Degenerative valve disease refers to progressive structural changes in heart valves due to aging, leading to calcification, thickening, or prolapse. These alterations impair valve function, causing stenosis or regurgitation over time.
Symptoms often include exertional shortness of breath, fatigue, chest discomfort, and reduced exercise tolerance. The condition can remain silent for years until significant valve dysfunction develops.
Echocardiography is the primary tool for diagnosing degenerative valve disease, assessing severity, and guiding treatment decisions. Advanced imaging modalities may provide further anatomical detail when surgical planning is required.
Treatment strategies range from medical management in mild cases to surgical valve repair or transcatheter replacement in advanced disease. Early recognition and timely intervention are crucial for improving long-term outcomes.
| Definition | Loss of function in heart valves due to structural deterioration caused by aging, mechanical stress and connective tissue weakness |
| Most Frequently Held Cover | Mitral and aortic valves; the most common forms are mitral valve prolapse and calcific aortic stenosis |
| Causing Factors | Aging, myxomatous degeneration, calcification, connective tissue diseases, hemodynamic stress |
| Risk Factors | Advanced age, hypertension, dyslipidemia, connective tissue diseases, genetic predisposition |
| Symptoms | Dyspnea, palpitations, chest pain, fatigue, syncope, signs of heart failure; may be asymptomatic in early stages |
| Diagnostic Methods | Transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), ECG, chest radiography, CT/MRI if necessary |
| Complications | Heart failure, arrhythmia, endocarditis, thromboembolic events, sudden death |
| Treatment Methods | Medical treatment (diuretics, ACE inhibitors, beta-blockers), surgical intervention (valve repair or replacement), TAVI (especially for aortic stenosis) |
| Follow-up and Monitoring | Follow-up of valve function with regular ECHO, symptom monitoring, cardiologist control |
| Ways of Prevention | No specific prevention methods; management of risk factors, regular cardiac monitoring, recognition of conditions that may require endocarditis prophylaxis |
What is Degenerative Valve Disease and which valves of the heart does it affect?
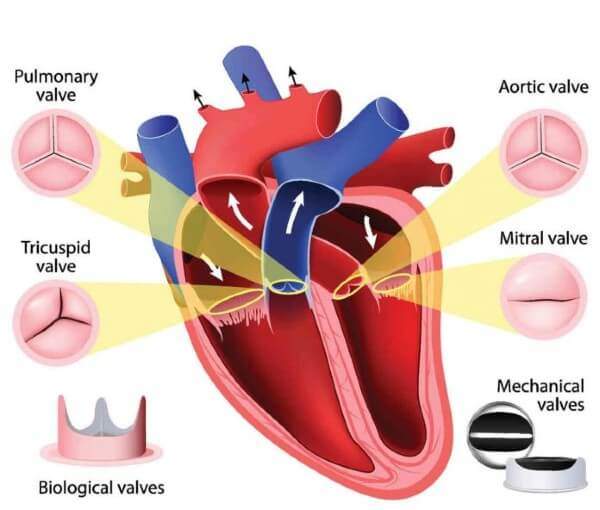
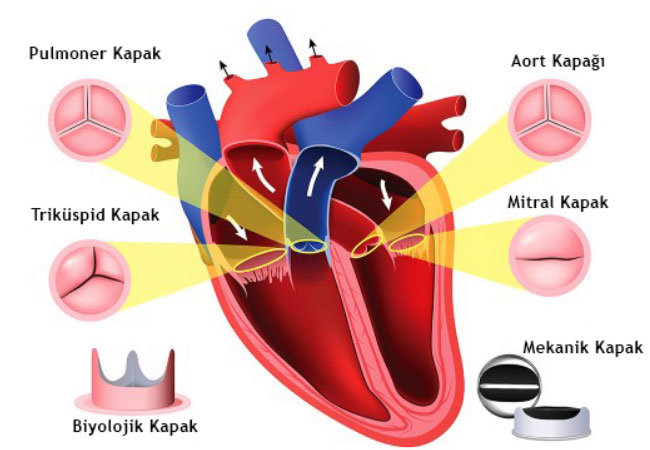
We can think of degenerative valve disease as the wear and deterioration of the one-way valves in the heart over time. There are four valves in our heart that keep the blood flowing in the right direction. These are the Aortic, Mitral, Tricuspid and Pulmonary valves. With each heartbeat, these valves open and close once, allowing blood to flow regularly between the chambers and from the heart to the body. When the disease develops, the mechanism of these gates is disrupted.
This distortion usually leads to two main problems.
- Stenosis (Stenosis): The valves thicken and harden and can stick together. This makes the valve unable to open and narrows the space for blood to pass through. The heart has to exert much more force than normal to move blood through a narrowed valve. Over time, this leads to fatigue of the heart muscle.
- Regurgitation: The valves cannot close tightly. Therefore, instead of being pumped forward, some of the blood leaks backwards into the chamber from which it came. This is known as heart valve regurgitation. Because the heart has to pump the same blood over and over again, the workload increases and the effective amount of blood to the body decreases.
In addition to these two main problems, prolapse of the mitral valve is also an important degenerative problem. In prolapse, the valves relax and lose their elasticity and bulge backwards like a parachute when the heart contracts. This is often the basic mechanism underlying mitral valve regurgitation (leakage).
Although degenerative changes can affect any valve of the heart, they are most common on the left side, which pumps blood throughout the body and is therefore subject to the highest pressure. These are the aortic valve, which usually causes stenosis, and the mitral valve, which usually causes regurgitation.
What causes Degenerative Valve Disease and what are the main risk factors?
The main cause of degenerative valve disease is the natural wear and tear of the valve tissue due to the mechanical stress it has been exposed to over the years. But there are other factors that can accelerate or trigger this process.
The main risk factors involved in the development of the disease are:
- Advanced age
- Congenital valve anomalies (e.g. aortic valve with two leaflets instead of three)
- Previous rheumatic fever
- Infective endocarditis (infection of the heart valves)
- High blood pressure (Hypertension)
- High cholesterol
- Diabetes (Diabetes)
- Chronic kidney disease
- Connective tissue diseases such as Marfan syndrome
- Previous heart attack
- Cardiomyopathy (heart muscle diseases)
- Radiation therapy to the chest area
Especially for those who wonder what aortic valve degenerative means; this is an active disease process that usually means the hardening and narrowing of the valve as a result of calcium deposition and calcification on the valves due to risk factors such as age, high blood pressure and cholesterol.
What are the symptoms of degenerative valve disease and when should you see a doctor?
One of the most misleading aspects of this disease is that it can progress insidiously for many years without any symptoms, despite being moderate or advanced. Most of the time, the disease is discovered by chance when a doctor hears an abnormal “murmur” while listening to the heart with a stethoscope during an examination for another reason.
Symptoms that may occur when the disease progresses are as follows:
- Shortness of breath, especially with exertion
- A feeling of fatigue and weakness above normal
- Difficulty in activities that used to be done comfortably
- Chest pain or a feeling of tightness in the chest
- Dizziness
- Fainting (especially during exertion)
- Feeling that the heart beats irregularly, rapidly or strongly (palpitations)
- Swelling in the ankles, legs or abdomen
If any of these symptoms are new or if you notice a worsening of your existing symptoms, it is important to contact a doctor to assess the situation. The sudden onset of severe shortness of breath, chest pain radiating to the arms or fainting requires urgent medical attention.
What problems does an untreated Degenerative Valve Disease cause in the body?
Left untreated, degenerative valve disease can cause serious and life-threatening complications by constantly forcing the heart to work harder. This is where the answer to the common patient question “can mitral valve insufficiency kill?” lies. Yes, untreated advanced valvular disease can trigger a series of life-threatening problems as the heart’s compensatory mechanisms are exhausted.
Initially, the heart thickens or expands to accommodate this extra load. However, this does not last forever. Over time, the overtaxed heart muscle weakens and the following serious complications can occur:
- Heart failure
- Stroke
- Blood clots
- Rhythm disorders such as atrial fibrillation
- Pulmonary hypertension (increased pressure in the pulmonary vessels)
- Sudden cardiac death
These problems illustrate how serious systemic consequences can result from what initially starts as a mechanical valve problem. Timely intervention before symptoms start or progress is therefore vital to break this chain reaction.
What structural changes does degenerative mitral valve disease cause in the heart?
The main problem in degenerative mitral valve disease is the deterioration of the structure of the tissue that forms the valve. In this process called myxohematous degeneration, the normally tight and durable connective tissue structure of the valve weakens and becomes spongy and loose. This is the main cause of what is popularly known as “valve collapse” or “loose valve”.
This weakening disrupts the integrity of the valves and the filamentous structures (chordae) that hold them. When the heart contracts, the weakened valves bulge back into the left atrium, a condition called prolapse. If the condition progresses further, one or more of the threads holding the valve in place may break. The rupture of the chordae causes the edge of the valve to become completely free and flutter uncontrollably. This often leads to sudden and severe valve leakage. These structural defects form the basis of mitral valve insufficiency.
How does calcification and inflammation progress in Degenerative Aortic Valve Disease?
For many years, aortic stenosis was thought to be a passive process of “wear and tear”, like the wear and tear of a machine part over time. Today, however, we know that this is a biologically active disease process, very similar to atherosclerosis.
The progression of this process usually follows these steps:
- Damage and Fat Accumulation: The process begins when the delicate layer lining the inner surface of the valve (the endothelium) is damaged by the mechanical stress of high blood flow. This damaged surface allows fat molecules such as “bad” cholesterol to leak into the valve tissue.
- Inflammation: The body’s immune system responds to these fats leaking into the valve tissue as a threat. Inflammatory cells accumulate in the area and this chronic inflammatory response triggers disease progression.
- Calcification: Chronic inflammation changes the structure of the cells in the valve tissue so that they resemble bone-forming cells. These cells begin to deposit calcium crystals. As a result, the valves, which should be flexible, become thick, hard, calcareous and limited in mobility over time.
How is Degenerative Valve Disease diagnosed?
The diagnostic process begins with listening to the patient’s complaints, questioning risk factors and a thorough physical examination. The most important finding of the examination is the abnormal sound called a “murmur”, which is usually heard while listening to the heart with a stethoscope. This is the sound of turbulent blood flow through the diseased valve and may be the first clue to valve disease:
- After the physical examination, some basic tests are performed to confirm the suspicion and determine the severity of the disease.
- Electrocardiogram (ECG)
- Chest X-ray
After these initial assessments, further tests are carried out to see details such as the type and severity of the disease and the heart’s response to it.
Why is echocardiography (ECHO) so important in the evaluation of Degenerative Valve Disease?
Echocardiography is an ultrasound method that uses sound waves to create moving images of the heart and is considered the “gold standard” for diagnosing valve diseases. This painless and harmless test provides a lot of critical information in a single session.
The basic information provided by echocardiography is as follows:
- Detailed structure of the covers
- Thickening, calcification or prolapse of the valves
- Lid opening and closing function
- Severity of stenosis or insufficiency
- Blood flow rate and direction
- Dimensions of the heart chambers
- Overall pumping power of the heart (ejection fraction)
Depending on clinical need, different types can be used, such as standard chest (Transthoracic), more detailed esophageal (Transesophageal) or exertional (Stress Echocardiography).
When are advanced imaging modalities such as Cardiac MRI and CT used in the diagnosis of Degenerative Valve Disease?
Echocardiography is the main diagnostic tool, but sometimes more detail is needed. In these cases, other advanced imaging modalities offered by modern medicine come into play.
- Cardiac Magnetic Resonance (Cardiac MRI): This test is used to measure the amount of valve leakage very precisely, especially when echocardiographic findings are inconclusive. It is also very valuable in detecting the presence of scar tissue (fibrosis), a sign of irreversible damage to the heart muscle.
- Cardiac Computed Tomography (CT): This is used to quantify the amount of calcium in the aortic valve and to plan catheterized valve replacement procedures such as TAVR. Before TAVR, it provides precise measurements and three-dimensional mapping of the valve, aortic and groin vessels, ensuring that the procedure can be performed safely.
Are there non-surgical treatment options for Degenerative Valve Disease?
Yes, not every valve disease diagnosis means immediate surgery. Especially in cases where the disease is mild or moderate and not yet symptomatic, treatment includes regular medical follow-up, lifestyle changes and medication. At this point, the question “what should people with mitral valve insufficiency pay attention to?” becomes important.
Lifestyle changes to be aware of include:
- Salt-poor diet
- Reducing saturated fat and sugar consumption
- A diet rich in fruits, vegetables and whole grains
- Regular exercise approved by the doctor
- Maintaining ideal weight
- Complete smoking cessation
Medication does not correct the mechanical problem in the valves. However, by controlling symptoms, lowering blood pressure and regulating rhythm disturbances, it reduces the heart’s workload and improves the patient’s quality of life.
Why is valve repair better for the treatment of Degenerative Mitral Valve Disease?
When it comes to the treatment of degenerative mitral valve insufficiency, i.e. mitral valve insufficiency, the generally accepted principle among surgeons and cardiologists is this: If a valve can be repaired, it should be repaired. Mitral valve repair is considered the “gold standard” compared to valve replacement.
The advantages of repair over valve replacement are as follows:
- Lower operation risk
- Better long-term survival
- Better preservation of the natural structure and function of the heart
- Lower risk of complications such as blood clots and infection
- No obligation to take blood thinners for life
For these reasons, the ability to perform a successful repair is a key factor even in the decision of when to perform surgery. An experienced surgeon can offer repair surgery before the patient’s heart is irreversibly damaged, allowing the patient to live a longer and healthier life.
What are the surgical options for Degenerative Aortic Valve Disease?
Unlike the mitral valve, the standard treatment for degenerative aortic valve disease is usually valve replacement, not valve repair. The main reason for this is the nature of the disease. Degenerative aortic stenosis is a process in which the valve calcifies and hardens, and it is technically impossible to restore this “petrified” tissue to a normal, flexible structure. Therefore, the most effective and permanent solution is to surgically remove the damaged valve and replace it with a prosthetic valve.
What are the valve types used in Degenerative Valve Disease surgery?
When valve replacement is necessary, one of the most important decisions you and your surgeon need to make is which type of prosthetic valve to use. There are two main options.
- Mechanical Covers: They are produced from very durable materials such as carbon. They are expected to last a lifetime. Due to these features, they reduce the possibility of reoperation, especially for young patients. Their most important disadvantage is that patients have to take blood thinners for life to prevent the risk of clots.
- Bioprosthetic (Tissue) Valves: They are usually made from bovine or porcine heart tissue. Their biggest advantage is that they do not require lifelong use of blood thinners. Their biggest disadvantage is their limited durability. They usually wear out within 10-20 years and require re-intervention. This wear and tear process tends to be faster in younger patients.
What are the advantages of minimally invasive and robotic Degenerative Valve Disease surgery?
Traditional heart surgery involves cutting through the breastbone. While this is a safe procedure, the recovery can be long. Modern surgery offers minimally invasive techniques that make this process much more comfortable for patients. Instead of cutting through the breastbone to reach the heart, the surgeon uses a small incision between the ribs. Robotic surgery is the most advanced form of this approach.
The main benefits of these modern approaches for patients are:
- Faster healing process
- Shorter hospital stay
- Less pain after surgery
- Lower risk of bleeding and infection
- Better cosmetic results
Robotic surgery, with its three-dimensional image and superior maneuverability, allows for more precise and successful mitral valve repairs, especially complex mitral valve repairs.
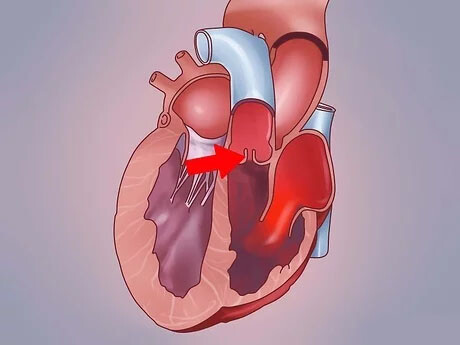
How is Transcatheter Aortic Valve Replacement (TAVR) a method for the treatment of Degenerative Valve Disease?
Transcatheter Aortic Valve Replacement (TAVR or TAVI) has revolutionized the treatment of aortic stenosis. In this procedure, a thin tube (catheter) is inserted through an artery, usually in the groin, without opening the rib cage. A new compressed bioprosthetic valve is advanced through this catheter to the heart, where it is expanded by inserting it right into the diseased, calcified aortic valve. The new valve replaces the old valve by pushing it to the edges and immediately restores blood flow.
Initially only an option for patients at very high risk for open heart surgery, TAVR has now become a treatment option for patients in all surgical risk groups thanks to large clinical trials. The decision on which treatment (TAVR or surgery) is best for you is made by a “Heart Team” consisting of a cardiologist and a heart surgeon.
What is the recovery process after Degenerative Valve Disease surgery?
Full recovery after heart valve surgery requires time and patience. While traditional open surgery takes 6-8 weeks to recover, minimally invasive methods are significantly shorter. One of the most important parts of this process is a structured Cardiac Rehabilitation program. This program is not just about exercise; it is a comprehensive approach aimed at physical, educational and psychological recovery.
The components of the program include:
- Individualized exercise plan under medical supervision
- Heart-friendly nutrition training
- Information on the correct use of medicines
- Stress management techniques
- Psychological counseling and emotional support
Cardiac rehabilitation is scientifically proven to reduce the risk of future heart problems and significantly improve quality of life.
What are the long-term expectations and quality of life after Degenerative Valve Disease surgery?
The ultimate goal of a successful heart valve surgery is not only to correct a mechanical problem but also to enable patients to return to a full and active life. The surgery provides a significant improvement in quality of life by eliminating restrictive symptoms such as shortness of breath and fatigue. Successful surgery significantly prolongs life expectancy and offers a near-normal life expectancy for many patients.
Life after surgery requires regular follow-up. It is therefore vital to maintain regular check-ups with your cardiologist. Long-term follow-up should be considered as follows:
- Regular echocardiographic monitoring of the condition of bioprosthetic valves
- Lifelong monitoring of blood thinner levels in patients with mechanical valves
- Adhering to lifestyle changes to maintain overall heart health
Degenerative valve disease is a serious but highly treatable condition. Navigating this promising path of modern treatment requires a strong partnership between an informed patient and a specialized Heart Team that can offer a full range of options. This partnership will help you choose the right path to a long and healthy life.
Frequently Asked Questions
What is degenerative valve disease?
It is a condition in which the heart valves undergo structural deterioration with age and cannot fully perform their functions.
Which valve is most commonly affected?
The mitral valve and aortic valve are the most commonly affected heart valves.
What causes this disease?
Aging, connective tissue weakness, genetic predisposition and rheumatic diseases can be the cause.
What are the symptoms?
Shortness of breath, fatigue, palpitations, chest pain, dizziness and fainting are common symptoms.
Are there stages of the disease?
Yes, there are mild (follow-up), moderate (medication) and severe (surgery may be needed) stages.
How is it diagnosed?
Echocardiography (ECHO) is the most basic diagnostic tool. Detailed examination with cardiac MRI or catheterization can be performed if necessary.
Can valve insufficiency and stenosis occur at the same time?
Yes, some patients may have both insufficiency and stenosis.
Is medication enough?
In mild and moderate patients, medications are used to control symptoms but do not completely cure the disease.
When is surgical treatment needed?
If there is severe valve dysfunction and it impairs heart function, surgery is required.
Prefer valve repair or replacement?
For the mitral valve, repair is usually preferred. In the case of the aortic valve, replacement is usually performed.
Will the replacement cover last a lifetime?
Mechanical valves are long-lasting but require blood thinners. Biological caps have a lifespan of 10-15 years.
Is this disease fatal?
If left untreated, it can lead to heart failure and sudden death. Early intervention prolongs life.
Should physical activity be limited?
Depending on the degree of the disease, exercise should be done as recommended by the doctor.
Is it more common in older people?
Yes, valve degeneration is more common, especially in people over the age of 65.
Which specialist follows?
Cardiologists guide diagnosis and treatment; cardiac surgeons step in when necessary.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.