient’s heart function becomes healthy and quality of life improves significantly.
Is VSD Surgery Risky?
VSD surgery is a serious surgical procedure that carries some risks, but has a high success rate when performed by a specialized team. Since open-heart surgery involves being connected to a heart-lung machine, complications such as bleeding, infection or rhythm disturbances can occur. VSD surgery, especially in young babies, takes into account the risks associated with anesthesia and the problems that may arise during the healing process.
Cardiac surgeons monitor and address complications such as blood clots or blood pressure changes during VSD surgery. After VSD surgery, the patient undergoes regular check-ups to help the heart adapt to its new condition and the healing process is closely monitored.
Until How Old Does a VSD Close?
VSD, ventricular septal defect, can close spontaneously, usually in children between 2 and 5 years of age. This opening in the heart wall, which occurs at birth, tends to close as the baby grows. During this process, heart doctors assess the likelihood of closure by monitoring the size of the VSD and the rate at which it closes.
Small and medium-sized VSDs may close spontaneously as the heart grows, but large openings usually require surgery. As the child gets older, if the VSD does not close or is progressing very slowly, VSD surgery may be recommended to protect the functioning of the heart. Even if the VSD does not close at an early age, it may become smaller over time and not interfere with the normal functioning of the heart.
What Causes Ventricular Septal Defect (VSD)?
It is usually caused by birth. When the heart chambers do not close completely as the fetus grows, a gap forms between the ventricles. Although the causes of VSD are not known exactly, genetic and environmental factors are thought to be effective.
People with a history of heart disease in their babies are more likely to have a VSD, suggesting that genetic predisposition plays an important role. Certain infections that the expectant mother has during pregnancy, especially viral infections such as rubella, can impair fetal heart development. Factors such as alcohol, drugs or smoking during pregnancy can also increase the risk of VSD.
If the expectant mother has chronic diseases such as diabetes or takes certain medications during pregnancy, this can also lead to VSD formation. To reduce the risk of VSD, it is important to adopt a healthy lifestyle before and during pregnancy and to be under medical supervision. However, the causes of VSD may not be known in all cases, so the baby’s heart health is regularly monitored.
What are the Symptoms of Ventricular Septal Defect (VSD)?
Depending on the size of the hole in the heart and the disruption in blood flow, the symptoms of a ventricular septal defect (VSD) can vary. Larger VSDs put more strain on the heart and can cause a variety of symptoms, while small VSDs are often asymptomatic. One of the most common symptoms is shortness of breath. This can be especially noticeable in babies who have difficulty breathing when crying or feeding.
Another symptom of VSD is growth retardation and children often have difficulty gaining weight compared to their peers because the heart may not carry enough oxygen. Another common symptom of VSD is getting tired quickly and having difficulty playing or doing physical activities. Symptoms of VSD in babies include rapid breathing and frequent sweating, a sign that the heart is working too hard.
How is Ventricular Septal Defect (VSD) Diagnosed?
Hearing heart murmurs during a physical examination is the beginning of a ventricular septal defect (VSD) diagnosis, which is then confirmed by various tests. The patient indicates that the doctor suspects a VSD when they hear an abnormal murmur in the heart with a stethoscope. Echocardiography (ECHO) is the most commonly used method for diagnosing a VSD. ECHO provides a comprehensive image of the heart and shows the impact of disruption on blood flow.
Echocardiography is both effective and safe because it uses sound waves to assess the structure and function of the heart. Large VSDs sometimes require cardiac catheterization. The purpose of this procedure is to measure pressures in the heart to show how blood moves through it. Electrocardiography, also known as electrocardiography, records the heart rhythm and electrical activity. If a VSD is present, abnormal electrical activity in the heart can be observed. A chest x-ray can be used to examine blood flow in the lungs and the size of the heart.
These tests provide detailed information about the size and effects of the VSD and help develop an appropriate treatment plan. Early diagnosis, especially in infants and children, protects heart function and prevents future problems.
What Should Ventricular Septal Defect (VSD) Patients Do?
Patients with ventricular septal defect (VSD) should pay attention to their lifestyle and regularly follow their doctor’s advice to maintain heart health and prevent complications. First of all, regular medical check-ups should not be neglected. During these check-ups, the extent of the heart problems and heart function will be examined and the treatment plan will be changed if necessary. If your doctor has prescribed any medication, it is very important to take it in the prescribed dose and duration.
Care should also be taken with physical activity. Some patients with VSD should avoid intense exercise, but light walks and low-paced activities can improve heart health. Eating healthy foods and avoiding processed foods and salt in daily life is good for the heart. VSD patients need to pay attention to dental hygiene to reduce the risk of infection because dental infections can cause serious problems with the heart.
Stress management is very important for VSD patients because stress can increase the heart load and trigger symptoms. To reduce stress, regular sleep, a balanced diet and, when necessary, breathing exercises or meditation are helpful. VSD patients should completely avoid alcohol and smoking, which can affect heart health. By following these tips, you can protect your quality of life and heart health.
What is VSD Repair?
VSD repair is the surgical closure of an opening between the ventricles of the heart called a ventricular septal defect. This opening causes blood flow between the left and right ventricles of the heart, leading to poor circulation. Over time, the excessive blood flow can increase the pressure on the right side of the heart and cause heart failure. VSD repair is usually performed through open-heart surgery and heart function returns to normal once the opening is closed. During surgery, synthetic patches or the patient’s own tissues are used to completely close the opening. Without early intervention, serious complications such as pulmonary hypertension can occur. Therefore, it is critical to make a surgical decision for VSD repair at the right time. After a successful surgery, the patient’s quality of life is significantly improved and the risk of permanent damage is prevented.
How is VSD Repair Performed?
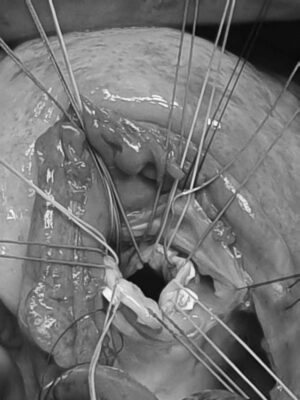
VSD repair is performed as an open heart surgery to close the ventricular septal defect in the heart. During the operation, the patient is first put to sleep under general anesthesia and the chest cage is opened to access the heart. The functioning of the heart is temporarily stopped and circulation is maintained using a heart-lung machine. Depending on the size and location of the defect, the opening is closed using synthetic patches or the patient’s own tissues. This patching is necessary to stop the abnormal blood flow between the right and left ventricles of the heart. After surgery, normal circulation is restored and heart function is restored. After a successful VSD repair, the risk of heart complications is significantly reduced. Timeliness of the procedure is crucial for the patient’s long-term heart health and quality of life.
In Which Situations Can VSD Repair Be Performed?
VSD repair can be performed in the following cases:
-
If there are signs of heart failure: If the heart is overworked by the VSD, heart failure can develop and requires repair.
-
If pulmonary hypertension develops: High pressure blood flow to the lungs causes pulmonary hypertension and requires intervention.
-
Growth retardation: Overworking the heart increases energy consumption, children’s growth can be affected and surgery is required.
-
If the defect is large: Large VSDs usually do not close on their own and surgical repair is recommended for heart health.
-
Heart rhythm disturbances: Prolonged high pressure can cause rhythm problems, in which case the VSD should be closed.
-
Frequent lung infections: Excess blood flow to the lungs increases the risk of infection and repair becomes necessary.
-
Failure to respond to medication: If symptoms cannot be controlled with medication, surgical intervention is inevitable.
-
Other heart anomalies: If there are additional heart problems in addition to the VSD, a combined surgical procedure corrects all the problems.
After Ventricular Septal Defect (VSD) Surgery
| Type of Surgery | Patch closure with open heart surgery or sometimes catheter closure for small VSDs. |
| Recovery Time | 10-15 days after closed minimally invasive surgery, recovery after catheter intervention occurs in a shorter time. |
| Physical Activity | Light walking for the first 10 days; heavy lifting and straining is not recommended if there is an old technique sternum incision. |
| Medication Use | If there are signs of heart failure, supportive medications; sometimes anticoagulants or rhythm regulators may be given. |
| Rhythm Monitoring | Heart blocks or ventricular arrhythmias may be seen rarely, especially after surgery; ECG monitoring is performed. |
| Imaging and Control | Echocardiography is used to monitor cardiac function and residual shunts, if any, after VSD closure. |
| Complications | Residual VSD, heart block, arrhythmia, valvular insufficiency, pulmonary hypertension may be seen rarely. |
| Wound Care | Surgical incision sites should be kept clean; be alert for signs of infection. |
| Nutrition | No special diet is required, but a balanced diet is recommended to maintain heart health. |
| Sexual Activity | It is usually possible within 4-6 weeks once physical competence is achieved. |
| Smoking and Alcohol | Not recommended for people with heart disease; cessation is recommended. |
| Psychological Support | It is especially useful for individuals who had surgery in childhood in terms of adaptation to the life process. |
| Vehicle Use | Once physical recovery is achieved, it is usually possible within 15 days. |
| Controls | Frequent check-ups are recommended during the first year, followed by regular echocardiography and cardiology follow-up annually thereafter. |
Frequently Asked Questions
Until what age does a VSD close?
Small VSDs, especially in muscle tissue, can usually close spontaneously in the first few years of life. The type and size of the hole affect this process. The closure process is monitored with regular physician follow-up; if it does not close, timely intervention is planned.
From which focus is the VSD heard?
The characteristic murmur of a VSD is most clearly heard with a stethoscope in the area just to the left of the sternum. The intensity and propagation of the sound gives us important clues about the type and size of the hole.
Is VSD surgery risky?
As with any surgery, there are certain risks, but VSD closure surgery is one of the most experienced and highly successful procedures in cardiac surgery. Risks are minimized with modern techniques and experienced teams.
Does VSD cause heart failure?
Particularly large and untreated VSDs can tire the heart over time and lead to heart failure. This condition, which causes the heart to overwork, can be prevented with early intervention.
How is VSD diagnosed?
It is first suspected by a typical murmur on examination. Echocardiography (ECHO) is performed for definitive diagnosis and detailed evaluation. ECHO is a painless ultrasound method that shows the location and size of the hole and its effect on the heart.
How many hours does VSD surgery take?
The repair of the hole in the heart usually takes 1-2 hours. The whole operating room process (preparation, anesthesia, discharge) can take 3-4 hours in total. The duration may vary depending on the type and location of the hole. The important thing is to realize a safe and flawless operation.
What are the types of VSD?
VSDs are named according to their location: Most commonly perimembranous (upper part of the wall), followed by muscular (thick muscular part), VSDs close to the inlet or outlet valves. The location of the hole is key in determining the treatment plan.
Where can you hear a VSD murmur?
It is most clearly heard at the lower left edge of the sternum. This sound is an indication of blood flow from the left ventricle to the right ventricle. Small holes can sometimes make a louder sound.
Is VSD genetic?
Genetic predisposition may play a role in VSD formation. The risk increases slightly if there is a family history of congenital heart disease. It is also associated with genetic syndromes such as Down syndrome. However, most VSDs are caused by a combination of many factors (multifactorial) in the womb.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.