Heart wall thickening, also known as myocardial hypertrophy, is a condition where the heart muscle becomes abnormally enlarged. This adaptation is often a response to increased workload or high blood pressure, potentially leading to impaired heart function if untreated.
Symptoms of myocardial hypertrophy include chest pain, shortness of breath, palpitations, and fatigue. In some cases, dizziness or fainting may occur due to reduced blood flow, making early recognition of clinical signs crucial for effective management.
Underlying causes include hypertension, valvular heart disease, and genetic cardiomyopathies. Echocardiography and advanced imaging play a vital role in assessing wall thickness, function, and associated complications in affected patients.
Management strategies involve controlling underlying conditions such as hypertension, prescribing medications to reduce cardiac workload, and in advanced cases, considering surgical options. Lifestyle modifications remain essential to support cardiac health.
| Definition | Thickening of the walls of the heart muscle (especially the left ventricle), usually a process of adaptation to pressure or volume |
| Causes | Prolonged high blood pressure (hypertension), aortic stenosis, athletic heart (physiological in those who do intense sports), cardiomyopathy, genetic predisposition |
| Risk Factors | Hypertension, aging, genetic predisposition, heart valve diseases, obesity, diabetes |
| Symptoms | Generally asymptomatic in the early period; shortness of breath, fatigue, palpitations, chest pain, fainting in the advanced period |
| Diagnostic Methods | ECG, echocardiography (the most important diagnostic method), cardiac MRI, X-ray, blood tests |
| Treatment Methods | Treatment of the underlying disease (hypertension, valvular disease), drug therapy (ACE inhibitors, beta blockers, calcium channel blockers), lifestyle changes, rarely surgical intervention |
| Complications | Heart failure, arrhythmia, sudden cardiac arrest, stroke, coronary artery disease |
| Prevention Methods | Control of hypertension and underlying diseases, healthy lifestyle, regular follow-up and regular use of medications |
What Is Heart Wall Thickening and Why Is It Important?
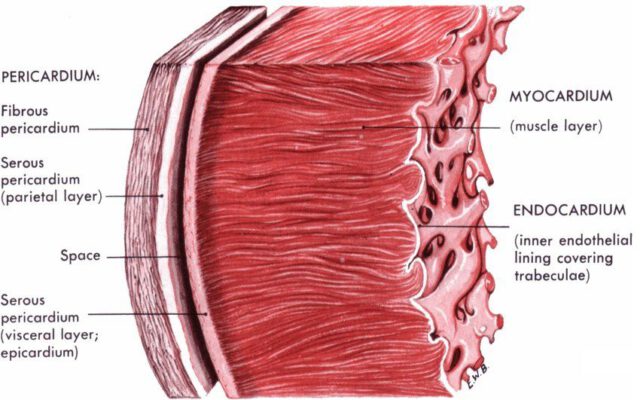
Heart wall thickening is easier to understand in terms of how any muscle in our body works. For example, just as the arm muscles of a person who regularly lifts weights develop and thicken over time, the heart muscle reacts in a similar way when it has to constantly work against a higher than normal load. The walls of the heart, especially those of the left ventricle, which is responsible for pumping blood throughout the body, thicken to accommodate this increased workload and to continue to function. In medical language, we call this condition “myocardial hypertrophy”.
However, there are two main scenarios behind this thickening and differentiating between them is the basis of treatment.
The first is when the heart thickens in response to another condition. This is the most common presentation and is often referred to as “Left Ventricular Hypertrophy (LVH)”. Here, the heart muscle is actually healthy, but it develops a defense mechanism because it is constantly working against resistance due to an external factor such as high blood pressure or a valve disease.
The second is when the problem is caused directly by the heart muscle itself. This is called “Hypertrophic Cardiomyopathy (HCM)”. There is no underlying blood pressure or valve problem; the problem is that the heart muscle cells tend to grow and thicken abnormally on their own, often through genetic inheritance.
The difference between these two scenarios is like night and day. One is a potentially reversible condition once you eliminate the cause, while the other is a disease of the heart muscle that requires a lifetime of careful monitoring and management. So when you hear “thickening of the heart wall”, the next step is always to find the answer to the question “Why?”.
Which Conditions Increase the Risk of Heart Wall Thickening?
Understanding why your heart wall thickens is like solving the most important piece of the puzzle. The reasons differ according to the two main pathways mentioned above.
The most common causes leading to a condition where the heart thickens as a reaction (LVH) are:
- High blood pressure (Hypertension)
- Aortic valve stenosis
- Intense and heavy athletic training (Athlete’s Heart)
The most common cause is high blood pressure. When your blood pressure is consistently high, your heart works like it is pushing against a wall to get blood into your blood vessels. This years-long struggle leads to fatigue of the heart muscle and thickening of the walls. Aortic valve stenosis is a narrowing of the heart’s outlet. As the heart tries to push the same amount of blood through a narrow door, it contracts with enormous pressure, which leads to thickening of the walls. The athlete’s heart is not a pathological condition. It is the physiological enlargement and some thickening of the heart of elite-level athletes to meet the body’s increased oxygen demand. This condition is usually not a risk but needs to be differentiated from diseases such as CDC.
When the heart muscle itself is diseased (CDM), the main cause is almost always genetic. Here, the problem is caused by a change in the genes that make up the heart muscle proteins, i.e. a mutation. This genetic inheritance is usually passed on in the family in an “autosomal dominant” way, meaning that if one of the parents has this genetic trait, there is a P chance that it will be passed on to the child. Therefore, when a person is diagnosed with CDC, it is vital that other members of the family are also checked.
What Signals Does Our Body Give for Heart Wall Thickening?
Thickening of the heart wall can be a very insidious condition. Many people go through life without feeling any abnormalities, especially in the early years of the disease. Symptoms usually start to appear gradually, when the heart’s function can no longer tolerate the additional load. There are some important signals that your body can send you.
Some of the most common symptoms of heart wall thickening are as follows:
- Shortness of breath with exertion
- Chest pain or feeling of pressure
- Irregular or strong heartbeat
- Sudden dizziness
- Fainting (syncope)
- Tired more quickly than usual
- Swelling in the legs or ankles
Let’s explain a little more about what these symptoms mean. Shortness of breath is usually the first and most common sign. It is typical to feel short of breath when climbing stairs, walking uphill or doing something you used to do easily. As the condition progresses, you may also experience this problem when you lie in bed at night or wake up with shortness of breath. Chest pain is a feeling of tightness or pressure, usually caused by an inability to meet the heart’s increased oxygen demand during activity.
Palpitations can be described as your heart suddenly misfiring, feeling like a bird flapping its wings, or beating much stronger and faster than normal. This may indicate an underlying arrhythmia. Dizziness and fainting, especially during or immediately after exercise, is a much more serious warning and should not be ignored. Because this can be an indication that the blood flow from the heart to the brain is momentarily reduced.
How Is Heart Wall Thickening Diagnosed Step by Step?
An accurate and complete diagnosis is the roadmap for an effective treatment. The process begins with a detailed interview with you. We will try to understand when and how your symptoms started and whether you have a family history of a similar condition. A “murmur” that we can hear when we listen to your heart with a stethoscope during a physical examination can give the first clue that there is a problem with blood flow.
Following this preliminary assessment, we use a series of diagnostic tests to clarify the situation. The main methods used in the diagnostic process are:
- Echocardiogram (ECHO)
- Electrocardiogram (ECG)
- Cardiac MRI (Magnetic Resonance Imaging)
- Holter monitor
- Effort (stress) test
- Genetic tests
Each of these tests has a different purpose. An echocardiogram (ECHO), an ultrasound of the heart, is the cornerstone of diagnosis. We take a live movie of your heart using sound waves. This allows us to measure the thickness of your heart walls in millimeters, assess the strength of your heart’s contraction and relaxation, check your valves and clearly see if there is a stenosis blocking blood flow. An electrocardiogram (ECG) records the electrical activity of the heart on a piece of paper. Thickening of the heart wall can leave typical traces on the ECG and give us valuable information about rhythm disturbances.
In more complex or borderline cases, Cardiac MRI comes into play. This test creates a three-dimensional map of your heart. It provides very detailed images showing the structure of the muscle tissue, the exact location of thickening and even whether there is scar tissue (fibrosis) within the muscle. If you have occasional palpitations, we use a small, portable device called a Holter monitor that records your rhythm for 24 or 48 hours. An effort test allows us to measure your heart’s response to stress while you walk on a treadmill. Especially if CDC is suspected or there is a family history of the disease, genetic testing can help to clarify the genetic origin of the problem.
Is Heart Wall Thickening Really a Dangerous Condition?
It is important to answer this question honestly: Yes, thickening of the heart wall is a condition that can be dangerous if neglected and should be taken seriously. Over time, a thickened and stiffened heart muscle is no longer able to both pump and relax as well as it used to. This brings with it the risk of a number of serious complications.
There are major risks that can occur if left untreated:
- Heart failure
- Rhythm disorders (especially Atrial Fibrillation)
- Stroke (Paralysis)
- Heart muscle ischemia (insufficient blood supply to the heart)
- Sudden cardiac death
Heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs and causes symptoms such as shortness of breath, fatigue and swelling in the legs. Rhythm disorders occur when thickened muscle tissue disrupts the heart’s sensitive electrical system. The most common of these is Atrial Fibrillation, in which the atria of the heart vibrate irregularly and rapidly. This can lead to clot formation in the heart, which can throw a clot into the brain, resulting in a stroke.
The most feared risk is sudden cardiac death. This is a sudden fatal arrhythmia resulting in cardiac arrest, especially in young people with HCM, even when there are no apparent symptoms. It is important to emphasize that this risk is low in the general population, but its very existence explains why these patients need to be followed very closely and why we take special precautions to protect at-risk individuals. Knowing these risks is critical, not to be afraid, but to understand the importance of treatment and to take the necessary steps in a timely manner.
What Treatment Methods Are Available for Thickening of the Heart Wall?
The good news is that thickening of the heart wall is a manageable condition and there are a wide range of effective treatment options available today. The treatment plan is as individualized as a fingerprint. The cause, type and severity of the thickening, as well as your general state of health, will determine how we proceed. Treatment can generally be categorized under three main headings.
Lifestyle and Dietary Habits
This is the pillar of treatment and the part where you are largely in control. Some positive changes in your life can completely change the course of the disease, especially in high blood pressure-related LVH. Here are the key points to focus on:
- Reduce salt
- Mediterranean-type nutrition
- Maintaining ideal weight
- Proper and regular exercise
- Definitely quit smoking
- Stress management techniques
- Limiting alcohol consumption
Reducing the salt in your diet is the simplest and most effective way to lower blood pressure. Avoiding processed foods, pickles and ready-made sauces is a good start. A diet rich in fresh vegetables, fruit, olive oil, fish and whole grains is your heart’s best friend. Excess weight is a burden on your heart and losing weight directly alleviates this burden. Regular exercise, such as walking or swimming, recommended by your doctor, strengthens your heart. However, it is important to remember that CDC patients should avoid competitive and heavy sports.
Drug Treatments
Medicines are used to make your heart’s work easier, reduce your symptoms and prevent dangerous complications. There are major groups of medicines used for this purpose:
- Beta blockers
- Calcium channel blockers
- ACE inhibitors / ARBs (Blood pressure medicines)
- Myosin inhibitors
- Blood thinners (Anticoagulants)
- Diuretics (Diuretics)
Beta blockers and calcium channel blockers allow the heart to rest by slowing the heart rate and slightly reducing the force of contraction. Blood pressure medications control blood pressure by getting to the root of the problem, especially in LVH. Myosin inhibitors are a new generation of smart drugs developed specifically for HCM, directly targeting the mechanism of excessive contraction. In patients with arrhythmia, blood thinners can be used to reduce the risk of stroke and diuretics can be used to remove fluid accumulation in the body.
Interventional and Surgical Treatments
In selected patients in whom medication and lifestyle changes are inadequate, especially in cases of obstructive CDM (obstructive CDM), we resort to more advanced and effective methods.
Prominent among these methods are the following:
- Septal Myectomy (Open heart surgery)
- Alcohol Septal Ablation (Angio-like method)
- ICD (Pacemaker / shock device)
- Heart Transplant
Septal myectomy is an open heart surgery performed by an experienced surgeon. During the operation, we carefully shave away the excess muscle tissue that blocks blood flow with the precision of a sculptor. This widens the pathway inside the heart, blood flows freely and the patient’s symptoms are largely eliminated. This is the “gold standard” treatment for the right patient. Alcohol septal ablation is an alternative for patients at high risk of surgery. In the angiography laboratory, a small amount of alcohol is injected into the blood vessel supplying the thickened muscle, causing the area to shrink in a controlled manner. The ICD is not a treatment method but life insurance. This device, which we implant under the skin in patients at risk of sudden death, saves lives by delivering a shock when it detects a dangerous rhythm. Heart transplantation is a door of hope for a very small number of patients with end-stage heart failure, when all other methods have been exhausted.
Is Heart Wall Thickening Completely Reversible?
The answer to this question depends on the two main scenarios we outlined at the beginning of the journey.
If your heart wall thickening is Left Ventricular Hypertrophy (LVH) due to a cause such as high blood pressure, the answer is promising: Yes, it can improve. When we effectively control the underlying cause – blood pressure – the constant pressure on the heart is removed. Over time, the heart adapts to this, gradually becoming thinner and returning to its old, normal structure. This is the best proof of how rewarding treatment adherence can be.
If your condition is Hypertrophic Cardiomyopathy (HCM) of genetic origin, this feature in the muscle itself does not completely “disappear”. This is because it is a trait that you carry in your genes. However, this does not mean that you should despair. Modern treatments can stop the progression of the disease, completely control the symptoms and minimize the risks. The goal is not to eradicate the disease, but to help you live a long, healthy and high-quality life with it, and today we can do this with great success.
Frequently Asked Questions
What is heart wall thickening?
It is when the walls of the heart muscle become thicker than normal. In medicine, it is often called “left ventricular hypertrophy”.
What does this mean?
It indicates that the heart is trying to compensate for a situation that causes it to exert more force. But in the long term it can impair heart function.
Why does it occur?
The most common cause is hypertension. Heart valve diseases, athlete’s heart, obesity and genetic diseases are also among the causes.
What are the symptoms?
Initially it is asymptomatic. In the advanced stage, shortness of breath, palpitations, chest pain, fatigue and fainting may occur.
Is thickening of the heart wall dangerous?
Yes, over time it can lead to serious consequences such as heart failure, arrhythmias and sudden cardiac arrest.
How is it diagnosed?
Echocardiography (ECHO) is the most commonly used test to measure heart wall thickness. ECG and MRI may also be supportive.
What is the difference with an athlete’s heart?
Thickening of the athlete’s heart is physiological and temporary. Pathologic thickening is due to heart disease and is risky.
What happens if left untreated?
Complications such as heart failure, valvular disease, stroke and sudden death can develop.
What are the treatment methods?
Depending on the underlying cause, blood pressure control, weight management, medication and sometimes surgical methods are used.
Do drugs reduce thickening?
Some blood pressure medications (especially ACE inhibitors and ARBs) can reduce heart wall thickness.
Could this condition be genetic?
Yes, especially in genetic diseases such as hypertrophic cardiomyopathy, the thickness of the heart wall can be prominent.
Is it safe to exercise?
People with thick heart walls should exercise under the supervision of a doctor. Intense exercise may need to be avoided.
Can heart wall thickening regress?
Yes, the thickening may partially regress if the underlying cause is controlled.
Does diet affect this condition?
A balanced, heart-friendly, salt-free diet contributes indirectly by reducing blood pressure and thus heart burden.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.