Mitral valve regurgitation is a condition where the heart’s mitral valve does not close fully, allowing blood to flow backward into the left atrium. This leads to reduced cardiac efficiency, fatigue, and in advanced cases, heart failure. Early recognition of symptoms is essential for timely treatment.
Common signs of mitral valve insufficiency include shortness of breath, irregular heartbeat, palpitations, and swelling in the legs. Fatigue and exercise intolerance are frequently reported. Severe regurgitation may cause pulmonary hypertension and atrial fibrillation, complicating the clinical course.
Diagnosis is primarily made using echocardiography, which shows valve structure and regurgitation severity. Additional tests such as chest X-ray and electrocardiogram support evaluation. Differentiating symptoms from other cardiac disorders ensures accurate treatment planning and avoids unnecessary delays.
Treatment ranges from medication for symptom control to surgical or transcatheter repair in severe cases. Regular follow-ups are crucial to monitor disease progression. Early intervention significantly improves survival rates and quality of life in patients with mitral valve regurgitation.
| Types | Primary (organic) insufficiency: disruption of valve structure; Secondary (functional): as a result of left ventricular dysfunction |
| Causes | Mitral valve prolapse, rheumatic disease, infective endocarditis, ischemic heart disease, cardiomyopathy |
| Risk Factors | Advanced age, rheumatic fever, previous heart infection, coronary artery disease, heart failure |
| Symptoms | Shortness of breath, fatigue, palpitations, orthopnea, paroxysmal nocturnal dyspnea, ankle edema |
| Diagnostic Methods | Murmur on physical examination, transthoracic and transesophageal echocardiography, ECG, chest radiography, CT/MR |
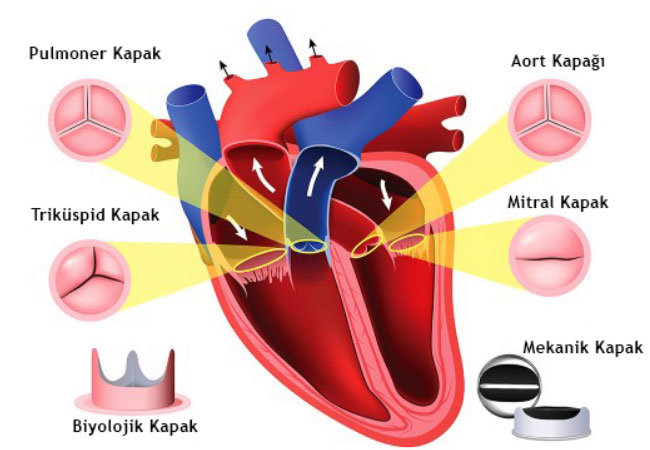
| Treatment Options | Medical treatment (ACE inhibitors, diuretics), mitral valve repair or replacement (surgical-minimal axillary-subcutaneous) |
| Complications | Left atrial and ventricular enlargement, atrial fibrillation, pulmonary hypertension, heart failure |
| Protective Measures | Control of risk factors, regular echocardiography follow-up, prevention of infections, early diagnosis and follow-up |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Mitral Valve Insufficiency?
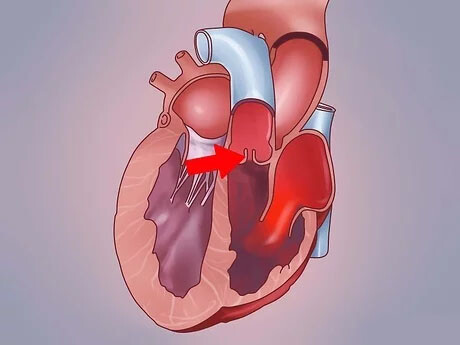
In a healthy heart, blood flow is like a one-way highway. When the left ventricle contracts, the mitral valve closes tightly, allowing all the blood to flow forward, through the aorta and out into the body. This provides our organs and tissues with the oxygen and nutrients they need.
In mitral valve insufficiency, this order is disrupted. Because the valve leaflets do not come together properly, during contraction some blood cannot go forward as it should and escapes backwards into the left atrium. This backward leakage accumulates in the left atrium, increasing the pressure in this chamber and causing it to enlarge over time. This increased pressure is reflected backwards into the pulmonary vessels, like a river overflowing its bed. This increase in pressure in the lungs is the main cause of shortness of breath.
Meanwhile, the left ventricle is not idle. It works twice as hard, both to send blood to the body and to cope with the volume of escaping blood. Over time, this endless overwork causes the heart muscle to tire, expand (like a balloon that is constantly inflated) and eventually lose its contractile strength. At this point, what is initially only a valve problem can turn into a heart failure picture that affects the whole heart.
What Types of Mitral Valve Insufficiency Are There?
To properly understand and treat mitral valve insufficiency, we categorize it in different ways. This helps us to draw our roadmap. We basically use two main classifications.
The first is according to the source of the problem:
- Primary Failure
- Secondary Failure
In primary insufficiency, the problem is directly in the valve itself. In other words, there is a deterioration in structures such as the valve leaflets, the strands that hold them together or the valve ring. This can be due to age-related wear and tear, calcification or congenital looseness of the valve structure (mitral valve prolapse).
In secondary failure, the valve is initially innocent; its structure is completely normal. The problem lies elsewhere in the heart. The left ventricle is enlarged and misshapen, usually as a result of a heart attack or heart muscle disease. This shifts the floor on which the normal lid sits, preventing the leaflets from touching each other and causing leakage.
The second classification is based on the rate of development of the disease:
- Acute Failure
- Chronic Insufficiency
Acute failure, as the name suggests, starts suddenly and violently. It is caused by a sudden perforation or rupture of the valve, usually triggered by an emergency such as a heart attack or infection. Since the heart has no time to prepare for this condition, the picture is very severe and requires urgent surgical intervention.
Chronic failure is the most common type. It develops slowly and insidiously over many years. The heart takes a long time to adapt to this slow leakage and patients may not feel anything for years. By the time symptoms appear, the disease is usually at a certain stage.
What Causes Mitral Valve Failure and Who is at Risk?
There are many factors that play a role in the occurrence of mitral valve insufficiency. A more accurate approach would be to divide these causes into primary and secondary insufficiency.
The most common causes leading to primary insufficiency, i.e. conditions that directly disrupt the structure of the valve, are
- Mitral valve prolapse (loosening of the valve leaflets)
- Degenerative valve disease (age-related wear and tear)
- Rheumatic fever (previous “beta” infection)
- Infective endocarditis (valve infection)
- Congenital valve anomalies
- Connective tissue diseases such as Marfan syndrome
- Chest trauma
- Radiotherapy to the chest area
Secondary insufficiency is caused by heart disease that impairs the function of the intact valve. Examples of these situations:
- Heart attack (Ischemic cardiomyopathy)
- Heart muscle diseases (dilated cardiomyopathy)
- Abnormal thickening of the heart muscle (hypertrophic cardiomyopathy)
- Prolonged and untreated high blood pressure
- Rhythm disorders such as atrial fibrillation
Some conditions increase the risk of developing mitral valve insufficiency. The most important of these risk factors are:
- Advancing age
- Male gender
- Past history of rheumatic fever
- Presence of coronary artery disease
- High blood pressure
- Diabetes
Knowing these causes and risk factors is of great importance both for developing prevention strategies and for asking the right questions during the diagnostic process.
Can Mitral Valve Failure Kill? What is Life Chances?
The ultimate goal of all efforts in the treatment process is to give the patient not only a longer life, but also a quality and normal life. So, can mitral valve insufficiency kill? The answer to this question depends on the right intervention at the right time. Untreated severe mitral regurgitation can lead to heart failure and death. However, thanks to modern treatment methods, it is possible to completely change this picture.
Patients who undergo successful mitral valve repair surgery at an experienced center, especially for degenerative (primary) regurgitation, before serious damage to the heart has occurred, have excellent long-term outcomes. Numerous scientific studies have shown that the life expectancy of these patients is on par with that of healthy individuals of their age and gender. This means that a successful repair can remove the risk of the disease and give you a normal life expectancy.
What Should People With Mitral Valve Insufficiency Pay Attention To?
Lifestyle changes, especially dietary habits, are one of the most important answers to the question of what to watch out for with mitral valve insufficiency. While the right choices won’t fix the valve leak, they can help you keep your symptoms under control and improve your quality of life by easing the burden on your heart.
The most critical point is salt (sodium) restriction. You can think of salt as a sponge that holds water in the body. Excess salt consumption increases blood volume, making the work of your already tired heart even harder, raising blood pressure and triggering shortness of breath and edema.
Here are some practical points to consider in your diet:
- Remove the salt shaker from the table.
- Avoiding processed and packaged foods.
- Limit canned food, pickles and charcuterie.
- Ask for your food to be prepared without salt when eating out.
- Read food labels and choose “low sodium” products.
- Flavoring food with spices, herbs and lemon instead of salt.
Your doctor may also ask you to limit your fluid intake, especially if you have advanced heart failure. The easiest way to monitor your body’s fluid balance is to weigh yourself every morning at the same time and under similar conditions. If you notice an increase of more than 2-2.5 kilos in a few days, this may be a sign of fluid accumulation in the body and you should report the situation to your doctor.
Can People with Mitral Valve Insufficiency Play Sports Safely?
the answer to the question “Can people with mitral valve insufficiency do sports?” is yes, depending on the stage of the disease and the individual’s condition. Instead of a sedentary life, a tailor-made exercise program approved by your doctor is very beneficial for both your physical and mental health.
Regular exercise improves overall heart health and maintains your muscle strength. It also acts as an “early warning system” for you. A person who walks regularly will notice much earlier that he or she becomes short of breath at a distance he or she used to walk comfortably. This is an important clinical sign that the disease is progressing.
However, the exercise plan should be personalized:
- Those with Mild to Moderate Failure: Patients without symptoms and with normal heart function can usually participate in most activities. Activities such as brisk walking, swimming, cycling and yoga are generally safe.
- Those with Severe Failure: Restrictions are needed in this group. Especially sports that are competitive and require heavy and sudden effort should be avoided. The aim is to maintain a basic level of activity without overstressing the heart.
Always consult your doctor before starting any program. It is very important to listen to your body’s signals during exercise. If you experience any of the following danger signals, stop exercising immediately and talk to your doctor:
- Unexpected or excessive shortness of breath
- Pain, pressure or discomfort in the chest, arm or jaw
- Feeling dizzy or lightheaded
- Eye darkening
- Severe palpitations
What are the Symptoms of Mitral Valve Failure?
Mitral valve insufficiency can live in your body like a silent guest for many years. The heart works extraordinarily hard to compensate for the increased workload and you don’t even notice it. But over time, as the heart’s compensatory mechanisms tire, the disease begins to manifest itself with specific signals.
The most common symptoms of mitral regurgitation are as follows:
- Shortness of breath
- Constant feeling of fatigue and exhaustion
- Palpitations
- Swelling in the feet, ankles or legs (edema)
- Dry cough, especially at night
- Dizziness
- Rarely chest pain
Among these symptoms, shortness of breath and fatigue are the most common and the earliest to appear. Shortness of breath, which initially only manifests itself as difficulty climbing stairs or hills, may become noticeable as the disease progresses, even when walking in a straight line and even when resting. Waking up at night with shortness of breath or being unable to sleep on your back and only being comfortable with a few pillows are important signs that indicate the seriousness of the disease.
Palpitations are usually a sign of a rhythm disorder called “atrial fibrillation”, in which the heart works irregularly. It can feel like the heart misfiring, like a bird flapping its wings. Swollen feet and coughing are indicators that fluid is beginning to accumulate in the body and lungs, meaning that the heart’s pumping power is insufficient. Any of these symptoms, especially if they have just started or are getting worse, should be taken seriously and a doctor should be consulted.
How is Mitral Valve Insufficiency Diagnosed?
Our process of diagnosing mitral valve insufficiency starts with listening to the patient’s history and is confirmed by the imaging techniques offered by modern medicine. The steps we take in this process are to confirm the presence of the disease, determine its severity and chart the most appropriate course of treatment.
The first step in the diagnostic process is to listen carefully and examine your heart with a stethoscope. A leak in the valve produces a characteristic sound called a “murmur” and hearing this sound is the first sign that leads us to suspect mitral valve insufficiency.
The main diagnostic tool we use to confirm our suspicions and clarify the situation is Echocardiography (ECHO), an ultrasound of the heart. This painless and harmless test gives us invaluable information. The main points we evaluate with echocardiography:
- Detailed examination of the cover structure
- Defects in leaflet movement and closure
- Determination of the amount of escaping blood (degree of insufficiency)
- Dimensions of the heart chambers
- Contractile force and pump function of the heart
Echocardiography allows us to classify the degree of failure as mild, moderate or severe. This classification directly affects our treatment decision and timing. Most of the time a standard ECHO through the chest wall is sufficient, but sometimes we may need a Transesophageal Echocardiography (TEE) through the esophagus to get a closer and clearer view of the valve.
In addition to these basic tests, we may order other tests to support the diagnosis and assess your overall heart health.
Electrocardiogram (ECG): Evaluates heart rhythm.
Chest X-ray It shows the size of the heart and the condition of the lungs.
Effort Test: It measures whether symptoms occur with exertion and how your heart responds to the load.
Cardiac MRI: It is an advanced imaging technique that measures the amount of leakage and heart function very precisely, especially in cases where ECHO findings are not clear.
1,2,3-4 Degree Mitral Valve Insufficiency
The degrees of mitral valve insufficiency are handled in 4 levels and 1st and 2nd degree mitral valve insufficiency is usually tried to be kept under control with patient follow-up. 3. in cases of mitral valve insufficiency of grade 4 and grade 4, patient treatment should be started as soon as possible.
The degree of insufficiency is important in terms of treatment in mitral valve disorders, which can be caused by genetic causes, impaired function of the mitral valve later in life after febrile illnesses as a child, or congenital causes.
| 1. Degree (Light) | Jet area is small in the left atrium (<4 cm² or <20% atrial area); no symptoms; may be generally physiologic |
| 2. Grade (Medium) | Jet area is moderate (-40 atrial area); mild symptoms may be present; ventricular function is preserved |
| 3. Degree (Intermediate-Advanced) | Jet area is large (>40% atrial area); marked symptoms may begin; left ventricular enlargement may be observed |
| 4. Degree (Advanced) | Jet fills the entire left atrium, may extend into the vena pulmonaris; severe symptoms (dyspnea, fatigue, edema); high risk of left heart failure |
1.Degree Mitral Valve Insufficiency
First-degree mitral valve insufficiency is a level of insufficiency that does not cause significant complaints in patients and can be found in many people. 1.it is sufficient for individuals with mitral valve insufficiency to be checked periodically. 1.no treatment is given for the level of insufficiency.
2.Degree Mitral Valve Insufficiency
2. mitral valve insufficiency of the second degree may cause some mild symptoms in individuals. Second-degree mitral valve insufficiency is usually found incidentally. Depending on the patient’s age, general health and history, follow-up of second degree mitral valve insufficiency is necessary. After echocardiography and other tests deemed necessary by the physician, the patient is asked to come for follow-up visits at regular intervals.
grade 3-4 Mitral Valve Insufficiency
Levels 3 and 4 are risky in mitral valve insufficiency. It should be treated without delay as it can lead to failure in the left side of the heart. Since mitral valve regurgitation is now successfully treated, patients with advanced regurgitation need not be alarmed. However, delaying treatment can lead to progression of the insufficiency and life-threatening consequences. 3. patients with grade 4 mitral valve insufficiency may experience breathing problems, fatigue and irregular heartbeat. Although advanced mitral valve insufficiency can be controlled with medication in some cases, surgical treatment may be necessary in the future.
Degrees of mitral valve insufficiency can progress if not treated in time. 1. in cases of grade 2 and grade 2 insufficiency, regular follow-up is necessary. 3. for mitral valve insufficiency at grade 2, treatment is decided after detailed examinations are performed. Patients with mitral valve insufficiency grade 4 usually require mitral valve surgery (valve repair or replacement). This statement can be described as an answer to the question of whether mitral valve insufficiency kills patients, which patients are anxious about and frequently ask.
What Problems Does Untreated Mitral Valve Insufficiency Cause?
Moderate to severe mitral valve insufficiency is like a time bomb. Although initially silent, left untreated it can cause serious, irreversible damage to the heart and body. Constantly overloading the heart leads to a number of dangerous complications.
The most important problems that can occur when left untreated:
- Atrial Fibrillation (AF)
- Stroke (Paralysis)
- Pulmonary Hypertension
- Congestive Heart Failure
- Sudden Cardiac Death
Atrial Fibrillation is when the enlarged left atrium loses its normal rhythm and begins to vibrate irregularly and rapidly. While this condition itself causes palpitations and fatigue, its main danger is that it prepares the ground for clot formation inside the heart. When these clots break off and block the brain vessels, it can result in a stroke, which can lead to permanent disability.
Pulmonary Hypertension is an increase in blood pressure in the pulmonary arteries to dangerous levels. This exacerbates shortness of breath and eventually leads to the failure of the right side of the heart.
The last and most feared complication is Congestive Heart Failure. At this stage, the heart muscle, tired from years of overwork, gives up and is no longer able to pump enough blood to meet the body’s needs. This is a life-threatening condition that severely reduces the patient’s quality of life. For these reasons, we say “timing is everything” in mitral valve insufficiency. An intervention at the right time can prevent all these bad scenarios from happening.
Which Methods are Used in the Treatment of Mitral Valve Insufficiency?
The treatment of mitral valve insufficiency is a completely individualized process with no single formula. When making the treatment decision, we evaluate many factors such as the severity and type of the disease, the patient’s age, general health status and most importantly, structural changes in the heart. Our aim is to protect the heart from further damage, improve quality of life by eliminating symptoms and, where necessary, permanently fix the mechanical problem with the valve.
Our treatment approach can basically be categorized under four main headings.
Medical Monitoring and Lifestyle Changes
In patients with mild insufficiency and no symptoms, we usually follow a strategy we call “watchful waiting”. This means that we closely monitor the course of the disease with regular check-ups and echocardiography. During this process, we recommend some lifestyle changes to all our patients to protect their heart health:
- Reducing salt consumption
- Maintaining a healthy weight
- Quitting all tobacco products
- Limiting alcohol consumption
- Keeping high blood pressure under control
- Regular physical activity approved by the doctor
Medication Therapy
Medicines cannot repair a damaged valve. However, they provide important support by easing the workload of the heart, controlling symptoms and reducing the risk of complications. It is a method we use especially in patients who are too early for surgery or who are at high risk of surgery. The main groups of medicines we use:
- Diuretics (Diuretics)
- ACE inhibitors and ARBs (blood pressure regulators)
- Beta blockers (drugs that slow down the heart rate)
- Anticoagulants (Blood thinners)
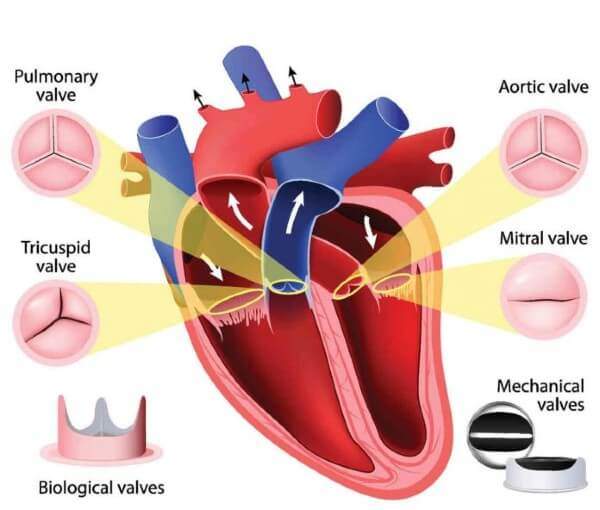
- Surgical Treatment (Valve Repair or Replacement)
If the regurgitation is severe, causing symptoms or, even if there are no symptoms, it has started to enlarge and cause dysfunction in the heart, it is time to address the mechanical problem in the valve. Surgical treatment is now the gold standard with highly successful results. Surgeries are now often performed without cutting the breastbone, with small incisions on the right side (minimally invasive surgery) or using robotic technology, which allows the patient to recover much faster.
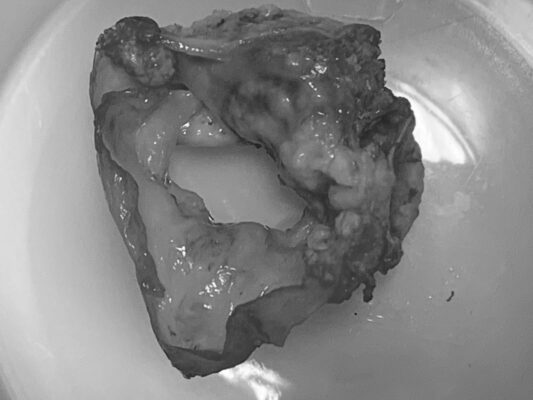
Our basic philosophy in surgery is to repair the patient’s own valve, preserving it if possible. Valve repair offers significant advantages over valve replacement, such as lower operative risk, longer life expectancy and no need to use blood thinners. However, if the structure of the valve is not suitable for repair, then the damaged valve is removed and replaced with a mechanical or bioprosthetic valve (valve replacement).
Transcatheter Methods (MitraClip)
In patients who are too high risk for open heart surgery, transcatheter treatments such as MitraClip, a non-surgical procedure performed through the groin, may be an option. In this method, the leaky leaflets of the valve are held together with a small clothespin to try to reduce leakage. This is not an alternative to surgery, but a treatment method that is only suitable for certain and risky patient groups.
What Should Be Considered After Mitral Valve Insufficiency Surgery?
A successful mitral valve surgery is the gateway to a healthy future. However, the process after passing through this door, the recovery period, is as important as the surgery itself. During this period, taking good care of the patient and following certain rules will make the success of the treatment permanent.
We can examine the things to be considered after surgery in two periods.
Early Recovery Period (First 10 days)
This is the most sensitive period when the body recovers. Today, minimally invasive mitral valve repair or replacement shortens the early recovery period considerably. There are some important rules to follow in this process:
- Regular use of medications for pain control
- Keeping the wound clean and dry
- Deep breathing exercises to prevent lung infections
- Short and regular walks recommended by your doctor
- Avoid lifting heavy objects (more than 5 kilos)
- Monitoring sudden and rapid weight gain (may be a sign of fluid accumulation in the body)
Long-term and Lifelong Habits
Once full recovery has been achieved, the goal is now to adopt a lifestyle that protects heart health.
Cardiac Rehabilitation: Participation in these professional programs accelerates the return to safe exercise.
Medication Discipline: The use of blood thinners (warfarin) is vital and requires regular blood tests (INR), especially if a mechanical valve is fitted.
Infection Prevention: Patients with artificial valves should receive prophylactic antibiotics before certain procedures such as dental treatment.
Regular Doctor Check-ups: After surgery, we will continue to follow you at regular intervals and check the condition of your valve.
Healthy Diet: A diet low in saturated fat with normal salt should be adopted.
Complete Smoking Cessation: This is an essential rule.
Can Mitral Valve Insufficiency be Prevented?
This is one of the most common questions we hear from our patients. The answer is both yes and no. Unfortunately, it is not possible to completely prevent some causes of mitral valve insufficiency, such as natural wear and tear (degeneration) due to aging or congenital structural defects. These are processes beyond our control.
But it is absolutely within our power to prevent some of the major causes of the disease, or at least to reduce its risks. The most important steps that can be taken in this regard are the following:
- Prevention of rheumatic fever
- Maintaining overall heart health
- Effective treatment of existing diseases
- Regular health checks
The most critical of these is the prevention of rheumatic fever. Streptococcal throat infections in childhood, commonly known as “beta germs”, can lead to rheumatic heart disease and mitral valve damage years later if not treated properly and completely with antibiotics. For this reason, febrile sore throats, especially in children, should be taken seriously and evaluated by a physician.
In addition, every step taken to protect general heart health indirectly reduces the risk of mitral valve insufficiency. This is because coronary artery disease and heart attack are the most common causes of secondary mitral regurgitation. A heart-friendly diet, regular physical activity, avoiding smoking, maintaining an ideal weight and keeping existing diseases such as high blood pressure under control are the most valuable investments that protect not only your mitral valve but your entire vascular system. Remember that prevention is always easier and more effective than cure.
Frequently Asked Questions
Is mitral valve insufficiency dangerous?
The severity depends on the degree of leakage. Mild failures usually do not affect quality of life and require only follow-up. Severe leaks, on the other hand, can lead to heart fatigue and eventually heart failure. These risks can be managed with regular follow-up and correct intervention.
Is mitral valve insufficiency treated with medication?
Yes, medicines play an important role in mitral valve insufficiency, reducing the workload of the heart, regulating blood pressure and slowing the effects of the disease. However, medications do not repair the valve. Surgical options come into play if necessary.
Can people with mitral valve insufficiency do sports?
Yes, an active life is encouraged. In mild to moderate insufficiency, you can do the exercises recommended by your doctor (walking, swimming, cycling). Sports that require excessive effort should be avoided. Always determine your exercise program in consultation with your cardiologist.
What should people with mitral valve insufficiency eat?
There is no special magic list; what matters is a heart-friendly diet. Cut down on salt, avoid processed and fatty foods, and eat a Mediterranean-style diet with vegetables, fruit, whole grains and olive oil. This is good for your heart and your overall health.
Which doctor treats mitral valve insufficiency?
Mitral valve insufficiency is diagnosed and monitored by a Cardiologist. If necessary, Cardiovascular Surgery is involved for surgical intervention. It is a team effort, with both branches guiding you through the process.
Does mitral valve insufficiency improve?
Spontaneous healing of the valve is difficult. Mild insufficiencies may remain stable for years. When surgical repair or replacement is performed if necessary, heart function improves and the regurgitation disappears. A healthy life is possible with the right treatment.
Does mitral valve insufficiency show up on ECG?
An ECG does not provide a direct diagnosis. However, in advanced mitral regurgitation, indirect findings such as rhythm disturbances or enlarged heart chambers may be detected. Echocardiography (ECHO) is used for definitive diagnosis and evaluation.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.