Arteriosclerosis, medically known as atherosclerosis, is the narrowing or complete blockage of an artery by the build-up of plaques containing cholesterol and fat on the inner wall of the arteries. The symptoms of atherosclerosis differ depending on which part of the body the blockage is in. In the heart, the most common symptoms are chest pain and shortness of breath. In leg veins, calf pain (claudication) during walking is typical. When it affects the vessels of the brain, it causes stroke symptoms such as sudden speech impairment, facial drooping or unilateral arm and leg weakness. These signs should be taken seriously.
| Definition | Blockage of blood vessels, usually due to atherosclerosis, clots or another cause |
| Causes | Atherosclerosis (arteriosclerosis), blood clots, embolism, vascular inflammation, trauma, diabetes, high cholesterol, smoking, hypertension |
| Risk Factors | Age, family history of vascular disease, smoking, high blood pressure, high cholesterol, diabetes, obesity, sedentary lifestyle |
| Symptoms | Depending on the location of the blockage; pain, numbness, weakness, coldness, bruising, sudden loss of organ function (e.g. stroke, heart attack, sudden pain in the leg) |
| Diagnostic Methods | Angiography, Doppler ultrasonography, CT-angiography, MR-angiography, blood tests |
| Treatment Methods | Surgical intervention (bypass) due to diffuse stenosis, lifestyle changes |
| Complications | Organ damage, tissue death (gangrene), stroke, heart attack, heart attack, stroke, loss of limb |
| Prevention Methods | Smoking cessation, healthy eating, regular exercise, blood pressure and cholesterol control, diabetes management, weight control |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Vascular Occlusion?
To better understand this topic, it is necessary to distinguish between two terms: arteriosclerosis and atherosclerosis. Arteriosclerosis is a general term meaning “hardening of the arteries”. You can think of it like an old garden hose that has been used for years and years, but over time it loses its flexibility and becomes hard and brittle. This includes many conditions in which the blood vessels harden as part of the natural aging process.
However, what we should focus on and what we mean when we say “atherosclerosis” is atherosclerosis. This is the most common and most dangerous type of arteriosclerosis. Going back to the garden hose example, atherosclerosis is not only the hardening of the hose, but also the formation of deposits on its inner wall, such as algae, lime and mud, which block the water passage. We call these “clogging” deposits plaques. These plaques are a mixture of cholesterol, fat, calcium and cellular waste. As plaque builds up, it narrows the space for blood to flow through and deprives our organs of oxygen. This distinction is very important, because while “erection” sounds like a helpless condition, “plaque accumulation” gives us concrete goals (such as lowering cholesterol, eating right) that can slow or even stop this process.
What Causes Vascular Occlusion?
Atherosclerosis, or atherosclerosis, is not something that happens overnight. It is a slow and complex process that is genetically inherited and starts in childhood or adolescence and progresses silently over decades. We can think of it as a kind of plaque ring that starts on the arterial wall, and later in life, cholesterol stones settle in these plaques. It all starts with damage to the delicate single layer of cells lining the inside of the arteries, which we call the endothelium.
The main triggers for this damage include the constant mechanical pressure on the vessel wall from high blood pressure, the toxic chemicals in cigarette smoke or the chemical irritation caused by high levels of bad cholesterol and sugar in the blood.
Our body sends an “emergency” team to repair the damaged area. White blood cells (white blood cells), which are part of this team, stick to the damaged area and infiltrate the vessel wall. There, they begin to soak up the abundant bad cholesterol (LDL) in the blood like a sponge. These cholesterol-filled cells are called “foam cells” because they look like foam under a microscope. As these foam cells build up, “fatty streaks” form on the vessel wall, the first visible sign of the disease.
Over the years, more and more cholesterol, calcium and cellular debris accumulate in this area. To control this build-up, the body tries to cover it with a hard shell (fibrous capsule), resulting in the formation of what we call “plaque”. The structure of this plaque determines the future fate of the patient. There are two types of records:
- Stable Record
- Unstable (Sensitive) Plaque
Stable plaques are harder, usually slow-growing plaques with a thick crust. They can slowly narrow the blood vessel, leading to chronic symptoms such as chest pain during exertion. The most dangerous are the unstable, or fragile, plaques. These have a thin crust and a fat-rich and highly inflamed interior. This thin crust can rupture suddenly, like a pimple. When the crust ruptures, the coagulation-inducing substances inside the plaque come into contact with the blood and a blood clot (thrombus) rapidly forms in the area. This clot can completely block the blood vessel within minutes, creating the final and most deadly step that leads to a heart attack or stroke.
Risk Factors for Vascular Occlusion: In Men and Women
There are a number of risk factors that accelerate and fuel the development of atherosclerosis. Dividing these into factors that we cannot change and those that we can change through intervention makes it easier to understand the situation.
Non-modifiable Risk Factors:
Unfortunately, some risk factors are beyond our control:
- Advancing age
- Family history (early onset of heart disease in first-degree relatives)
- Male gender (risk is equalized in women after menopause)
Having these factors does not mean that you will develop atherosclerosis, but it does mean that you need to be more careful and keep other risk factors under closer control.
Risk Factors that can be changed and that we need to focus on:
The good news is that many of the most important factors leading to atherosclerosis are directly related to our lifestyle habits and can be controlled:
- High LDL (bad) cholesterol
- Low HDL (good) cholesterol
- High blood pressure (Hypertension)
- Tobacco use (cigarettes, hookah, electronic cigarettes)
- Diabetes (Diabetes)
- Overweight and especially abdominal fat (obesity)
- Sedentary lifestyle
- Unhealthy eating habits
- Intense and unmanageable stress
“High LDL (bad) cholesterol” is the main building block of plaques; it is like bricks in a wall. “High blood pressure”, on the other hand, is like a worker who damages that wall by constantly hitting it with a hammer, making it easier for new bricks (cholesterol) to adhere. “Tobacco use” is the biggest saboteur that accelerates this process at every stage. It directly damages the lining of the blood vessels, increases the tendency of the blood to clot and disrupts the cholesterol balance. Diabetes also significantly accelerates the process by weakening the vessel walls and increasing inflammation. These risk factors often coexist and multiply each other’s negative effects. Treatment therefore requires a holistic approach targeting all of these factors.
| Region and Affected Vessels | Consequences and Symptoms |
| Heart – Coronary Arteries | Chest pain (angina), heart attack, shortness of breath |
| Brain – Cerebral Arteries | Stroke (paralysis), dizziness, slurred speech, loss of consciousness |
| Legs – Peripheral Arteries | Leg pain, cramps, coldness, delayed wound healing, gangrene |
| Kidney – Renal Arteries | Hypertension, renal failure, changes in urine |
| Neck – Carotid Arteries | Transient ischemic attack (TIA), stroke risk, visual impairment, dizziness |
| Abdomen (Intestines) – Mesenteric Arteries | Severe abdominal pain, nausea, intestinal ischemia |
| Male Genitalia – Penile Arteries | Erectile dysfunction, sexual dysfunction |
| Right and Left Arm – Brachial, Radial and Ulnar Arteries | Pain in the arms, numbness, loss of strength, coldness, pallor, weak pulse |
What are the Symptoms of Vascular Blockage in the Heart?
When a blockage affects the vessels that supply the heart, called “coronary arteries”, we call it coronary artery disease. Symptoms that occur when the heart muscle does not get enough blood and oxygen are the most common manifestation of the disease. Symptoms of cardiovascular blockage usually start insidiously and manifest themselves with exertion.
The most typical symptom in the chronic (long-term) stage of the disease is “angina pectoris”, or chest pain. This pain is usually felt in the following ways:
- A feeling of pressure, squeezing, burning or heaviness in the center or left side of the chest
- Intense pressure, described as if an elephant had sat on the chest
- Pain or discomfort that may radiate to the left arm, shoulder, neck, jaw or back
- Shortness of breath that occurs with exertion (walking, climbing stairs, running) and passes with rest
- Unexplained fatigue and weakness far above normal
These classic symptoms may not be the same for everyone. Especially in women, the elderly and diabetics, the symptoms of cardiovascular blockage may be more subtle. In these groups, indigestion, nausea, sudden sweating, atypical pain in the back or jaw may take precedence over chest pain. Therefore, such complaints should never be dismissed as “gas pains” or “muscle pain”.
The acute, sudden and most feared aspect of the disease is a heart attack. This occurs when a plaque ruptures and suddenly blocks a blood vessel, and is a life-threatening condition that requires immediate medical attention. Heart attack symptoms are usually more severe and do not go away with rest:
- Overwhelming and severe pain that starts in the chest, usually lasting more than 20 minutes
- Intense cold sweating
- Nausea and sometimes vomiting
- Dizziness, feeling dizzy
- Intense anxiety and fear of death
What Symptoms Does Vascular Blockage in the Brain and Cervical Vessels Cause?
After the heart, the brain is the second most critical organ most frequently affected by vascular occlusion. A stroke occurs when the carotid arteries, the main vessels supplying the brain, or smaller vessels within the brain are blocked. A stroke is a permanent damage to part of the brain tissue as a result of a lack of blood supply.
Sometimes the body sends a “warning” before a major stroke arrives. We call this a “Transient Ischemic Attack” (TIA) or “mini-stroke”. In a TIA, the blockage in the blood vessel is temporary and the symptoms usually resolve completely within a few minutes or hours. However, this is a sign of impending disaster. A person who has a TIA has a very high risk of having a permanent stroke within the first few days. TIA is therefore an emergency, just like a heart attack, and requires immediate medical evaluation.
The symptoms of stroke and TIA start suddenly and are quite typical. To easily keep these symptoms in mind, we can adapt the international acronym “F.A.S.T.” (Face, Arms, Speech, Time) into Turkish. Remember that symptoms usually affect only one half of the body.
- Face shift When you ask a person to smile, one side of their face shifts downwards.
- Weakness in the arms: When you ask the person to raise both arms forward, one arm falls down or does not raise at all.
- Speech impairment: The person has difficulty repeating a simple sentence, slurs words or speaks gibberish.
- Don’t waste time: If you notice any of these symptoms, you should immediately call for emergency help.
Other possible stroke symptoms include
- Sudden numbness or loss of sensation in one half of the body (face, arm, leg)
- Sudden confusion or difficulty understanding
- Sudden loss of vision in one or both eyes, blurred vision or double vision
- Sudden dizziness with difficulty walking, loss of balance and coordination
- Unprecedented, sudden and severe headache
What are the Symptoms of Vascular Occlusion in the Legs and Feet?
Blocked arteries affect not only the heart and brain, but also the arteries that supply the legs. We call this condition “peripheral arterial disease” (PAD). Symptoms of vascular occlusion in the leg usually occur in exertional situations, such as walking, and the presence of the disease is an important sign that the vessels of the heart and brain are also at risk.
The most classic symptom of PAH is a condition called “intermittent claudication”. This is a cramping, compressive pain in the leg muscles (usually in the calf, but also in the thigh or buttock) after walking a certain distance. This pain is caused by the increased oxygen demand of the exercising muscles not being met by the constricted blood vessels. It forces the person to stop and rest and goes away in a few minutes with rest. When you start walking, it reappears at the same distance.
As the disease progresses, other symptoms begin to appear as blood flow is further reduced. Symptoms of foot and leg vascular occlusion include the following:
- A marked feeling of coldness in the legs and feet, especially compared to the other leg
- A shiny, taut appearance and discoloration of the skin of the legs (pale or purplish color)
- Loss of hair on legs and feet
- Slow growth, thickening and dull toenails
- Wounds (ulcers) on the legs or feet, especially between the fingers and on the heel, which heal easily and too late
- Severe foot pain, even at rest, especially at night when lying down and relieved by lowering the leg off the bed (this is a sign of an emergency condition called “critical leg ischemia”)
- Weak or absent pulses on the back of the foot or on the inside of the ankle
How to Detect Cardiovascular Blockage without Angiography?
The answer to the question “How can I detect cardiovascular blockage without angiography?” is yes. Angiography is a method we use especially in cases where treatment is planned, but there are many simpler and non-invasive methods we use in the diagnostic process. The diagnostic process starts with a good doctor-patient interview. After listening to your complaints, lifestyle and family history, a physical examination provides the first clues. We then use some tests to confirm or exclude our suspicions.
The main diagnostic methods we use to understand the presence and severity of vascular occlusion are the following:
- Blood Tests: Values such as cholesterol (LDL, HDL) and triglyceride levels, blood sugar and hs-CRP, a marker of inflammation, reveal your overall risk profile.
- Electrocardiogram (ECG): Records the electrical activity of the heart and can show rhythm disturbances or signs of a past heart attack.
- Stress Test: By monitoring your ECG and blood pressure while you walk on a treadmill, we observe how your heart reacts under load. ECG changes or chest pain with exertion may indicate a problem with the coronary vessels.
- Doppler Ultrasonography: This painless and radiation-free method uses sound waves to visualize the blood flow in the vessels supplying the neck, legs or intra-abdominal organs and can detect stenosis or blockages.
- Ankle-Arm Index (ABI): A very simple test used when peripheral artery disease is suspected. It is based on the ratio of blood pressure readings measured at the ankle and arm.
- Computed Tomography (CT) Angiography: This test, performed with intravenous contrast medium, produces a detailed three-dimensional map of the arteries and clearly shows the location and degree of stenosis.
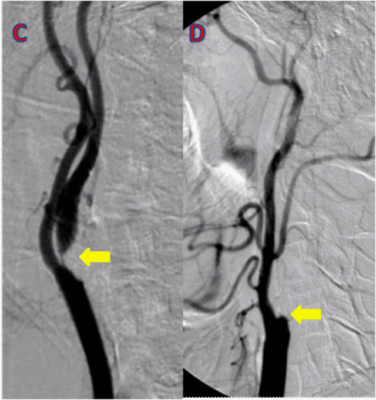
If these tests reveal a critical stenosis that may require treatment, or if the diagnosis is still unclear, the “gold standard” procedure is catheter angiography. In this procedure, a thin tube (catheter) is inserted through an artery, usually in the wrist or groin, into the arteries supplying the heart or other organs. A special dye is then administered through the catheter to take X-rays of the blood vessels and clearly visualize the blockages. The main advantage of angiography is that it allows treatment (balloon/stent) at the same time as diagnosis.
How to Open a Blocked Artery? How is it treated?
Vascular occlusion is a chronic disease and treatment is lifelong. The aim of treatment is to slow the progression of the disease, control symptoms and prevent serious events such as heart attack and stroke. To this end, we use a combination of three main treatment approaches.
Lifestyle Changes: Indispensable for Treatment
This is the main pillar of treatment. No medication or surgery can replace a healthy lifestyle.
Heart-Friendly Nutrition: Nutrition models such as the Mediterranean diet should be taken as a basis. What you should not miss from your table:
- Plenty of fresh and colorful vegetables
- Fruits
- Whole grain products (whole wheat bread, bulgur, oats)
- Legumes (chickpeas, lentils, beans)
- Fish (especially fatty fish such as salmon and sardines)
- Raw nuts such as walnuts, hazelnuts, almonds
- Olive Oil
Here’s what you should avoid or severely limit:
- Processed meat products (salami, sausage, pepperoni)
- Sugary and carbonated drinks
- Pastries, pastries, cakes made with white flour
- Fried foods and packaged products containing trans fats
- Excess salt and sugar
Regular Physical Activity: Even brisk walking for 30-45 minutes at least 5 days a week makes a big difference. Swimming and cycling are also great options.
Quitting Smoking Completely: If you smoke, the best thing you can do is to quit immediately.
Maintaining Ideal Weight: Getting rid of excess weight has miraculous effects on blood pressure, cholesterol and blood sugar.
Medication Therapy
In addition to lifestyle changes, we often need medication to control risk factors.
- Statins: The most important group of drugs that lower bad cholesterol (LDL) levels and stabilize plaque.
- Blood Thinners (Antiplatelets): Drugs such as aspirin and clopidogrel reduce the risk of heart attack and stroke by preventing clot formation.
- Blood Pressure Medicines (Antihypertensives): Used to keep blood pressure at target levels.
- Diabetes Medicines: Blood sugar control is vital for vascular health.
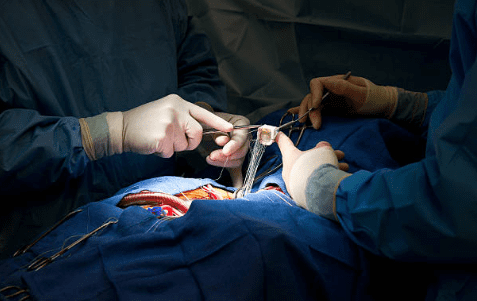
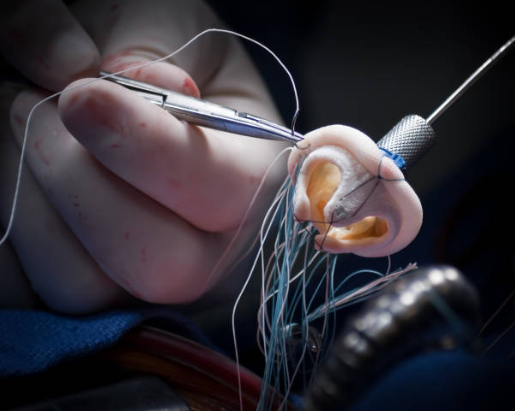
Interventional and Surgical Treatments
If symptoms persist despite medication and lifestyle changes, or if the stenosis is critical, interventions may be needed to restore blood flow.
- Balloon Angioplasty and Stenting: It is the process of opening the blocked vessel with the help of a catheter with a small balloon at the end and placing a small metal cage called a “stent” to prevent re-narrowing. It can usually be applied for a very short and single segmental stenosis in the vessel.
- Bypass Surgery: When there are severe stenoses, especially in multiple blood vessels, a piece of blood vessel from another part of the body (usually the chest or leg) is used to create a new “bridge” to carry blood further away from the blockage.
- Endarterectomy: Especially in accessible vessels such as the carotid artery (carotid artery), it is the process of surgically opening the vessel and scraping out the plaque inside.
Which of these methods is suitable for you is decided by taking into account many factors, such as the condition of your disease, the location and number of stenoses seen on angiography.
How Does Vascular Occlusion Go Away? Can It Be Prevented or Reversed?
This is the question that our patients are most curious about and seek hope for. The answer to this question is both yes and no. It is not possible to completely “erase” a hardened, calcified plaque with the current technology. However, this does not mean that we are helpless. The main goal of modern treatments and lifestyle changes is to stop the plaque from growing, stabilize it (i.e. reduce the risk of rupture) and extinguish the inflammation inside the vessel.
Scientific studies have shown that, especially with high-dose statin therapy and a very strict lifestyle change, the fatty and inflamed part of the plaque can be reduced, i.e. the plaque can “shrink” somewhat. This significantly reduces the risk of clots blocking the arteries and therefore the risk of heart attack or stroke. So yes, it is certainly possible to stop the progression of the disease and “reverse” its dangerous consequences.
Your most powerful weapon in the fight against atherosclerosis is knowledge and determination. Knowing your risk factors, undergoing regular medical check-ups and adopting healthy living habits as a way of life will make you victorious in your fight against this insidious enemy. Remember, the healthier your veins are, the healthier you are.
What is Good for Blocked Arteries?
The methods that are good for vascular occlusion are as follows:
Healthy Nutrition
- Consume fish rich in omega-3 (salmon, sardines, mackerel)
- Consume foods containing healthy fats such as walnuts, almonds and avocados
- Eating oats, whole grains and fibrous vegetables
Increasing Antioxidant Consumption
- Antioxidant-rich fruits such as pomegranate, blueberries, strawberries, grapes
- Green tea consumption
- Consuming dark green leafy vegetables such as broccoli and spinach
Garlic Usage
- Regular garlic consumption provides vasodilation and regulates blood flow.
Exercise
- Doing cardio activities such as regular walking, swimming and cycling
- At least 150 minutes of moderate-paced exercise per week
Breaking Harmful Habits
- Quitting smoking
- Reducing or quitting alcohol consumption
Achieving Weight Control
- Getting rid of excess weight and reaching the ideal weight
Stress Management
- Yoga, meditation, breathing exercises
- Engaging in stress-reducing activities (nature walks, hobbies)
Adequate Water Consumption
- Drinking at least 2 liters of water daily, supporting blood circulation
Regular Health Checks
- Regular monitoring of cholesterol and blood pressure values
- Regular doctor check-ups
These methods are very useful in maintaining vascular health and preventing and alleviating vascular occlusion.
Frequently Asked Questions
How does a blocked artery go away?
The treatment of vascular occlusion is planned with an individualized road map. Depending on the location and degree of blockage, lifestyle changes (healthy diet, exercise, quitting smoking), medications, balloon/stent applications or bypass surgery may be required. Our goal is to restore safe and healthy blood flow.
How do we know if the arteries are blocked?
Your body signals; symptoms such as chest pain or shortness of breath in the heart vessels, cramps in the calf when walking and pain that passes when resting in the leg vessels, sudden loss of vision or speech impairment in the carotid artery. If you have these symptoms, you should consult a doctor.
Can a blood test show atherosclerosis?
Blood tests do not directly show a blocked artery, but they do reveal your risk for blocked arteries. The risk increases if bad cholesterol (LDL), sugar and inflammation markers are high. If obstruction is suspected, imaging methods such as ultrasound and angiography are used.
Can ECG detect vascular occlusion?
The ECG shows the heart muscle that is fed by the blood vessel, not the blood vessel itself. If there is a critical blockage or if you have had a heart attack, the ECG may show signs. However, a normal ECG does not guarantee that there is no blockage. If necessary, further tests such as a stress ECG are performed.
Does stress cause atherosclerosis?
Stress alone does not clog blood vessels, but it can significantly accelerate this process. Stress hormones increase inflammation in the vascular wall, raise blood pressure and can lead to unhealthy habits. Stress management is as important for vascular health as healthy diet and exercise.
Which department should I go to for vascular occlusion?
You should consult Cardiology for symptoms related to the heart and Cardiovascular Surgery in areas such as the leg/arm/trunk veins. If necessary, the two departments work together to plan the most appropriate treatment.
What are the symptoms of vascular occlusion in the arms?
Complaints such as pain, cramps and fatigue in the arm during use, pain that goes away at rest, coldness, pallor, weak pulse, numbness in the fingers may be a sign of blockage. In this case, you need to contact a specialist.
Does a blocked artery get better on its own?
Unfortunately, blocked blood vessels do not open by themselves. The body has no mechanism to completely dissolve plaques. Only with treatment can the plaques be stabilized, progression halted and a safe life ensured.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Heart diseases are conditions that impair the structure and function of the heart, leading to [...]
Aug
How the Heart Works
The heart functions as a muscular pump that circulates blood throughout the body. It consists [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Heart valve surgery duration varies depending on the complexity of the case and the valve [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Coronary bypass surgery duration depends on the number of blocked arteries and patient-specific factors. On [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Kalp kapakçığı değişimi, kapakların ileri derecede daralması (stenoz) veya yetersiz kapanması (yetmezlik) durumlarında, onarımın mümkün [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Kalp kapakçığı tamiri, mevcut kapağın korunarak yapısal bozukluklarının düzeltilmesi işlemidir. Kapak yaprakçıkları, kordonları veya halka [...]
Aug
Life After Heart Valve Surgery
Life after heart valve surgery involves a structured recovery period, with gradual improvement in physical [...]
Aug
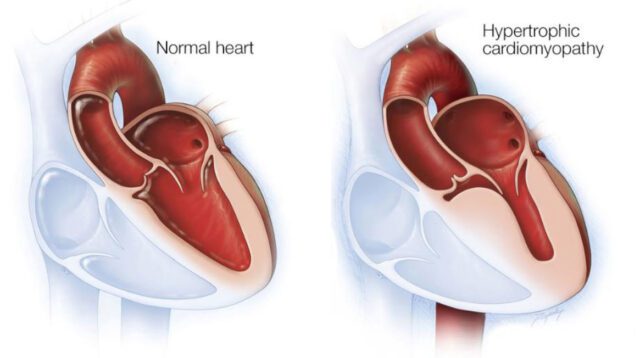
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, [...]
Aug