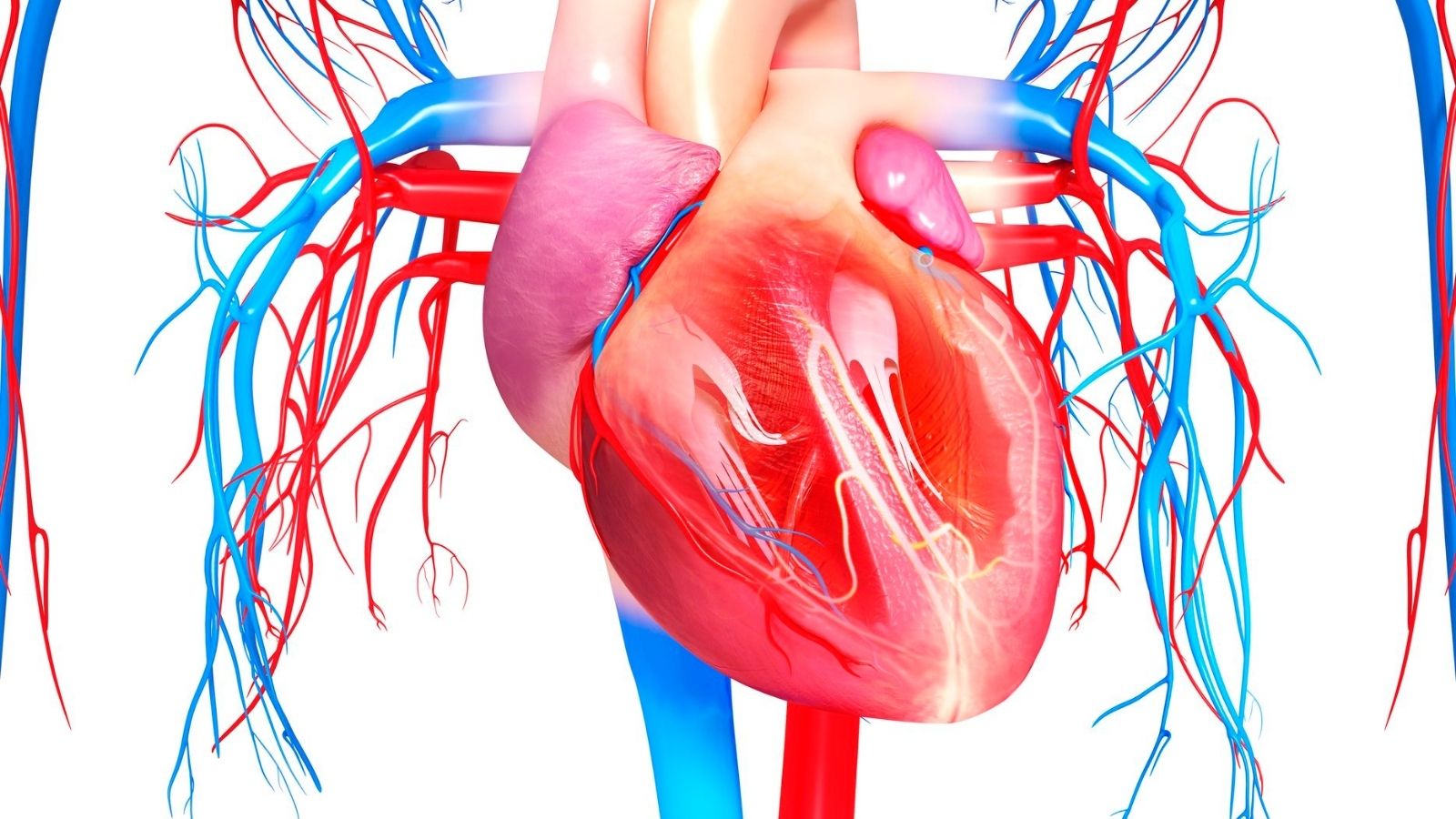
Carotid artery surgery, also known as carotid endarterectomy, is performed to prevent stroke in patients with significant carotid artery stenosis. The procedure involves removing plaque buildup to restore normal blood flow to the brain and reduce the risk of ischemic events.
Candidates for carotid surgery are typically patients with symptomatic stenosis or severe asymptomatic narrowing. Risk factors such as hypertension, diabetes, and smoking increase the likelihood of plaque accumulation, making early screening and intervention crucial.
The operation requires careful surgical technique to minimize risks such as cranial nerve injury, restenosis, or perioperative stroke. In some cases, carotid artery stenting may be considered as an alternative, particularly in high-risk surgical patients.
Postoperative care focuses on blood pressure control, antiplatelet therapy, and lifestyle modification. Long-term monitoring with ultrasound imaging helps ensure patency of the operated vessel and reduces the likelihood of future cerebrovascular events.
|
Definition |
Surgical removal of stenosis or occlusion of the carotid artery in the neck and restoration of vascular patency |
|
Indications |
Severe stenosis of the carotid artery, history of stroke or transient ischemic attack (TIA), symptomatic or asymptomatic severe stenosis |
|
Causes |
Atherosclerosis (arteriosclerosis), cholesterol accumulation, intravascular plaque formation |
|
Surgery Methods |
Carotid endarterectomy (opening the vessel to remove plaque), rarely stent placement |
|
Preparation Process |
Blood tests, ECG, carotid Doppler ultrasonography, CT or MR-angiography, anesthesia evaluation |
|
Operation Process |
Under general or local anesthesia, the vessel is accessed through a small incision in the neck, the plaque is removed and the vessel is repaired |
|
Complications |
Stroke, temporary or permanent paralysis, bleeding, infection, blood vessel blockage, nerve damage |
|
Recovery and Follow-up |
Short-term hospitalization, early mobilization, antiplatelet therapy, regular ultrasound and medical check-ups |
|
Lifestyle Tips |
Smoking cessation, healthy diet, blood pressure and cholesterol control, regular exercise, regular use of medications |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is the jugular vein that feeds our brain and why does it become narrow enough to require a jugular vein surgery?
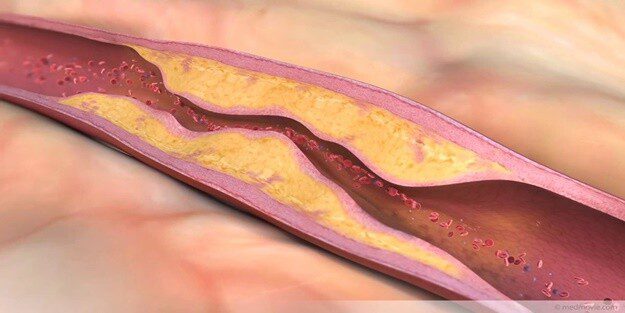
You can think of the carotid artery as a highway leading to your brain. In a healthy person, the lanes of this highway are wide and the blood flow moves quickly, without traffic. However, over the years, a process called “atherosclerosis”, commonly known as “arteriosclerosis”, gradually deteriorates this highway. Factors such as poor diet, smoking and inactivity begin to build up a sticky layer of cholesterol, fat and calcium called “plaque” on the inner wall of the arteries.
These plaques are like piles of garbage on the side of a highway. Over time, they grow, narrowing the lanes and making blood flow difficult. This is what we call carotid stenosis. This process usually goes on quietly for many years and may go unnoticed until it becomes a serious problem.
There are some important risk factors that can accelerate this narrowing and make you a candidate for Carotid Surgery. Knowing these factors is the first step in combating them. The most common risk factors are:
- High blood pressure (Hypertension)
- High cholesterol
- Diabetes (Diabetes)
- Cigarette smoking
- Obesity and overweight
- Sedentary lifestyle
- Family history of vascular disease
- Advancing age
The most frightening consequence of a stenosis of the carotid artery is a sudden lack of blood to the brain. A small piece of the narrowed and roughened plaque can break off or a clot can suddenly form in the area. This clot or piece of plaque, carried away by the blood flow, can block a thinner vessel in the brain and cause a “stroke”. Therefore, if you are diagnosed with carotid artery stenosis, it should not only be seen as a problem with a blood vessel in your neck, but as a harbinger of a vascular disease that affects your entire body.
What are the warning signs of carotid artery stenosis and how do they influence the decision for carotid artery surgery?
Although jugular vein stenosis often progresses insidiously, sometimes our body sends us small warning signals of impending danger. The most important of these signals is the “Transient Ischemic Attack” (TIA) or “mini-stroke” as it is popularly known. This occurs when blood flow to the brain is cut off for a short time and then restored. The symptoms are the same as a permanent stroke, but usually disappear completely within a few minutes or hours.
If you experience these symptoms, you should never ignore them, thinking that “my body gave a signal and it passed”. A mini-stroke is the most serious harbinger of a large, permanent stroke to come. If you experience any of these symptoms, it means you should seek urgent medical attention. Typical symptoms of a TIA attack are:
- Sudden, painless loss or blurring of vision in one eye (sensation of a curtain coming down in the eye)
- Sudden weakness in the arm or leg on one side of the body
- Numbness or downward shift on one side of the face
- Sudden difficulty in speaking, inability to find words or lisping
- Sudden difficulty in understanding what is being said
- Sudden dizziness and loss of balance
The fact that you have had a TIA or a mild stroke puts you in the group of “symptomatic” patients. This makes the decision for a Carotid Surgery much more urgent. Scientific data clearly shows that an operation performed within the first two weeks of experiencing such symptoms provides the highest benefit in preventing the risk of future permanent stroke. This is why these warning signs are the most important guideline for treatment planning.
How does my doctor suspect carotid artery stenosis and what tests are ordered before a carotid artery surgery?
Diagnosis of carotid stenosis usually starts with a simple examination. When we put the stethoscope to your neck while listening to you, we may hear an abnormal, whispering or murmur-like sound (bruit) made by blood passing through the narrowed vessel. This is an important finding that raises initial suspicion. Most of the time, however, the diagnostic process starts when you come to us with a mini-stroke (TIA) or symptoms of a stroke.
We use a series of painless and advanced imaging tests to confirm suspicion and clarify the severity of the stenosis. These tests, which draw our pre-operative roadmap, include:
- Carotid Doppler Ultrasound: This is the first and most basic step in diagnosis. Using sound waves, we take a kind of movie of your carotid arteries. With this test, we measure the structure of the vessel wall, the size of the plaque inside and, most importantly, the speed of blood flow. As a simple law of physics, the narrower a tube gets, the faster the fluid flowing through it. The high blood flow velocity we measure on ultrasound gives us very reliable information about the degree of stenosis. It is a completely painless and harmless method.
- Computed Tomography (CT) Angiography or Magnetic Resonance (MR) Angiography: If we detect a significant stenosis with ultrasound, we may order one of these advanced tests to plan surgery down to the finest detail. In these tests, a contrast agent (dye) is injected into a vein in your arm to create detailed three-dimensional maps of your carotid arteries. With these maps, we can clearly see not only the percentage of stenosis, but also the structure of the plaque (soft and rough, hard and calcareous), the tortuosity of the vessel and whether the brain is getting enough blood from other vessels (collateral circulation). This information allows us to choose the safest method of carotid artery surgery for you.
How does the severity of carotid artery stenosis affect the decision to have a carotid artery surgery?
Not all carotid stenosis requires surgery. The treatment decision is based on what percentage of the stenosis is present and whether the patient is experiencing symptoms such as a mini-stroke (symptomatic or asymptomatic). In making this decision, we weigh your risk of future stroke against the risks of the surgery itself and choose the path that is most beneficial for you.
- Surgery Decision in Symptomatic Patients: If you have recently had a mini-stroke (TIA) or mild stroke, the situation is more urgent.
- severe stenosis from p-99: In this case, surgery has been scientifically proven to reduce the risk of stroke very significantly and surgical treatment is strongly recommended.
- Moderate stenosis between p-69: Surgery may also be beneficial in this group, but the decision is individualized, taking into account additional factors such as the patient’s age and general health.
- Mild stenosis below P: Surgery has not been shown to be superior to medication for this level of stenosis and is generally not recommended.
- Decision on Surgery in Asymptomatic Patients: Even if you have no symptoms, a check-up may reveal a serious stenosis in your carotid artery. In this case, the decision is more sensitive.
- severe stenosis between `-99: In this patient group, surgery may be considered to prevent the risk of a silent stroke in the future. However, there is a critical condition here: The center and the surgeon must have a very low rate (less than 3%) of serious complications (stroke or death) related to this procedure. For this reason, it is very important that this type of surgery is performed in centers that are very experienced in this field.
What is the difference between open surgery and stenting as the main treatment methods for a carotid artery surgery?
There are two main modern proven methods to treat carotid stenosis: Traditional open surgery (Carotid Endarterectomy – CEA) and the less invasive method of stenting (Carotid Angioplasty and Stenting – CAS). Which method is right for you depends on many factors such as your age, general health and the nature of the stenosis.
- Open Surgery (Carotid Endarterectomy – CEA): This method is considered the “gold standard” in the treatment of carotid stenosis and has been used successfully for the longest time. In this surgery, we access the carotid artery directly through a small incision in the neck. We temporarily close and open the vessel and carefully scrape away the plaque layer that narrows the vessel as a whole. This is a procedure that solves the problem at its root, i.e. physically removes the plaque. After cleaning, we repair and close the vessel, usually by dilating it with a patch.
- Stenting (Carotid Angioplasty and Stenting – CAS): This is a newer and less invasive alternative. No incision is made in your neck. Instead, a thin needle is inserted through an artery, usually in the groin. With the help of thin and flexible tubes (catheters), we access the area of stenosis in your neck under X-ray. We first inflate a small balloon to widen the stenosis and then insert a special metal cage called a “stent” into the vessel to make the opening permanent. The stent crushes and stabilizes the plaque against the vessel wall, creating a wide and smooth new pathway for blood flow.
What is the new hybrid method of jugular vein surgery called Transcarotid Artery Revascularization (TCAR)?
Developed in recent years, Transcarotid Artery Revascularization (TCAR) is an innovative hybrid technique that combines the best aspects and minimizes the risks of traditional open surgery and stenting. You can think of it as a smart solution that offers the best of both worlds.
The biggest difference and advantage of the TCAR method is that it uses an ingenious protection system that reduces the risk of a clot traveling to the brain during the procedure to almost zero. Here’s how it works
- Direct and Minimal Access: Instead of traveling a long way through the groin, the carotid artery is accessed directly through a very small incision in the lower neck, just above your collarbone.
- Intelligent Blood Flow Routing: This is the key to this method. During the stenting procedure, the blood flow from the carotid artery to the brain is temporarily reversed. The blood is taken out of the body by a special system, passed through a filter to remove possible clots and plaque particles, and then returned to circulation through a vein in the leg. This prevents even the smallest particle that may form during the procedure from reaching the brain.
- Safe Stent Placement: While the brain is fully protected by this smart system, the stent is safely placed in the stenosis area.
This method avoids both the risks of large incisions and nerve damage of open surgery and the potential risks of the long catheter journey from the groin to the brain of traditional stenting. It is an excellent alternative, especially for patients considered high risk for open surgery.
What happens during a Carotid Surgery with open surgery (Carotid Endarterectomy)?
Carotid endarterectomy is a highly standardized and safe procedure that has been successfully performed for decades. The operation proceeds step by step as follows:
- Anesthesia: Depending on preference and the patient’s condition, it can be performed under general anesthesia (you are completely asleep) or local anesthesia (you are awake but your neck area is completely numbed). The advantage of local anesthesia is that we can monitor your brain function by talking to you during the operation.
- Incision A small incision is made in a natural skin fold on your neck. This makes the scar less aesthetically prominent.
- Vascular Preparation: The carotid artery is found by carefully crossing the subcutaneous tissues. Soft surgical clamps are placed above and below the vein to temporarily stop the blood flow. In some cases, a thin tube called a “shunt” is temporarily inserted into the vein to maintain blood flow.
- Plaque Removal: A small incision is made in the vessel wall and with special instruments, the plaque layer that narrows the vessel is carefully peeled off and removed as a whole.
- Repair: After the plaque is removed, the vessel wall is repaired. Usually, during this repair, a piece of synthetic material or a piece of the patient’s own vein, called a “patch”, is used to prevent the vein from narrowing again in that area. This patch closes the vein by widening it.
The operation usually takes one to three hours. If you have a stenosis in both carotid arteries that requires surgery, the procedures are usually performed in separate sessions a few weeks apart.
For which patients is a carotid artery surgery with stenting a better option?
Stenting (CAS) is not suitable for every patient, but in certain situations it can be a safer and more effective option than open surgery. Generally, we prefer this method in patients who are considered to be at higher risk than open surgery. Situations where stenting may be a better option include
- Patients with additional health problems such as serious heart or lung disease
- The stenosis is in a location that is very difficult to access surgically (e.g. very close to the skull base)
- Patients who have previously undergone another surgery in the same neck area and have severe scar tissue in that area
- Patients who have received radiotherapy (radiation therapy) to the neck area due to cancer treatment
- Patients who have previously undergone open carotid artery surgery and developed stenosis in the same vessel again (restenosis)
In these cases, stenting offers an elegant intravascular solution, avoiding a large incision and difficult surgery in scar tissue. The decision is made by a team of cardiovascular surgeons, neurologists and interventional radiologists.
What are the risks of open surgery and carotid artery surgery with stenting?
The aim of both methods is to reduce your risk of stroke and both are similarly effective in the long term. The main difference is in the short-term risk profiles during and immediately after the procedure. Large scientific studies such as CREST have clearly demonstrated these differences. We can summarize as follows: Stenting is associated with a slightly higher risk of stroke during the procedure, whereas open surgery is associated with a slightly higher risk of heart attack during the procedure.
Possible Risks After Open Carotid Surgery (CEA):
Although this surgery is quite safe, it carries potential risks like any surgical procedure. In experienced centers, these risks are very low.
- Stroke: It is the most serious risk, but the rate is as low as 1-3%.
- Heart Attack: There is a small risk due to the stress of the surgery on the body.
- Cranial Nerve Damage: This may occur due to stretching of the sensitive nerves in the surgical area. This is usually temporary and can cause symptoms such as hoarseness, difficulty swallowing or a slight asymmetry of the lips when smiling. The risk of permanent damage is very low.
- Wound Site Problems: There are risks associated with any surgery, such as bleeding (hematoma) or infection at the surgical site.
- Possible risks after carotid artery surgery with stenting (CAS):
Although less invasive, stenting also has its own risks.
- Stroke: The most important risk is that small plaque particles may travel to the brain during the advancement of catheters and stents during the procedure. Despite the protective filter systems used to minimize this risk, the risk is slightly higher than with open surgery.
- Re-stenosis (Restenosis): Re-stenosis may occur in the stented area over time.
- Intervention Site Problems: Bleeding or bruising may occur in the groin area where the catheter is inserted.
- Contrast Material Reaction: There is a risk of allergy to the dyed substance used in the procedure or adverse effects on the kidneys (especially in patients with already poor kidney function).
What is the recovery period after a carotid artery surgery and what should be considered?
Recovery after surgery is usually quite quick and comfortable. Most patients can return to their normal life in a short time.
Hospitalization: You usually only need to stay in the hospital for one or two nights. During this time, your blood pressure and neurological status will be closely monitored.
Recovery at Home:
After Open Surgery: Mild pain and tenderness at the incision site in your neck, which may last for a few weeks, is normal. This is controlled with simple painkillers.
After Stenting: There may be some mild bruising and tenderness at the incision site in the groin, which may last for a few days.
Activity Restrictions: There are some simple rules to follow for the first few weeks after surgery. These will reinforce the success of your treatment:
- Avoid heavy lifting (usually more than 5 kg).
- Avoid strenuous exercises and sudden neck movements.
- Light brisk walks will help you recover.
- You can usually start driving after 1-2 weeks, when you feel completely comfortable.
|
Type of surgery |
Carotid endarterectomy (intravascular cleaning) or carotid stenting (opening the vessel with a catheter). |
|
Recovery Time |
Recovery is usually observed within 10-15 days after endarterectomy and 1-2 weeks after stenting. |
|
Physical Activity |
Rest is recommended for the first few days, followed by a return to activity with light walking. |
|
Medication Use |
Antiplatelet drugs such as aspirin, clopidogrel; sometimes statins and antihypertensives are added. |
|
Wound Care |
The incision is usually in the neck area; the wound site should be kept dry and clean and signs of infection should be monitored. |
|
Complications |
There are risks such as stroke, transient ischemic attack (TIA), bleeding, hoarseness, difficulty swallowing, stent narrowing (restenosis). |
|
Pulse and Blood Pressure Monitoring |
Postoperative blood pressure control is very important; high blood pressure can cause bleeding and low blood pressure can affect brain perfusion. |
|
Nutrition |
A low-fat and normal salt diet suitable for cholesterol and blood pressure control is recommended. |
|
Sexual Activity |
It can usually be started after 2-3 weeks once physical fitness is achieved. |
|
Smoking and Alcohol |
Smoking and alcohol consumption should definitely be stopped; |
|
Psychological Support |
Patients who have had a stroke may have emotional lability, anxiety; support is recommended if necessary. |
|
Vehicle Use |
Driving is usually possible within 2 weeks if the person has not had a stroke. |
|
Controls |
Carotid Doppler ultrasound should be used to check vascular patency in the first month and at 6-12 month intervals thereafter. |
What should I do to prevent the vessels from narrowing again after a carotid artery surgery?
Remember, Carotid Surgery is not the end but the first step towards a healthy future. The surgery removes the critical stenosis but does not treat the underlying disease that causes atherosclerosis. This is why your lifestyle after surgery is the most important and longest-lasting part of treatment. There are two basic rules you must follow to ensure the success of the surgery and to protect your other arteries: medication and lifestyle changes.
Medication (Lifelong):
- Blood Thinners (Antiplatelet): Drugs such as aspirin prevent blood clots from forming, helping to keep both the operated vessel and the stent, if present, open.
- Cholesterol Lowering Drugs (Statins): These drugs not only lower cholesterol, but also stabilize plaques in the vessel wall, slowing the formation of new plaques. Even if your cholesterol level is normal, these drugs act as a protective shield for your vascular health.
Lifestyle Changes:
- Definitely quit smoking: This is the single most important change you can make for your vascular health.
- Eat a healthy diet: Adopt a diet rich in vegetables, fruits, whole grains and healthy fats, such as the Mediterranean diet.
- Exercise regularly: Aim for moderate exercise, such as brisk walking for at least 30 minutes most days of the week.
- Keep your weight under control: Losing excess weight eases the burden on your blood vessels.
- Check your blood pressure and sugar: Keep your high blood pressure and diabetes under strict control, if any.
Why should I be followed up in the long term after a carotid artery surgery?
Regular follow-up after surgery is critical to ensure the continued success of the treatment. This is an ongoing health partnership between you and your surgeon.
The main objectives of this follow-up are:
- To check for re-narrowing (restenosis) of the operated vessel.
- To monitor the progression of the condition in the other unoperated carotid artery.
- Make sure that your risk factors such as blood pressure and cholesterol are under control.
- Optimize your medication according to your current needs.
Our typical follow-up program starts with a check-up in the first month, 6 months and 1 year after surgery. After that, if the condition is stable, we usually check your vessels with Carotid Doppler Ultrasound once a year. Regular visits are the key to maintaining the health you have achieved with surgery and living a long, healthy life.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.