An aortic aneurysm is a dangerous weakening of the wall of the aorta, the body’s main artery. Although it often progresses asymptomatically, deep pain in the abdomen or back and the sensation of a pulsating mass are among the most common complaints. Aortic aneurysm treatment depends on the severity of the condition. While small and slow-growing aneurysms can be kept under control with medication and active monitoring, aortic aneurysm surgery performed with open or closed (endovascular) methods for aneurysms that reach a certain size or grow rapidly is a life-saving intervention that eliminates the risk of rupture.
| Types | Abdominal Aortic Aneurysm (AAA), Thoracic Aortic Aneurysm (TAA), Thoracoabdominal Aortic Aneurysm |
| Causes | Atherosclerosis, genetic connective tissue diseases (Marfan, Ehlers-Danlos), trauma, infection, hypertension |
| Risk Factors | Age (60 years), male gender, smoking, family history, high blood pressure, high cholesterol |
| Symptoms | Usually asymptomatic; abdominal or back pain, pulsating mass, sudden severe pain (sign of rupture) |
| Diagnostic Methods | Ultrasound, Computed Tomography (CT) angiography, Magnetic Resonance Imaging (MRI), physical examination |
| Treatment Options | Observation (for small aneurysms), Endovascular Aneurysm Repair (EVAR), Open surgical repair |
| Complications | Aneurysm rupture, internal bleeding, insufficient blood flow to organs, embolism, infection |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is an aortic aneurysm and why is it called the “silent danger”?
You can think of the aorta, the largest artery in our body, as a city’s main water pipeline. It takes the clean, oxygen-rich blood pumped from the left ventricle of the heart and delivers it to all organs and tissues, from the brain to our fingertips. After leaving the heart, it travels like the handle of a cane, first upwards and then in an arc downwards, through the chest and abdominal cavity. During this journey, it gives life-giving branches to all our organs. A healthy aorta and intact walls are therefore essential for all our bodily functions.
An aortic aneurysm is a weakening of one part of the wall of this main pipeline and the resulting abnormal enlargement. Just like an old rubber hose balloons outward at a weak point, the wall of the aorta stretches outward and balloons with the constant pressure of the blood flowing through it. For a dilatation to be medically recognized as an aneurysm, the vessel must be at least P larger than its normal diameter in that area.
The most worrying feature of aortic aneurysms is that they can grow completely silently, often without any symptoms. This is why we call it a “silent danger”. Patients may be completely unaware that a potentially life-threatening condition is developing in their body. Once the aneurysm reaches a certain size or its wall becomes even weaker, the most feared complications, rupture (rupture) or separation of the layers of the vessel wall (aortic dissection), can occur. Both of these conditions can lead to sudden and severe internal bleeding, which unfortunately can be fatal. That is why it is vital that people, especially those at risk, are aware of this issue and have regular health check-ups without waiting for symptoms to appear. Early detection is our most powerful weapon against this silent danger.
Which parts of the body are affected by aortic aneurysm?
As the aorta travels a long way, aneurysms can occur at different points along this path. They are basically divided into two main groups according to their location.
The most common sites of an aneurysm are:
- Abdominal Aortic Aneurysm (AAA)
- Thoracic Aortic Aneurysm (TAA)
Abdominal aortic aneurysm (AAA) is the most common type of all aneurysms. It occurs in the part of the aorta that passes through the abdominal cavity and carries blood to our legs, intestines and kidneys. Its incidence increases in men, especially with advancing age, and if it ruptures, it poses a serious public health problem.
A thoracic aortic aneurysm (TAA) develops in the part of the aorta that remains in the chest cavity, that is, in any segment from where it exits the heart to the diaphragm. Although it is rarer than AAA, its risk is increased especially in people with certain genetic diseases or in those with a similar family history. Most of these aneurysms also progress silently and are usually diagnosed by chance during imaging for another reason.
What Are the Most Common Aortic Aneurysm Symptoms?
As we have already mentioned, the vast majority of aortic aneurysms do not cause any symptoms, especially when they are small in size. Therefore, if you have risk factors, it is very important to get checked without waiting for symptoms. However, as the aneurysm grows and starts to put pressure on surrounding organs, it can give some clues.
Possible symptoms for an abdominal (abdominal) aortic aneurysm are
- A deep, constant and gnawing pain felt in the abdomen or sides of the back
- A throbbing or pulsing in the abdomen consistent with the heart, especially when lying down
- Immediate feeling of satiety even with a small amount of food
- Sudden pain, bruising or non-healing wounds on the toes (sign of embolism)
Possible symptoms for a thoracic aortic aneurysm are as follows
- Chest pain radiating to the jaw, neck or between the shoulder blades
- Sticking sensation or pain when swallowing
- Unexplained and increasing hoarseness
- Dry and persistent cough
- Shortness of breath or wheezing
- Swelling of the face, neck or arms
Since these symptoms can be confused with many other diseases, especially people with risk factors should take such complaints seriously and consult a physician.
What Situations Signal an Aortic Aneurysm Complication Requiring Emergency Intervention?
Aneurysm rupture or dissection is an absolute medical emergency in which even seconds count. This means that the wall of the aneurysm can no longer withstand the pressure and ruptures or its layers tear and separate. The chances of survival in such a situation directly depend on how quickly medical help is received.
If any of the following symptoms occur suddenly and severely, the 112 emergency hotline should be called immediately:
- Very severe chest, back or abdominal pain, never experienced before, described as “tearing” or “stabbing”
- Sudden dizziness or fainting
- Pale skin and cold sweating
- Very fast heartbeat (palpitations)
- Sudden onset and severe shortness of breath
- Numbness, weakness or paralysis on one side of the body
- Speech or vision impairment
These symptoms are the body’s way of saying “a major disaster is happening”. In this case, seeking professional help without wasting time is the most correct and life-saving action that can be taken.
What are the Risk Factors Leading to the Development of Aortic Aneurysm?
Aortic aneurysms do not occur due to a single cause; usually, the structural integrity of the vessel wall deteriorates over time due to a combination of multiple factors. The most important cause is atherosclerosis, also known as hardening of the arteries. However, some people are more prone to developing aneurysms due to their lifestyle habits or genetic heritage.
The most important factors that increase the risk of aortic aneurysm are:
- Smoking (the most important and modifiable risk factor)
- Advanced age (especially 65 years and older)
- Male gender (4-6 times more common than women)
- Family history of aortic aneurysm or sudden cardiac death
- Uncontrolled high blood pressure (hypertension)
- Hardening of the arteries (Atherosclerosis)
- Genetic connective tissue diseases such as Marfan syndrome, Loeys-Dietz syndrome
- Presence of a congenital two-leaflet (bicuspid) aortic valve
The most prominent of these factors is undoubtedly smoking. Smoking has a direct toxic effect on the vessel wall, increasing inflammation, accelerating atherosclerosis and significantly increasing the risk of both growth and rupture of an existing aneurysm. Family history is also critical. If a first-degree relative (mother, father, sibling) has an aneurysm, the risk of developing an aneurysm in themselves increases many times compared to the normal population. Therefore, it becomes even more important for people with unchangeable risk factors (age, gender, genetics) to keep the modifiable ones (smoking, blood pressure, cholesterol) under control.
What Methods Are Used to Diagnose Aortic Aneurysm?
We use modern imaging technologies after a detailed medical history and physical examination to make a diagnosis in a patient who presents with a suspected aortic aneurysm or is in a risk group. Although it is possible to detect a palpable, pulsating mass in the abdomen on physical examination, most aneurysms cannot be detected in this way. There are basic imaging methods we use for definitive diagnosis.
These methods are as follows:
- Abdominal Ultrasonography
- Echocardiography (ECHO)
- Computed Tomography (CT) Angiography
- Magnetic Resonance (MR) Angiography
Ultrasound is the most common, radiation-free, painless and practical method for the screening and follow-up of abdominal aneurysms (AAA). Echocardiography is an ultrasound of the heart and is very valuable in evaluating the first parts of the aorta that exit the heart.
If an aneurysm is detected or if surgery needs to be planned, we then resort to Computed Tomography (CT) or Magnetic Resonance (MR) angiography, which provides more detailed anatomical information. These tests show in three dimensions the exact location, size and shape of the aneurysm, the presence of clots or calcification in its wall, and its relationship to important side branches such as the kidney vessels. This detailed mapping allows us to determine the best treatment strategy for each patient.
Who Should Be Screened for Aortic Aneurysm?
Due to the “silent” nature of aneurysms, screening at-risk individuals, even if they have no symptoms, is the most effective way for early detection and life-saving interventions. Screening recommendations are particularly clear for abdominal aortic aneurysm (AAA).
It is strongly recommended that people in the following groups consult a physician for screening:
- all men between 65 and 75 years of age who have smoked cigarettes (more than 100 cigarettes) at any time in their lives
- All individuals (regardless of whether male or female) with a history of aortic aneurysm diagnosis or repair in first-degree relatives (mother, father, sibling)
- People with diagnosed genetic connective tissue diseases such as Marfan syndrome, Loeys-Dietz syndrome
The decision for routine screening for men aged 65-75 years who have never smoked or women who have smoked is made on an individual basis, taking into account the patient’s other risk factors and general health status. If you think you are in a risk group, you should definitely discuss this with your doctor. Remember, a simple ultrasound scan can save your life.
Is Surgery Necessary for Every Detected Aortic Aneurysm?
hearing the word “aneurysm” naturally causes concern, but not every diagnosis of an aneurysm means immediate surgery. In fact, for the vast majority of small and asymptomatic aneurysms, surgery is not our first approach. Instead, we initiate a careful follow-up process, which we call “active monitoring” or “wait and see”.
This process is not to ignore the condition, but to keep the aneurysm under close control. We usually measure the size of the aneurysm with imaging tests (ultrasound or CT) every 6 or 12 months. If the aneurysm remains stable or is growing very slowly, this follow-up can continue for years. Our aim is to catch the “right time” when the risk of the aneurysm rupturing is higher than the risks of a possible surgery. During this waiting period, we focus on medical treatments and lifestyle changes to slow the growth of the aneurysm.
What Can Be Done to Slow Aortic Aneurysm Growth?
The most important part of the active follow-up process is to slow down the growth rate by reducing the pressure on the aneurysm. The active role of our patients in this process is critical for the success of the treatment.
Here are the basic steps that need to be taken:
- Keeping blood pressure at ideal levels (targeting below 130/80 mmHg with medication)
- Lowering bad cholesterol (LDL) (statin group drugs are used)
- Strictly and immediately quit smoking and all tobacco products
- Restricting salt consumption
- Avoiding movements that increase intra-abdominal pressure such as heavy lifting and straining
- Doing regular and light-paced exercises approved by the doctor, such as walking
- Maintaining a healthy weight and eating a heart-friendly (Mediterranean-type) diet
These measures not only slow the growth of the aneurysm, but also improve your quality of life by protecting your overall cardiovascular health.
When Is Aortic Aneurysm Surgery Decided?
We make the decision to operate by weighing the risk of rupture of the aneurysm on one side of the scale and the risks of surgery on the other. When the risk of rupture is high, it is time to intervene.
The main conditions that trigger the decision for surgery are as follows:
- Aneurysm diameter exceeds a certain threshold (usually 5.5 cm in the abdomen, 5.5-6.0 cm in the chest)
- Rapid growth of the aneurysm (e.g. 0.5 cm in 6 months or more than 1 cm per year)
- The appearance of symptoms such as pain due to an aneurysm
- Aneurysm rupture or dissection (emergency)
These thresholds are not absolute. For example, in women or in special cases such as Marfan syndrome, smaller diameters may be recommended. Each patient is evaluated individually and the decision is made together, taking into account the patient’s age, general health and personal preferences.
What is the Traditional Open Aortic Aneurysm Surgery?
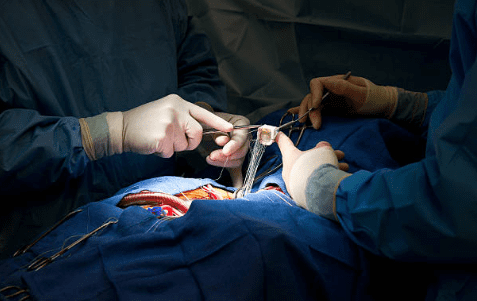
Open surgery is the traditional, proven method of treating aortic aneurysms that has been used for decades. This is literally a major operation and requires serious expertise. The operation is performed under general anesthesia. Depending on the location of the aneurysm, the surgeon makes an incision in the abdomen or chest to access the aorta.
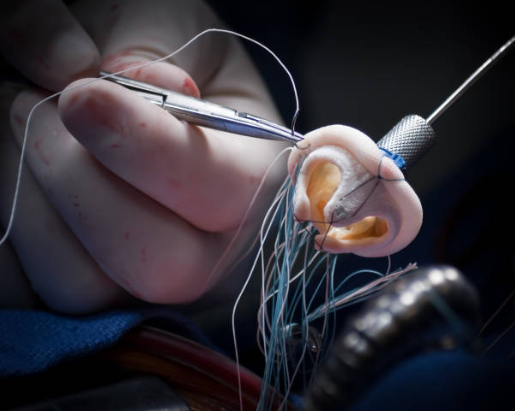
After the blood flow is temporarily stopped, the diseased, ballooned section of blood vessel is completely removed. In its place, a tubular artificial vessel (graft) made of a special synthetic fabric called Dacron is sewn. This new vessel creates a stable and safe pathway for blood flow. When the surgery is completed, blood flow is restored through this new graft.
Open surgery has a longer recovery period. Hospitalization can last up to several days and full return to normal life usually takes several months. Although it is a more arduous process, it may be the best treatment option, especially in young patients in good general health and in some complex aneurysm types, which is still considered the “gold standard” due to its long-term durability.
How is Endovascular Aortic Aneurysm Repair (EVAR/TEVAR), Known as Closed Method?
Thanks to advances in medical technology over the last 20-25 years, we now have the opportunity to treat aortic aneurysms in a much less invasive way. endovascular repair (EVAR/TEVAR), also known as the “closed method”, is performed through small incisions, usually in the groin area, instead of a large surgical incision.
In this technique, a folded stent-graft (a fabric-covered tube with a metal skeleton inside) is advanced through thin tubes called catheters to the site of the aneurysm. Once in the right place under the guidance of X-ray equipment, this stent-graft opens like an umbrella inside the aneurysm and attaches to the vessel wall. The blood continues to flow safely through this new tunnel without ever entering the now weakened aneurysm sac. The ballooned sac is bypassed and the risk of rupture is prevented because the pressure inside is removed.
The most important advantages of this method are:
- A much smaller surgical incision
- Less pain after surgery
- Significantly shorter hospital stay (usually 1-3 days)
- Much faster return to normal activities
However, this method may not be suitable for every patient or every aneurysm type. In addition, the most important feature is that it requires lifelong regular follow-up to maintain the success of the treatment.
How to Choose Between Open and Closed Methods in Aortic Aneurysm Treatment?
This is one of the most common questions our patients ask: “Which method is better for me?” There is no one-size-fits-all answer to this question. The decision is based entirely on the characteristics of the patient and the aneurysm, like a tailor making a tailor-made suit. This is a team decision and the patient is the most important member of this team.
While open surgery is more challenging but may offer a more permanent solution in the long term, there are cases where the endovascular method can be life-saving with a more comfortable healing process, especially for patients with advanced age and additional health problems. When making a decision, we evaluate many factors such as the patient’s age, general health status, life expectancy, anatomical structure of the aneurysm (location, shape, compatibility of the vessels) and the patient’s own preferences. Our goal is to find the safest and most effective solution for each patient.
What Should Be Considered to Keep Quality of Life High After Aortic Aneurysm Surgery?
Aortic aneurysm surgery is not an end but a new beginning to a healthy life. The surgery removes the existing risk, but the responsibility for maintaining vascular health remains for life. the best answer to the question “How long does an aortic patient live?” depends on how well they adapt to this new beginning. With a successful surgery and good follow-up, our patients can lead a normal and long life.
The most important points to be considered after surgery are as follows:
- Regular use of all medications prescribed by your physician (blood pressure, cholesterol, blood thinners, etc.)
- Never neglecting the specified doctor controls and imaging follow-ups
- Adhering to physical restrictions (such as not lifting heavy weights) in the postoperative period
- Eliminating smoking from your life completely
- Maintaining heart-healthy eating habits
- Do not hesitate to share any concerns or new complaints with your doctor.
What to do if there are concerns about an aortic aneurysm?
Aortic aneurysm is a condition that needs to be taken seriously but can be managed effectively thanks to modern medicine. Staying informed, being aware of your own risks and being proactive is the best investment you can make in your health. If you think you are at risk because of your family history, lifestyle or age, or if you have suspicions about an aneurysm, please do not keep these concerns to yourself.
Consulting an expert cardiovascular surgeon is the first step in finding answers to all the questions you have and drawing the right road map for you. Remember, with early diagnosis and proper treatment planning, it is possible to successfully combat this “silent danger” and lead a healthy life.
After Aortic Aneurysm Surgery
| Type of Surgery | Open surgical graft placement or endovascular aortic repair (EVAR/TEVAR). |
| Recovery Time | Open surgery: 15-20 days; EVAR/TEVAR: 5-7 days |
| Physical Activity | Light walking is recommended in the first weeks; heavy lifting and straining are prohibited for 6 weeks. |
| Medication Use | Antihypertensives (especially beta blockers, ACE inhibitors), aspirin or antiplatelets, statins. |
| Blood Pressure Control | The target is usually kept <140/70 mmHg to reduce the load on the aorta. |
| Imaging and Follow-up | CT angiography should be performed annually after open surgery and at 3-6 month intervals in the first year after EVAR/TEVAR. |
| Complications | Endoleak (in EVAR), graft infection, aneurysm recurrence, aortic dissection, renal or spinal ischemia. |
| Wound/Catheter Site Care | Abdominal incision in open surgery and inguinal access sites in EVAR should be monitored for infection. |
| Nutrition | A low-salt, low-fat, fiber-rich diet that supports vascular health is recommended. |
| Smoking and Alcohol | Strongly discouraged; increases the risk of aortic disease and vascular complications. |
| Sexual activity | It can usually be started after 4-6 weeks, once physical recovery is achieved. |
| Psychological Support | Anxiety and depression are common in patients recovering from major surgery; counseling is recommended. |
| Vehicle Use | It can usually be started within -5-20 days after open surgery and 7-10 days after EVAR. |
| Controls | Cardiovascular surgery and radiology follow-up should continue at regular intervals throughout life. |
Frequently Asked Questions
What are the symptoms of aortic aneurysm?
Aortic aneurysm usually progresses asymptomatically for a long time. In the abdomen, there may be a mass around the navel that beats with the heart or persistent abdominal and back pain. In the chest area, symptoms may include sudden and sharp chest, back or shoulder pain, shortness of breath and difficulty swallowing. These symptoms should be taken seriously and a specialist should be consulted.
How long does a ruptured aortic artery live?
A ruptured aorta is a very urgent and life-threatening situation. Life is measured in seconds and minutes; most patients die before reaching the hospital. Survival depends on getting to a full-fledged center quickly and undergoing emergency surgery. Our goal is to intervene before it gets to that point.
Can aortic aneurysm heal?
Unfortunately, once an aortic aneurysm has formed, it does not resolve or shrink on its own. The weakening of the vessel wall is permanent and can grow over time. The aim of treatment is to slow the growth and, when it reaches a dangerous size, to repair it surgically.
How old does aortic aneurysm occur?
It can occur at any age, but is most common in men after the age of 65. Smoking, family history of aneurysms and high blood pressure are the main factors that increase the risk. Regular check-ups are recommended, especially for those in the risk group.
Is aortic vessel dilatation considered 4 cm?
Yes, we consider a 4 cm dilatation of the abdominal aorta to be a “small aneurysm”. Normally, this vessel is 2-2.5 cm. enlargements over 3 cm require follow-up; 4 cm should be checked with regular ultrasound or CT scans. Aneurysms of this size have a low risk of rupture but should be monitored closely.
Does aortic aneurysm show up on ECHO?
Echocardiography (ECHO) is particularly effective in detecting aneurysms in the first part of the heart (ascending aorta). However, aneurysms further into the abdominal or thoracic cavity require additional imaging methods such as ultrasound or CT scan.
Does a ruptured aortic artery live?
It is a very urgent situation and requires rapid intervention. Most patients die before reaching the hospital. However, those who reach the hospital quickly and are operated on urgently have a chance of survival. This is one of the most challenging and time-consuming aspects of surgery.
How many cm does the aorta tear?
Although it varies in each patient, generally, when the diameter of the abdominal aorta reaches 5.5 cm, the risk of rupture increases and surgery is recommended. In the thoracic aorta, this limit is usually 6 cm. The growth rate and shape of the aneurysm are also important in the decision to operate.
Can aortic aneurysm be felt by hand?
Yes, in thin people and when an abdominal aortic aneurysm enlarges, it can be felt by hand as a pulsating mass around the navel. Aneurysms in the chest cannot be felt by hand because of the bone and muscle tissue.
How to tell if you have an aneurysm?
It is usually detected incidentally during imaging for another reason. If there is any doubt, a definitive diagnosis is made by ultrasound, computed tomography (CT) or MRI. Regular screening is of great importance in high-risk individuals.
Is aortic artery surgery risky?
As with any major surgery, there are risks. However, the risk of planned surgery is much lower than if the aneurysm is left alone and ruptures. With closed (EVAR/TEVAR) and surgical techniques, operations can now be performed much more safely.
Can aortic aneurysm be seen on ultrasound?
Yes, aortic aneurysms, especially in the abdomen, can be diagnosed and monitored quickly and effectively with ultrasound. It is also commonly used as a screening test because it is radiation-free and easy to perform.
Which department treats aortic aneurysm?
Cardiovascular Surgery is responsible for the diagnosis, follow-up and surgical treatment of aortic aneurysm. Cardiology can help with diagnosis and management of risk factors. Surgery and follow-up are mainly the domain of cardiovascular surgeons.
What should people with aortic aneurysm pay attention to?
Keep your blood pressure within the limits recommended by your doctor. If you smoke, quit smoking. Avoid heavy lifting, straining and sudden exertion. Keep your follow-up appointments. Lifestyle changes and regular check-ups can greatly reduce the risks.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Prof. Dr. Yavuz Beşoğul » General » Heart Disease: Types, Causes, and SymptomsHeart diseases are [...]
Aug
How the Heart Works
Prof. Dr. Yavuz Beşoğul » General » How the Heart WorksThe heart functions as a [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Prof. Dr. Yavuz Beşoğul » General » How Many Hours Does Heart Valve Surgery Take?Heart [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Prof. Dr. Yavuz Beşoğul » Coronary Artery Bypass » How long does coronary artery bypass [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Prof. Dr. Yavuz Beşoğul » Kalp Kapak Hastalıkları » Kalp Kapak Değişimi Ameliyatı Nedir? Kalp [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Prof. Dr. Yavuz Beşoğul » General » Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki [...]
Aug
Life After Heart Valve Surgery
Prof. Dr. Yavuz Beşoğul » General » Life After Heart Valve SurgeryLife after heart valve [...]
Aug
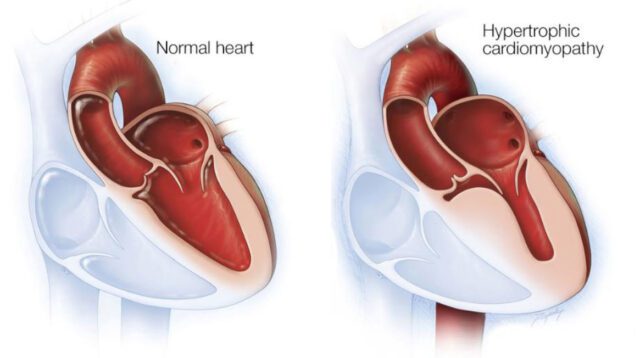
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Prof. Dr. Yavuz Beşoğul » General » Hypertrophic Cardiomyopathy: Symptoms & TreatmentHypertrophic cardiomyopathy is a [...]
Aug