Transcatheter Aortic Valve Implantation (TAVI) is a minimally invasive procedure performed without open-heart surgery. It is primarily used in patients with severe aortic stenosis who are at high surgical risk, providing an effective alternative treatment option.
TAVI indications include elderly patients with comorbidities where open-heart surgery may be risky. The procedure involves inserting a new valve via catheter, often through the femoral artery, ensuring shorter recovery times and reduced complications.
The advantages of TAVI include shorter hospital stays, faster return to daily activities, and lower risk of infection. It has become a preferred method in cardiology for patients unsuitable for traditional surgical valve replacement.
Possible risks of TAVI include bleeding, vascular complications, and arrhythmias. Careful patient selection, advanced imaging, and multidisciplinary evaluation are essential to minimize complications and achieve optimal outcomes.
| Medical Name | Transcatheter Aortic Valve Implantation (TAVI) |
| Frequent Use Areas | – Patients with aortic valve stenosis and high risk of open heart surgery – Elderly and individuals with comorbidities |
| Causes | – Severe aortic valve stenosis – Patients not suitable for open surgery or at high risk |
| Risk Factors | – Old age- Chronic cardiovascular disease- Renal failure- Previous heart surgery- Diabetes, hypertension |
| Complications | – Vascular injury – Bleeding – Heart rhythm disorders (block, arrhythmia) – Stroke – Valve displacement or leakage |
| Diagnostic Methods | – Echocardiography- Cardiac CT- Angiography- ECG- Blood tests |
| Treatment Methods | – Insertion of a new aortic valve intravenously through a groin or small incision – Post-procedure antiplatelet and anticoagulant therapy |
| Prevention Methods | – Management of underlying risk factors- Regular cardiology follow-up- Healthy lifestyle and exercise |
Who Is TAVI Heart Valve Surgery an Option?
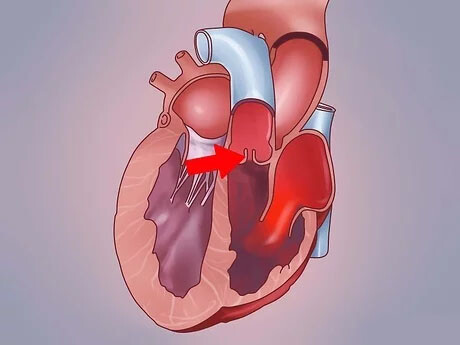
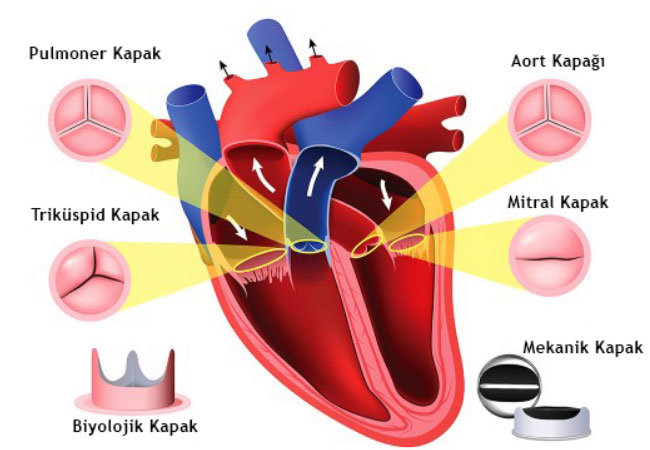
In order to understand the answer to this question, it is first necessary to understand the source of the problem, aortic stenosis, in simple terms. Imagine the aortic valve as a door at the exit of the main pipe that carries clean blood from the heart to the whole body. With age, the hinges of this door can become calcified and rusted. The door becomes narrow and cannot open fully. The heart has to exert more and more effort every day, every hour, every beat, to get the blood through this narrow door. After a while it gets tired and the whole body starts to suffer.
This usually leads to the following complaints in our patients:
- Shortness of breath
- Chest pain
- Dizziness and fainting
When any of these symptoms occur, the situation is serious and treatment should not be delayed. This is exactly where TAVI is a modern solution. Whereas open heart surgery used to be the only option, now with TAVI we can help a much wider range of patients.
So, for whom is TAVI particularly considered? Current medical approaches prioritize several main groups in patient selection. Especially in patients over the age of 80, TAVI is usually the first choice, as the body may not be able to handle the stress of major surgery. Similarly, TAVI is the most logical option for patients who are 75 years of age or older or younger but who have serious conditions in other organs such as the lungs or kidneys, i.e. who are at high surgical risk.
patients between 65 and 80 years of age are in a slightly different situation. In this age range, TAVI and open heart surgery (SAVR) are two valid and effective treatment methods. At this point, the decision is not made by a single physician but by a “Heart Team” together with the patient. The patient’s general health, whether the vascular structure is suitable for TAVI, expectations and his/her own preferences play a decisive role in this decision. It should not be forgotten that for some patients (e.g. very young patients with no other health problems) open surgery may still be the best option due to the proven very long term results. This is a completely personal decision.
How is Patient Evaluation and ‘Heart Team’ Decision Made for TAVI?
Deciding whether a patient is suitable for TAVI is like putting the pieces of a puzzle together. It is not a decision made by a single doctor looking at a single film. On the contrary, it is like a council meeting where physicians from different specialties come together and discuss every aspect of the patient. We call this approach the “Heart Team” and it is an indispensable safety and quality standard of modern cardiac care. This team includes physicians such as interventional cardiologists, cardiovascular surgeons, cardiac anesthesiologists and imaging specialists:
The evaluation of this team consists of several basic steps:
- Listening to the patient’s complaints
- Confirmation of valve stenosis by echocardiography (ECHO)
- Calculation of surgical risk scores
- Examination of vascular and valve structure with tomography
- Control of other organ functions
The assessment process starts with listening to the patient’s story. Details such as the difficulties he or she is experiencing, when he or she stops breathing and the character of the pain in the chest are very valuable for us. Echocardiography (ECHO) is then used to clearly show the degree of stenosis and how much the heart is affected.
Then, internationally recognized risk calculation systems (such as STS and EuroSCORE) are used to mathematically predict the risk that a patient may face if they undergo open heart surgery. However, these scores do not tell everything. What is important for us are the factors that the scores cannot measure. For example, the patient’s “frailty”. Frailty is when a patient’s walking speed slows down, when they have difficulty getting up from a chair without support, or when they have low physical resistance in general. Even with a low risk score, it can be difficult for a frail patient to recover from major surgery. TAVI offers a great advantage in this patient group.
The most critical and technological step in the evaluation is computed tomography (CT). The CT scan is like a road map for us. Thanks to this detailed imaging, we can measure the dimensions of the annulus (the ring in which the aortic valve to be replaced sits) with a precision of one tenth of a millimeter. This measurement is vital for choosing the right size valve. Too small a valve can lead to leakage and too large a valve can cause tissue damage. The CT scan also completely maps the arteries in the groin, the arterial pathway through which the valve is delivered to the heart. The diameter, calcification and tortuosity of the vessels are examined to determine whether the procedure can be performed safely. In the light of all this information, the Heart Team convenes and decides on the right, safest and most effective treatment for the patient.
Non-Surgical Aortic Valve Replacement What Are the Main Differences Between TAVI and Open Heart Surgery?
The aim of both methods is the same: to replace the dysfunctional aortic valve with a new one. However, the paths they follow to achieve this goal, the patient’s experience and the speed of recovery are as different as night and day.
The main difference is the way it enters the body. In open heart surgery, the sternum, also known as the breastbone, is cut through the sternum to access the heart. This is a major surgical trauma and takes weeks or even months to heal. In TAVI, the entire procedure is usually performed through a small incision of about 1 centimeter in diameter in the groin artery. The rib cage is never opened, no bone is cut.
The second major difference is that the procedure is performed according to the condition of the heart. During open surgery, the heart is stopped and the patient is connected to a heart-lung pump to maintain body circulation. This is a burden for the body. In TAVI, the entire procedure is performed while the heart continues to function normally. No heart-lung pump is used. This significantly reduces the stress and risks of the procedure on the body.
These two fundamental differences directly affect the recovery process. A patient who undergoes open surgery usually stays in the hospital for more than a week, and after discharge, needs a long recovery period for the sternum to fuse and the pain to subside. A TAVI patient, on the other hand, can usually be discharged from the hospital within 1 to 3 days and can return to their daily life, walking and social activities within a few days. This rapid recovery is invaluable, especially for our elderly patients to maintain their general fitness and quickly regain their grip on life.
Of course, each procedure has its own advantages and disadvantages. For example, the need for permanent pacemaker implantation is slightly higher in TAVI than in open surgery because the frame of the new valve presses on the heart’s electrical system. On the other hand, surgical valves used in open surgery have decades of proven long-term durability data. Although the 8-10 year results of TAVI valves are excellent, since the technology is newer, 20-year data is not yet available. Therefore, when choosing a treatment, we weigh all these factors and choose the method that offers the greatest benefit for the patient.
How is TAVI, Also Known as Heart Valve Replacement by Angiography?
The answer to the question “How is TAVI performed?”, which is frequently asked by our patients, is actually a process consisting of highly organized and meticulous steps, combining technology and experience. You can think of the process as scenes from a movie:
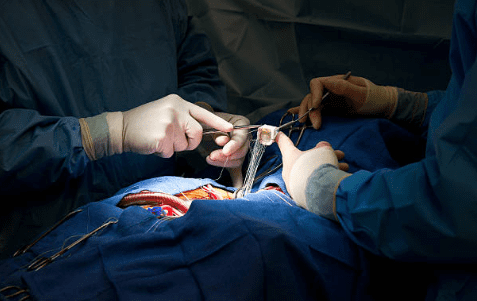
It all starts with our patient being taken to a special room, which we call the hybrid operating room or angiography lab. General anesthesia is usually not necessary. A mild sedative is administered intravenously to relax the patient and make the procedure comfortable. The groin area where the procedure will be performed is completely numbed with a local anesthetic needle. This way, the patient remains awake throughout the procedure but does not feel any pain.
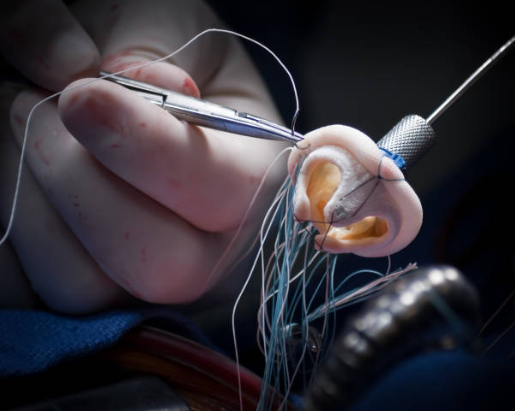
The most common route is the main artery in the groin (femoral artery). Under ultrasound guidance, a needle is inserted into this vessel. This step is very similar to a normal angioplasty procedure. A thin sheath is then inserted through this access hole, through which the catheters that will extend to the heart can pass. It’s like the starting toll booth of the highway to the heart:
Through this sheath, a thin catheter with a curved tip and a much thinner, soft-tipped guidewire is inserted. This wire travels up the aorta, the body’s main artery, to the heart. The aim is to pass through the small gap in the narrowed aortic valve and enter the left ventricle of the heart. This is one of the most delicate maneuvers of the procedure. Once this soft wire has passed, it is replaced by a much harder and more supportive guide wire with a specially shaped tip, almost like a rail system. We now have a solid “rail” on which our new valve will slide:
The new heart valve is crimped to the thickness of the tip of a pencil in a special process and is ready at the end of its own carrier system. This system is inserted through a sheath in the groin, guided over a “rail” wire and inserted into the old, calcareous valve. Under X-ray (fluoroscopy), the ideal position is found with millimetric adjustments. Once the position is confirmed, the deployment phase begins.
Balloon Expanding Closures: If this type of valve is used, the balloon at the end of the system is inflated. The expanding balloon opens the metal frame (stent) of the new valve, pushing the old valve towards the edges and ensuring that it fits tightly into place.
Self-Expanding Closures: These caps are made of a special metal alloy (Nitinol) and when the cover is pulled back, they automatically return to their pre-programmed shape. They open slowly and in a controlled manner and settle into place.
Once the new cover is in place, the conveyor system is retracted. Immediately afterwards, checks are carried out to make sure that the new valve is working perfectly. A contrast medium is injected via angiography to check for leaks at the edges of the valve. Intracardiac pressures are measured. Once everything is confirmed to be in order, the access site in the groin is closed with special stitched closure devices placed at the beginning of the procedure. A small bandage is placed over it. And the procedure is completed. After a few hours of observation, the patient is taken to his/her room and is usually well enough to return home the next day.
What are the Risks and Possible Complications of TAVI Surgery?
As with any effective medical intervention, TAVI has potential risks that need to be managed. Talking openly and honestly about these risks is an important part of the treatment process. With the increase in technology and experience, many of these risks have been reduced to very low levels.
The main potential risks and complications are:
- Stroke (paralysis)
- The need for a permanent pacemaker
- Vascular access site problems
- Bleeding
- Leakage from the lid edge
Let us now explain these risks in a little more detail. The risk of stroke is the most worrisome complication. It occurs when tiny particles that may break off from the old calcareous valve or aortic vessel during the procedure travel to the brain. In today’s TAVI procedures, this risk is around 1-3%. To further reduce this risk, especially in high-risk patients, we can use special protection devices such as “filters” that protect the vessels leading to the brain during the procedure.
The need for a permanent pacemaker is the most common condition after TAVI. The metal frame of the newly implanted valve comes into close contact with the heart’s own electrical system. In some patients, this contact can slow down the heart’s rhythm. If this slowing becomes permanent, a pacemaker may need to be implanted to regulate the rhythm. Depending on the model of valve used and the patient’s own heart structure, this probability can vary between 5% and %5.
Vascular access site problems are complications that can occur in the inguinal artery where the procedure is performed. These can include bleeding, rupture of the vessel or clotting. This risk is about 5-10% and usually occurs in patients with very calcareous or thin veins. However, we are now able to treat the majority of such problems with angiographic methods, i.e. closed stents or balloons.
Valve edge leakage (Paravalvular Leak – PVL) is a condition where the new valve does not fit the patient’s anatomical structure and leaks some blood from the edges. This problem, which was more common with older generation valves, has been largely solved with the new generation of valves with a “skirted” design. The risk of serious leakage is now very low.
So, What are the Comments of Those Who Have TAVI Surgery?
While scientific data and statistics are very important to us, it is the real change in our patients’ lives that really shows the success of the treatment. Reviews from those who have had TAVI surgery often focus on how fast and dramatic this change has been. As a team that has been practicing this treatment for years, the feedback we have received from our patients and scientific studies generally converge on the following points:
- Fast recovery
- A painless process
- Disappearing shortness of breath
- Re-engagement in life
- Increased self-confidence
The most common thing our patients say is that the recovery process is surprisingly fast. One of the greatest comforts for them is that TAVI does not cause chest pain, restricted mobility and fatigue that can last for months after open heart surgery. It is a priceless source of happiness to be able to return home in a few days and continue their daily lives pain-free with their loved ones.
Another important feedback is the sudden disappearance of the shortness of breath that has been a nightmare for years. we often hear sentences such as “Sir, for the first time in years I was able to climb a hill”, “Now I can play with my grandchild without getting out of breath”, “I don’t wake up at night with the feeling of suffocation in bed”. This is not only a physical relief but also a great psychological freedom. Regaining lost functions gives patients great self-confidence and joy of living.
Being able to participate in life again is also very valuable. Activities that used to be a dream, such as going shopping, meeting friends and traveling, become possible again after TAVI. This social revitalization has a positive effect on both the mental and physical health of our patients. In short, the comments after TAVI are not just about solving a medical problem; it is also the story of regaining a lost life, breathing again and hope.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.