Deep vein thrombosis is a condition in which a vein deep inside the body, usually in the legs, becomes blocked by a blood clot. The most common symptoms usually occur in one leg and include swelling, pain in the calf or thigh, tenderness, an abnormally warm feeling in the skin and a red or purplish discoloration. This condition, also known colloquially as the symptoms of a thrombus in the leg, should be taken seriously. Sometimes these symptoms of thrombosis can be very mild or not present at all, causing the condition to progress silently, further increasing its importance.
| Definition | Formation of a blood clot in the deep veins of the body, usually in the legs |
| Causes | Prolonged immobility, trauma, surgical interventions, pregnancy, cancer, genetic predisposition, advanced age, obesity, hormone treatments, smoking |
| Risk Factors | Prolonged bed rest, surgery, long-term travel, family history of DVT, heart failure, varicose veins |
| Symptoms | Leg swelling, pain, increased temperature, redness, tenderness, sometimes without obvious symptoms |
| Diagnostic Methods | Doppler ultrasonography, D-dimer test, blood tests, CT-angiography |
| Treatment Methods | Anticoagulant drugs, thrombolytic therapy, compression stockings, rarely surgical intervention |
| Complications | Pulmonary embolism, postthrombotic syndrome, chronic venous insufficiency |
| Prevention Methods | Early mobilization, compression stockings, anticoagulant prophylaxis, fluid consumption, avoidance of smoking |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Deep Vein Thrombosis?
Deep Vein Thrombosis, or DVT as we often call it, is the formation of a blood clot (thrombus) in a large vein deep inside the body, usually hidden between layers of muscle.
The key word here is “deep”. This is to be distinguished from clotting in the superficial veins close to the surface of the skin, which sometimes look like a purple web and which we confuse with varicose veins. DVT is like a car accident on one of the main highways that carries blood from the legs and arms back to the heart. When this highway is blocked, the entire circulatory system is affected.
Although patients often think of DVT as a “leg problem”, it is actually a systemic circulatory issue. It is indeed most common in the legs, especially the deep veins in the calf, thigh or hip (pelvis). However, it is important to remember that in rare cases the same condition can also occur in the deep veins in the arms, in the abdomen (intestines, liver, kidneys) or in the brain. This shows us that DVT is not just a local problem in that area, but a serious circulatory disorder with the potential to threaten the whole body.
Why Deep Vein Thrombosis Should Be Taken So Seriously
The seriousness of deep vein thrombosis is actually due to its potential “dual threat”. We can think of this as two different dangers, one immediate and one long-term.
The first and most immediate threat is the risk of Pulmonary Embolism. Imagine a small piece of that insidious clot that forms in the leg vein breaking off and traveling with the bloodstream. This clot fragment usually ends up in the lungs. When it blocks one of the pulmonary arteries, this leads to Pulmonary Embolism, a life-threatening emergency. This is the third most common cause of cardiovascular death after heart attacks and strokes, and a clear indication of how grave the situation can be.
The second threat is Post-Thrombotic Syndrome (PTS), which progresses more slowly but permanently reduces quality of life. Even after the DVT attack has passed and the acute danger has been overcome, the clot can leave debris behind. It damages the delicate valves in the vein, causing a continuous pooling of blood in the leg. This turns into a lifelong problem that occurs in about half of patients with DVT and leads to chronic pain, swelling, discoloration and non-healing wounds in the leg.
This dual threat explains why DVT treatment should not only aim to save the moment, but also to protect the future. The aim of treatment is both to prevent the clot from traveling to the lung and to prevent chronic leg problems that will appear years later.
Why Does a Clot Form Inside a Vein? What Causes Deep Vein Thrombosis?
In medicine, we talk about three main factors that we call the “Virchow Triad” to explain this condition. When these three factors come together, the perfect groundwork is laid for DVT to occur. Let’s examine these factors in simpler terms:
Slowing of the Blood Flow (Medically: Stasis): Think of our veins as pipes through which a river flows. The slower the river flows, the more likely it is that sediments will settle to the bottom and accumulate. The same is true for our blood. When we are sedentary for long periods of time, blood begins to pool in our legs. Our leg muscles work like a second heart, pumping blood back to the heart against gravity. As we walk, this pump is activated. When we are inactive, this pump stops and blood flow slows down:
- Long plane or car journeys
- Bed rest after major surgery
- Paralysis
- Plaster cast on the leg
Damage to the Vascular Wall: The inner surface of our blood vessels is normally as smooth as a Teflon pan, allowing blood to flow without sticking. When damage occurs on this delicate surface, the body immediately activates the clotting mechanism to repair it. But sometimes this repair process can get out of control and turn into a large clot:
- Major surgeries (especially hip and knee replacement)
- Serious accidents and bone fractures
- Catheters inserted into a vein for intravenous serum or medication
- Some infections
Blood is more prone to clotting: In some cases, the structure of the blood itself becomes more “sticky” than normal and more prone to clotting. This condition can be both acquired and congenital:
- Cancer and some cancer treatments (chemotherapy)
- Pregnancy and the first six weeks postpartum
- Birth control pills and hormone therapies
- Smoking
- Obesity (overweight)
- Dehydration of the body (dehydration)
- Inherited (genetic) clotting disorders such as Factor V Leiden
The danger of these three factors is that when they are combined, their effects are multiplied. For example, an overweight smoker taking a long airplane trip increases the risk of DVT much more than someone with only one factor.
What are the symptoms of deep vein thrombosis and what should I look out for?
Symptoms of thrombosis in the leg often start insidiously and often occur in a single leg. Recognizing these symptoms early is vital to start treatment early and prevent serious complications. But remember that almost half of DVT patients may not show any symptoms at all. Knowing your risk factors is therefore as important as knowing the symptoms.
The most common symptoms of thrombosis are:
- Sudden onset of swelling, usually in one leg
- Pain or tenderness in the calf or thigh
- Cramp-like pain, especially when walking or standing
- The skin in the area of the clot is warmer than the other leg
- Redness, bruising or bluish discoloration of the skin
- Surface veins become more prominent
If you notice one or more of the items on this list of symptoms of a clot in the leg, you should consult a doctor instead of waiting for it to “go away”. This may be a muscle pain, but it is necessary to exclude the possibility of DVT.
What is Pulmonary Embolism and Which Symptoms Signal an Emergency?
As we have already mentioned, a Pulmonary Embolism (PE) is when a fragment of a clot in the leg travels through the bloodstream to the lungs and blocks a blood vessel there. This is the most dangerous consequence of DVT and requires immediate intervention.
If any of the following symptoms suddenly appear in addition to the symptoms in your leg, this could be a sign of a pulmonary embolism and you should call 112 or go to the nearest emergency room without waiting a second:
- Shortness of breath that starts suddenly and does not go away even at rest
- Stabbing, sharp chest pain when breathing deeply or coughing
- Sudden dizziness or fainting
- Very fast or irregular heartbeat (palpitations)
- Coughing up blood
These symptoms are the body’s emergency signals. Please take these signals seriously. It’s important to see a doctor for symptoms in the legs, but when these lung-related symptoms appear, you’re racing against time.
Life after Deep Vein Thrombosis: What is Post-Thrombotic Syndrome?
Once the acute danger of DVT has passed, the second act of the battle begins. Post-Thrombotic Syndrome (PTS) is a consequence of the permanent damage caused by DVT and can negatively affect patients’ quality of life for many years.
Think of the one-way valves in our veins like the front door of an apartment building; they only open from the outside to the inside. DVT damages these valves, preventing them from closing properly. As a result, blood constantly pools in the legs and the pressure inside the vein increases. This leads to a range of chronic complaints.
Typical signs and symptoms of PTS are as follows:
- A constant feeling of heaviness and fullness in the leg
- Chronic, persistent pain and cramps
- Swelling that increases with standing and decreases with rest
- Itching and tingling of the skin
- Brown discoloration around the ankle
- Hardening and thickening of the skin
- Painful wounds that are very difficult to heal (venous ulcers)
The most effective way to prevent PTS is to strictly adhere to treatment from the moment DVT is diagnosed, especially the regular use of compression stockings recommended by your doctor.
What Can I Do to Prevent Deep Vein Thrombosis?
Prevention is always easier and better than treatment. There are many practical steps you can take to reduce your risk of DVT. These steps can be divided into general lifestyle habits and measures for specific situations.
General Lifestyle Recommendations
Keep Moving Inactivity is DVT’s best friend. Exercise your leg muscles with activities such as regular walking, swimming and cycling.
Be Active at the Desk: If you work sitting for long periods of time, get up and walk around every hour. You can also do simple deep vein thrombosis exercises while sitting.
- Move your feet back and forth (gas-brake movement).
- Rotate your ankles in a circular motion.
- Stretch your legs straight alternately and hold for a few seconds.
Keep your weight under control: Excess weight puts extra strain on your leg veins. Try to maintain your ideal weight through healthy eating and exercise.
Drink plenty of water: Dehydration thickens the blood. Help keep your blood fluid by drinking enough water throughout the day.
Quit Smoking Smoking directly damages your vein walls. Quitting smoking is one of the most important things you can do to reduce the risk of DVT.
Special Precautions to be taken in High Risk Situations
Long Journeys When traveling by plane, car or train for more than three to four hours, it is very important to take the following precautions.
- If possible, get up every hour and walk in the corridor.
- Choose loose and comfortable clothes that are not tight.
- Avoid crossing your legs.
- Do the above-mentioned leg exercises often while sitting.
If you are in a high-risk group, consult your doctor before traveling and consider using compression stockings or taking protective medication.
Surgery and Hospitalization:
- After surgery, get up and start moving as soon as possible as soon as your doctor gives you permission.
- While in hospital, use mechanical compression devices that are attached to your legs and massage them by inflating and deflating at regular intervals.
- High-risk patients may receive a preventive dose of blood thinners to prevent DVT. Your doctor will decide on this treatment.
After Deep Vein Thrombosis (DVT) Surgery
| Recovery Time | Average 2-6 weeks; varies according to the scope of the procedure and the patient’s condition. |
| Physical Activity | Early mobilization is recommended; walking is beneficial to increase the leg muscle pump effect. |
| Medication Use | Long-term anticoagulant therapy (e.g. warfarin, rivaroxaban, apixaban) is required. INR or anti-Xa levels can be monitored during follow-up. |
| Leg Position | In the first days, the leg should be kept elevated; it is important to reduce edema and support circulation. |
| Complications | Clot recurrence, pulmonary embolism, postthrombotic syndrome (chronic leg pain, edema, wound), bleeding. |
| Wound and Catheter Site Care | Surgical incision or entry sites should be monitored for infection and kept dry and clean. |
| Compression Socks | Long-term use of compression stockings is recommended; they promote venous return and reduce the risk of postthrombotic syndrome. |
| Nutrition | If warfarin is used, vitamin K content should be balanced; a balanced and low-salt diet is generally recommended. |
| Smoking and Alcohol | Smoking should definitely be stopped and alcohol should be limited against the risk of bleeding. |
| Sexual Activity | It can usually be started after 2-4 weeks when physical recovery is achieved. |
| Psychological Support | Long-term medication use and fear of embolism can cause anxiety; support is helpful. |
| Vehicle Use | Anticoagulation and consciousness can usually be started after 1-2 weeks if appropriate. |
| Controls | Blood tests and venous doppler monitoring should be performed frequently in the first 3 months and then regularly throughout the duration of anticoagulant therapy. |
Frequently Asked Questions
What is the most important complication of deep vein thrombosis?
The most serious and dangerous complication is when the clot breaks off and travels to the lung and blocks a lung vessel. This is called “pulmonary embolism”. It can cause sudden shortness of breath, chest pain and life-threatening symptoms. Early diagnosis and treatment of DVT is vital to prevent this risk.
Is deep vein thrombosis varicose veins?
No, DVT (deep vein thrombosis) is not varicose veins. Varicose veins are enlarged and tortuous superficial veins. DVT is the formation of a clot in the deep veins. Varicose veins may be a risk factor for DVT, but there is no rule that every person with varicose veins will develop DVT.
Which doctor treats deep vein thrombosis?
In this case, the department you should consult is Cardiovascular Surgery. Diagnosis, treatment and follow-up are carried out by this branch. If necessary, ultrasound and radiologists can also help with the diagnosis.
How old does deep vein thrombosis occur?
DVT can occur at any age, but the risk increases with age and is particularly common after the age of 60. It can also occur in young people if they have risk factors such as birth control pills, genetic clotting disorders, long periods of inactivity or cancer.
What are the physical examination findings for deep vein thrombosis?
Swelling, pain, tenderness, increased discomfort when walking, redness or bruising of the skin and an increase in temperature, usually in one leg. Sometimes severe pain when squeezing the calf muscle (Homans’ sign) is also noted, but this is not always the case.
Does deep vein thrombosis heal?
Yes, with the right and timely treatment, DVT can usually be cured. Treatment prevents the clot from growing and allows the body’s own mechanisms to dissolve the clot. Blood thinners are the main treatment. Some patients may have problems such as persistent swelling and pain, called “post-thrombotic syndrome”.
How is deep vein thrombosis diagnosed?
The most reliable and commonly used method is “Color Doppler Ultrasonography”. This test directly visualizes the clot in the blood vessel. A blood test and D-dimer level can also give clues about clots, but ultrasound is essential for diagnosis.
Is aspirin used in deep vein thrombosis?
Although aspirin dilutes the blood, it is not the first choice in DVT treatment. Stronger anticoagulants (blood thinners) are used in DVT. Aspirin can only be used in special cases and on doctor’s recommendation. You should not start on your own.
Is massage performed in deep vein thrombosis?
Absolutely not! Massage can cause the clot to break off and travel to the lung (pulmonary embolism). Massage should be avoided in the leg with suspected DVT.
What are the complications of deep vein thrombosis?
The most dangerous is “pulmonary embolism”, which can even lead to sudden death. Another complication is “post-thrombotic syndrome”, which can lead to persistent swelling, pain, discoloration and sores (venous ulcers) in the leg, seriously reducing quality of life.
What happens if DVT is not treated?
Untreated DVT can lead to severe pain as the clot grows and causes severe blood flow disturbance in the leg. Worse, the clot can break off and travel to the lung, causing sudden death. In short, leaving it untreated is life-threatening.
Is deep vein thrombosis completely cured?
In most patients, with the right treatment, the vein can be restored and the clot completely removed. But sometimes the clot can stick to the blood vessel wall and cause permanent damage, leading to swelling, pain and lifelong problems in the leg.
How long does it take to treat deep vein thrombosis?
The duration of treatment depends on the individual. Generally, blood thinners are used for at least 3-6 months. If the cause of the clot or an underlying chronic disease is present, the duration of treatment may be longer. The duration is determined by your doctor at regular check-ups.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Prof. Dr. Yavuz Beşoğul » General » Heart Disease: Types, Causes, and SymptomsHeart diseases are [...]
Aug
How the Heart Works
Prof. Dr. Yavuz Beşoğul » General » How the Heart WorksThe heart functions as a [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Prof. Dr. Yavuz Beşoğul » General » How Many Hours Does Heart Valve Surgery Take?Heart [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Prof. Dr. Yavuz Beşoğul » Coronary Artery Bypass » How long does coronary artery bypass [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Prof. Dr. Yavuz Beşoğul » Kalp Kapak Hastalıkları » Kalp Kapak Değişimi Ameliyatı Nedir? Kalp [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Prof. Dr. Yavuz Beşoğul » General » Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki [...]
Aug
Life After Heart Valve Surgery
Prof. Dr. Yavuz Beşoğul » General » Life After Heart Valve SurgeryLife after heart valve [...]
Aug
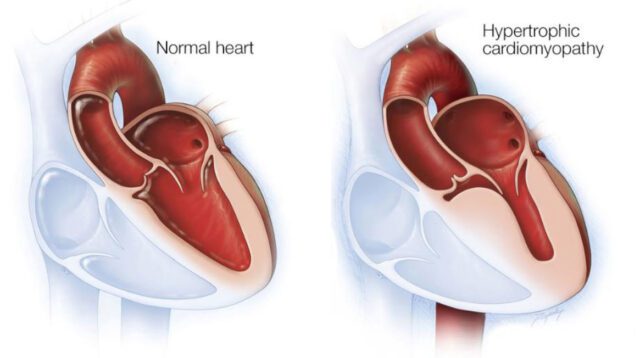
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Prof. Dr. Yavuz Beşoğul » General » Hypertrophic Cardiomyopathy: Symptoms & TreatmentHypertrophic cardiomyopathy is a [...]
Aug