Coronary artery disease is the narrowing or blockage of the arteries that supply the heart, called coronary arteries, as a result of plaque build-up on their walls (atherosclerosis). This narrowing prevents the heart muscle from receiving enough oxygen and nutrients and is manifested by coronary artery symptoms such as chest pain (angina). The main causes include factors such as high blood pressure, cholesterol and diabetes. With modern treatments, the progression of the disease can be slowed and controlled. In particular, early diagnosis of coronary artery disease is the most critical step that directly affects treatment success and life expectancy.
| Definition | Narrowing or blockage of the coronary arteries supplying the heart, resulting in insufficient blood supply to the heart muscle |
| Causes | Atherosclerosis (arteriosclerosis), high cholesterol, hypertension, smoking, diabetes, obesity, genetic predisposition |
| Risk Factors | Advanced age, family history of heart disease, male gender, hypertension, diabetes, smoking, high cholesterol, stress, sedentary lifestyle |
| Symptoms | Chest pain (angina), shortness of breath, weakness, palpitations, sweating, nausea, sometimes silent |
| Diagnostic Methods | ECG, stress test, echocardiography, coronary angiography, CT-angiography, blood tests |
| Treatment Methods | Lifestyle changes, antiplatelet drugs, beta blockers, statins, ACE inhibitors, balloon angioplasty, stents, coronary bypass surgery |
| Complications | Heart attack (myocardial infarction), heart failure, arrhythmia, sudden cardiac arrest, sudden death |
| Prevention Methods | Smoking cessation, healthy and balanced diet, regular exercise, stress management, blood pressure and cholesterol control, regular monitoring of diabetes |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Coronary Artery Disease?
We can think of Coronary Artery Disease as the build-up of deposits over time on the inner walls of the arteries that feed the heart, blocking the flow of blood. Imagine our arteries as smooth pipes through which water flows freely. Over the years, especially substances such as excess fat, cholesterol and calcium circulating in the blood begin to stick to the inner walls of these pipes. these deposits, which we call “plaque”, gradually thicken, like a layer of limescale inside a water pipe.
As these plaques grow, they narrow the pathway through which blood passes. When the heart is at rest, it can normally manage with blood passing through this narrowed pathway. But when we climb stairs, run or have a stressful moment, our heart needs more blood and oxygen. The narrowed artery cannot keep up with this increased demand and the heart “starves”. This is usually manifested by chest pain (angina).
The most dangerous scenario is when one of these plaques suddenly cracks. The body recognizes this crack as a wound and quickly sends blood platelets to the area to repair it, forming a clot. However, when this clot forms in an already narrow vessel, it completely blocks the pathway, cutting off the blood flow abruptly. This leads to a life-threatening condition known as a “heart attack”, which requires urgent intervention.
What Causes Coronary Artery Disease?
The mechanism underlying this blockage process is called “atherosclerosis” or arteriosclerosis. It is much more than a simple mechanical blockage; it is actually a slow and insidious inflammatory process that takes years to develop in the arterial wall. It all starts with damage to the protective layer called the “endothelium” that lines the inside of the blood vessels and keeps the blood flowing smoothly.
The main factors that damage this delicate inner layer are high blood pressure, smoking, high blood sugar (diabetes) and high cholesterol. Once this damage has occurred, the body’s defense mechanisms kick in. However, this process complicates the situation. The damaged area becomes a magnet for “bad cholesterol” (LDL) circulating in the blood. Cholesterol seeps in and is swallowed by the inflammatory cells and deposited inside the vessel wall.
Over the years, this deposit grows, hardens and calcium precipitates on it, forming a “layer of lime”. These plaques gradually narrow the vessel. Although the vessel tries to compensate for this narrowing by expanding outwards for a while, at some point this mechanism becomes inadequate and blood flow is significantly reduced. This is the biological process that underlies Coronary Artery Disease.
What are the Symptoms of Coronary Artery Disease?
Coronary Artery Disease can often progress asymptomatically for years. However, when the stenosis reaches a certain level, the heart begins to signal that it is not getting enough oxygen, especially during exertion. The most common symptoms are:
- Feeling of pressure, tightness, burning or heaviness in the chest (angina)
- It feels like someone is sitting on the chest
- Pain that occurs with exertion (walking, climbing stairs) and disappears at rest
- Pain radiating to the left arm, neck, jaw or back
- Increased shortness of breath, especially during exertion
- Excessive fatigue and weakness, even with previously easy activities
- Dizziness or cold sweats
Does Coronary Artery Disease Differ in Women?
Yes, this is a very important point. The symptoms of Coronary Artery Disease in women can be different and more subtle than the classic chest pain seen in men. Unfortunately, this can lead to a delayed or missed diagnosis. Atypical symptoms, which are more common in women, include
- Sharp or stabbing pains instead of classic chest pressure
- Pain is felt in the shoulders, upper back, jaw or abdomen
- Sudden and severe fatigue that is more predominant than chest pain
- Unexplained shortness of breath
- Sleep disorders
- Indigestion or nausea
- Sudden dizziness
Is Coronary Artery Disease Fatal?
Coronary Artery Disease is more than a simple narrowing of the arteries. Left untreated or uncontrolled, it can lead to very serious life-threatening consequences. These complications clearly show why the disease should be taken seriously. Possible serious consequences include:
- Heart Attack (Myocardial Infarction): Sudden and complete blockage of the artery as a result of plaque rupture and death of the heart muscle.
- Heart Failure: A condition in which the heart, which has become tired and weakened over the years, is unable to meet the body’s need for blood.
- Arrhythmias: Dangerous and irregular heartbeats that occur as a result of disruption of the heart’s electrical system.
- Sudden Cardiac Arrest: It is when the heart suddenly stops and is unable to pump blood due to a life-threatening rhythm disturbance.
What are the Risk Factors for Coronary Artery Disease?
Some risk factors are related to our genetic inheritance or the natural course of life and we cannot change them. Being aware of these factors allows us to be more mindful of other factors that we can change:
- Advanced age
- Male gender (risk is equalized in women after menopause)
- Family history of early heart disease
What are the risk factors for Coronary Artery Disease that we can change?
The good news is that many of the most important factors that predispose to Coronary Artery Disease are directly related to our lifestyle choices and are under our control. Managing these factors is key to preventing the disease or slowing its progression:
- High LDL (“bad”) cholesterol
- High blood pressure (Hypertension)
- Smoking and use of tobacco products
- Diabetes (Diabetes)
- Overweight and obesity (especially abdominal fat)
- Physical inactivity
- Unhealthy eating habits
- Intense and unmanageable stress
What lifestyle changes are recommended to reduce the risk of Coronary Artery Disease?
Prevention and treatment of coronary artery disease should be considered as a whole. As important as medications and interventional treatments are, lifestyle changes are always the foundation. These steps are a powerful shield that protects not only your heart but your whole body. The most important steps that can be taken in this regard are the following:
- Be Active: Aim for at least 30 minutes of brisk walking most days of the week. Even small changes like taking the stairs instead of the elevator and not driving short distances can make a big difference.
- Eliminate Smoking from Your Life: Quitting smoking is the best thing you can do for your heart health. From the moment you quit, your risk starts to decrease. It is equally important to avoid secondhand smoke.
- Keep Your Weight Under Control: Being at a healthy weight reduces the burden on your heart and positively affects all other risk factors such as blood pressure, cholesterol, sugar, etc.
- Learn to Deal with Stress: While it is not possible to completely eliminate the stress of life, you can learn to manage it. Yoga, meditation, spending time with loved ones or engaging in a hobby you enjoy are effective ways to reduce stress.
How does a heart-healthy diet affect the risk of Coronary Artery Disease?
Nutrition is one of our most powerful weapons in the fight against Coronary Artery Disease. The foods we consume directly affect the health of our arteries. The goal is to adopt an overall healthy eating pattern rather than counting individual foods. The model known as the Mediterranean diet is the best guide.
A must-have on your table:
- Olive Oil
- Plenty of greens and vegetables
- Fruits
- Legumes (chickpeas, lentils, beans)
- Whole grains (bulgur, whole wheat bread)
- Nuts such as walnuts, hazelnuts, almonds
- Fish (especially salmon, sardines) at least twice a week
Those to be avoided or severely limited:
- Processed meat products (salami, sausage, pepperoni)
- Sugary drinks and instant fruit juices
- Refined carbohydrates such as white bread, pastries, rice
- Packaged snacks, crisps, biscuits
- Saturated fats such as butter, tail fat
- French fries and margarines containing trans fats
- Excessive salt consumption
What does ‘secondary prevention’ mean for people diagnosed with coronary artery disease?
When a person is diagnosed with Coronary Artery Disease (e.g. after a heart attack, stenting or bypass surgery), the approach to treatment changes fundamentally. The aim is no longer just to reduce risks, but to prevent future events (a new heart attack, stroke, etc.) by controlling an active and progressive disease. We call this “secondary prevention”.
This requires a much more determined and aggressive approach than primary prevention. While lifestyle changes remain vital, they are no longer sufficient on their own. Medication becomes mandatory. Cholesterol and blood pressure targets are much lower. For example, the goal is usually to reduce bad cholesterol (LDL) levels below 70 mg/dL. Regular use of anticoagulants is an essential part of treatment. It is important to remember that procedures such as stents or bypasses do not “cure” the disease, but only open or bridge a blocked vessel. Lifelong adherence to secondary prevention strategies is essential to prevent progression of the disease in other vessels.
How is Coronary Artery Disease Diagnosed?
When a patient’s complaints and risk factors raise suspicion of coronary artery disease, the diagnostic process usually starts with basic tests that do not require any intervention in the body. These tests give important clues about the presence of the disease:
- Blood tests
- Electrocardiogram (ECG)
- Echocardiography (ECHO – Heart ultrasound)
- Effort (Stress) test
How is Coronary CT Angiography used in the diagnosis of Coronary Artery Disease?
Coronary CT Angiography is a modern technology that we use to image blood vessels in a non-invasive way, especially in patients with symptoms but at low or intermediate risk. This test does not involve a catheter in the groin or arm, as with traditional angiography. An iodized contrast agent (dye) is injected through a vein in your arm, while a quick computed tomography (CT) scan is performed. This takes just a few seconds and produces a detailed three-dimensional map of the coronary arteries. This map clearly shows calcium deposits, plaques and stenoses in the vessels.
Why is angiography called the ‘gold standard’ in the diagnosis of coronary artery disease?
When other tests are suspicious or the patient’s condition is high-risk, the “gold standard” method, classical coronary angiography, is used to confirm the diagnosis and determine the treatment plan. This procedure is performed in a catheterization laboratory. A very thin and flexible tube called a “catheter” is inserted into the heart through an artery in the groin or wrist. Contrast material is injected into the coronary arteries at the tip of the catheter and X-rays are taken. These films show the blood flow in the arteries, the exact location, number and severity of the stenoses (what percentage are blocked). The great advantage of angiography is that it is not only a diagnostic method, but also opens the door to treatment. If a critical stenosis is detected during the procedure, the vessel can be opened instantly by stenting in the same session.
Can Coronary Artery Disease be cured with medication?
The medical treatment of CAD requires a drug regimen that targets the different mechanisms of the disease and works in harmony with each other. These medicines control symptoms, slow the progression of the disease and, most importantly, prevent events such as heart attacks:
- Cholesterol-lowering drugs (especially statins)
- Anticoagulants (Antiplatelets – Aspirin, clopidogrel, etc.)
- Drugs that control heart rate and blood pressure (beta blockers)
- Vasodilators and drugs to relieve chest pain (Nitrates, Calcium channel blockers)
What is the vital role of anticoagulant therapy in Coronary Artery Disease?
When an atherosclerotic plaque cracks, the body quickly forms a blood clot at this site. This clot completely blocks blood flow in a narrowed coronary artery, causing a heart attack. Anticoagulants (antiplatelet drugs) prevent this deadly clot from forming by reducing the stickiness of blood platelets (platelets) to each other. For this reason, it is vital that patients diagnosed with CAD or who have had a stent implanted take these medications as prescribed by their physicians and for as long as recommended.
How does Coronary Angioplasty and Stenting treat Coronary Artery Disease?
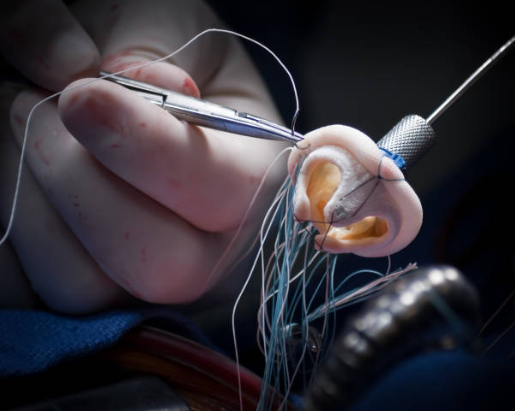
Coronary Angioplasty and Stenting is a minimally invasive procedure used to open a blocked or severely narrowed coronary artery without surgery. During the angiography procedure, the site of the stenosis is accessed with a catheter with a deflated balloon at the tip. The balloon is inflated inside the stenosis, crushing the plaque against the vessel wall and widening the bloodway. Then, to prevent the vessel from narrowing or collapsing again, a tubular metal cage made of wire mesh, often called a “stent”, is placed in the same area. Like a scaffold, the stent supports the vessel from the inside, keeping it open. The drug-coated stents used today also minimize the risk of re-narrowing of the vessel with special drugs secreted from their surface.
When is Coronary Artery Bypass Surgery (CABG) necessary for Coronary Artery Disease?
Coronary Artery Bypass Surgery is a surgical treatment for more complex and widespread disease where stenting is inappropriate or inadequate. The basic logic of this surgery is to create a new pathway, a “bridge” or “bypass” that carries the blood forward by going around the blockage instead of opening the blocked vessel. For this bridge, an intrathoracic artery from the patient’s own body, an artery from the arm or a vein from the leg is usually used. Bypass surgery may be a superior treatment option, especially in the following cases
- Severe stenosis in multiple coronary vessels
- Critical stenosis in the left main coronary artery, the main artery of the heart
- Presence of diffuse and multiple vascular disease, especially in patients with diabetes
- The structure of the stenosis is not technically suitable for stenting
- Decreased strength of heart contraction
What is the process of traditional coronary artery bypass surgery?
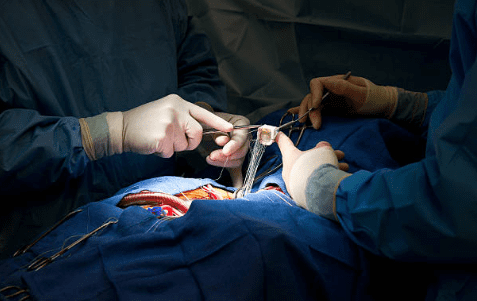
Traditional bypass is an open heart surgery that has been performed safely and with proven results for many years. Under general anesthesia, the sternum is cut to access the heart. During the operation, the heart is stopped with a special solution so that the surgeon can work safely in a bloodless and immobilized environment. Meanwhile, the patient’s blood circulation is maintained by a heart-lung machine that temporarily takes over the function of the heart and lungs. Meanwhile, the surgeon uses vascular grafts prepared from the patient’s own body to sew new blood pathways ahead of the blocked vessels. After the bypasses are completed, the heart is restarted and the operation is terminated.
What advantages does minimally invasive and robotic surgery offer in Coronary Artery Bypass Surgery?
With the advancement of technology, we no longer always have to perform bypass surgery by completely opening the sternum. Minimally invasive and robotic surgery are modern approaches that significantly reduce the trauma of this major surgery in appropriate patients. Instead of cutting through the breastbone, these techniques access the heart through small incisions between the ribs. The main advantages of this approach are:
- Smaller scar
- Less pain after surgery
- Reduced risk of bleeding
- Shorter hospital stay
- Faster return to everyday life and work
- Lower risk of infection due to not cutting the sternum
Robotic surgery is the cutting edge of this technique. With robotic arms operated from a console, the surgeon can perfectly suture even the most complex sutures with precision that the human hand cannot achieve.
| Feature | Coronary Angioplasty and Stenting (PCI) | Coronary Artery Bypass Surgery (CABG) |
| Procedure Type | Minimally Invasive (Interventional) | Open Heart Surgery or Minimally Invasive |
| Main Indications | Fewer, simpler strictures | Multiple, complex strictures, diabetes |
| Anesthesia | Usually local | General |
| Recovery Time | Fast (1-7 days) | Longer (6-12 weeks) |
| Basic Principle | Opening the existing stenosis from the inside | Creating a new path around the blockage |
How does the recovery process progress after treatment for Coronary Artery Disease?
Recovery after treatment varies greatly depending on the procedure performed. After stenting, patients usually stay in the hospital overnight and can return to their normal lives within a few days. Bypass surgery, on the other hand, is a larger surgery and the recovery process is more gradual. The average hospital stay is 5-7 days and full physical recovery can take 2-3 months. Strict adherence to medication and lifestyle changes is critical for lasting success after both procedures.
Does Coronary Artery Disease Increase Life Expectancy?
After a cardiac event or surgery, it is crucial that patients recover not only physically but also mentally and return to life with confidence. Cardiac rehabilitation is a comprehensive, physician-supervised program that serves this very purpose. This program is an integral part of the treatment and provides many benefits to the patient. The main components of this program are:
- Personalized exercise training
- Heart-friendly nutrition counseling
- Training on medication use and disease management
- Stress management techniques
- Psychological support
It has been proven that patients who participate in cardiac rehabilitation programs have an improved quality of life, a significantly lower risk of future heart problems and feel much more confident. This is one of the most important steps towards a healthy future.
Frequently Asked Questions
How to recognize coronary artery disease?
The most typical symptom is a feeling of pressure in the chest when walking or climbing hills, which goes away at rest. The pain can also radiate to the jaw, left arm or back. Shortness of breath and fatigue are also important signs. For a definitive diagnosis, a stress test, echocardiography and coronary angiography, which is the gold standard, are performed.
How long does a person with coronary artery disease live?
There is no clear answer, because life expectancy depends on your lifestyle, adherence to treatment and risk factors. With modern treatments and the right habits, a long, quality life is possible. You are in control!
Can coronary artery be detected on ECG?
Not always. A resting ECG is often normal. An exertional ECG measures the heart’s response to fatigue. Further tests may be needed for a definitive diagnosis.
What should coronary artery disease patients not eat?
Avoid packaged and processed foods, foods containing trans fats, excess salt, saturated fats, sugary drinks and baked goods. You need to remove “factory products” from your table and replace them with “farm” natural foods.
Where do the coronary arteries supply?
The coronary arteries supply the heart muscle itself. When these vessels, which work like the crown veins of the heart, are blocked, the heart muscle can be damaged and cannot function properly.
Does a coronary artery show up in a blood test?
A blood test does not directly show vascular stenosis, but it can reveal risks such as cholesterol, triglycerides and sugar. During a heart attack, heart damage can be detected with certain enzymes such as troponin.
Who has coronary artery disease?
Smokers, high blood pressure, diabetes, high cholesterol, those with a family history of heart disease at an early age, overweight and sedentary individuals are at risk. It is more common in men, but its incidence increases in women after menopause.
At what age does coronary artery disease occur?
It usually becomes symptomatic after the 40s; the risk increases after 45 in men and 55 in women. However, it can also be seen at a young age if there are risks such as genetic predisposition, smoking and diabetes.
How many hours does coronary artery surgery take?
Coronary bypass surgery usually takes between 3-6 hours. Factors such as single vessel or multiple vessel replacement and additional surgical procedures affect the duration. The most important goal is to complete the surgery safely and successfully.
Which doctor to see for coronary artery disease?
The cardiologist is the first point of contact for diagnosis and treatment. In cases requiring advanced surgery or stents, a Cardiovascular Surgery specialist steps in. The two branches work together in this process.
Is coronary artery disease genetic?
Yes, the risk is increased if there is a family history of premature heart disease (especially in male relatives under 55 and female relatives under 65). But managing risk factors is key to staying healthy despite genetics.
Does coronary artery disease happen in young people?
Yes, coronary artery disease can develop even in the 30s, especially if there is obesity, irregular diet, smoking and familial high cholesterol. If there is a complaint in young people, cardiology should be consulted.
Is coronary artery disease permanent?
Yes, coronary artery disease is chronic. However, with the right treatment and a healthy lifestyle, a lifelong quality and long life is possible. Follow-up and compliance with treatment is very important.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Heart diseases are conditions that impair the structure and function of the heart, leading to [...]
Aug
How the Heart Works
The heart functions as a muscular pump that circulates blood throughout the body. It consists [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Heart valve surgery duration varies depending on the complexity of the case and the valve [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Coronary bypass surgery duration depends on the number of blocked arteries and patient-specific factors. On [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Kalp kapakçığı değişimi, kapakların ileri derecede daralması (stenoz) veya yetersiz kapanması (yetmezlik) durumlarında, onarımın mümkün [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Kalp kapakçığı tamiri, mevcut kapağın korunarak yapısal bozukluklarının düzeltilmesi işlemidir. Kapak yaprakçıkları, kordonları veya halka [...]
Aug
Life After Heart Valve Surgery
Life after heart valve surgery involves a structured recovery period, with gradual improvement in physical [...]
Aug
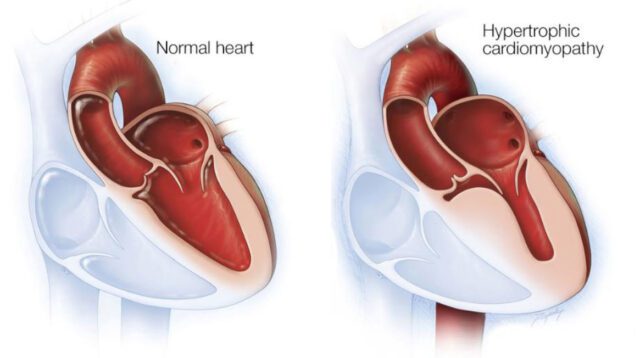
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, [...]
Aug