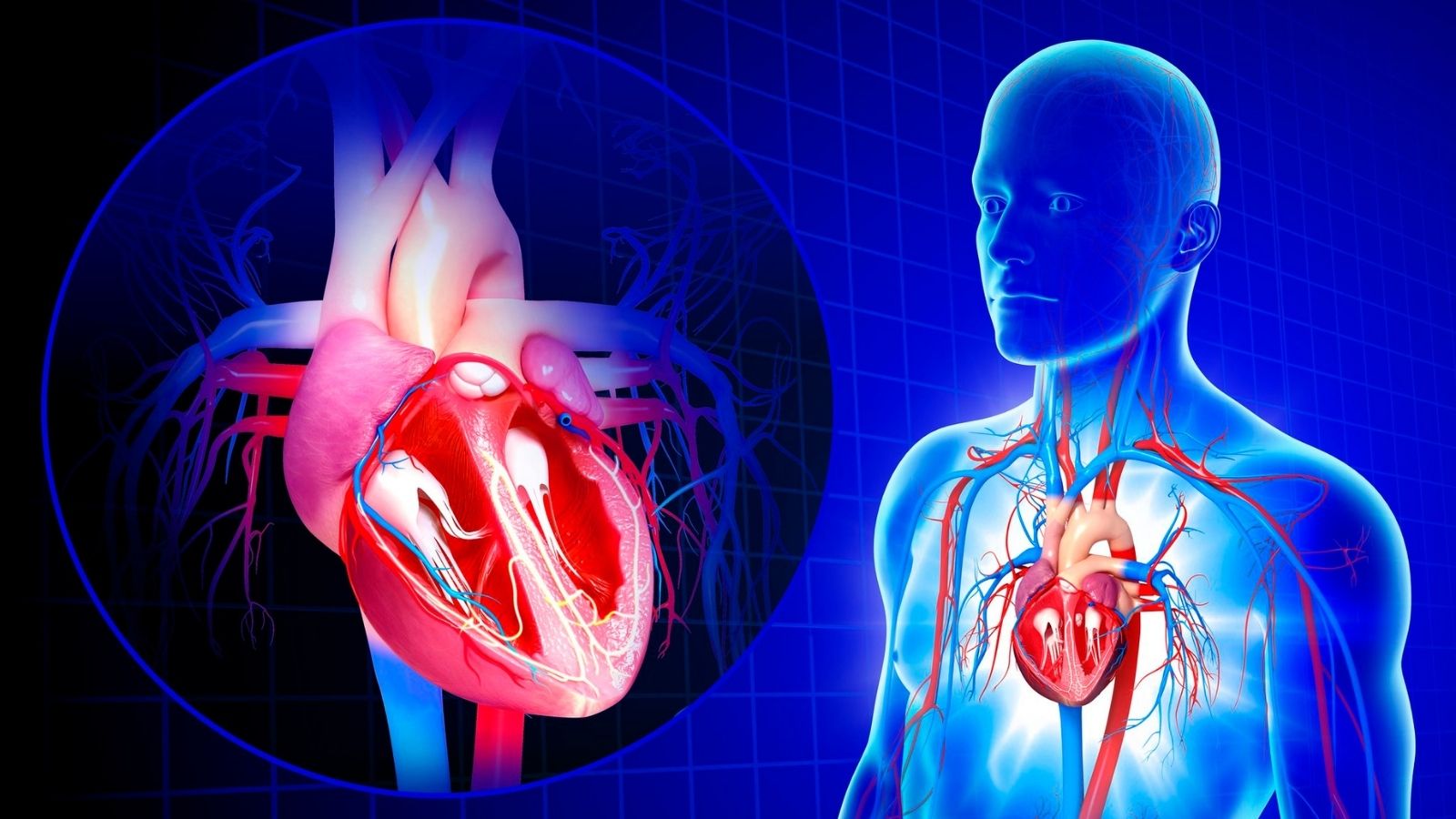
Broken heart syndrome, also called Takotsubo cardiomyopathy, is a temporary heart condition triggered by severe emotional or physical stress. It mimics heart attack symptoms such as chest pain and shortness of breath but occurs without blocked coronary arteries. Diagnosis is confirmed with imaging and cardiac tests.
The primary symptoms of broken heart syndrome include chest tightness, rapid heartbeat, dizziness, and fainting. Unlike a heart attack, patients often recover completely within weeks if properly managed. However, immediate medical attention is required to rule out life-threatening causes.
Risk factors for this syndrome are predominantly postmenopausal women, intense grief, shock, or major surgery. Stress hormones such as adrenaline are thought to weaken the heart muscle, leading to temporary dysfunction of the left ventricle.
Treatment focuses on supportive care and managing symptoms. Beta-blockers, ACE inhibitors, and stress reduction techniques are commonly used. With early diagnosis and appropriate therapy, most patients regain normal heart function without permanent damage.
| Medical Name | Tako-Tsubo Cardiomyopathy (Stress Cardiomyopathy, Broken Heart Syndrome) |
| Common Symptoms | – Sudden onset of chest pain- Shortness of breath- Palpitations- Sweating- Fainting or dizziness |
| Causes | – Sudden and intense emotional stress (loss of family, sudden bad news) – Physical stress (serious illness, surgery, trauma) – Intense fear or anger |
| Risk Factors | – Female gender (especially after menopause)- Middle and older age- Predisposition to emotional or psychological trauma |
| Complications | – Heart failure – Arrhythmias (arrhythmia) – Cardiogenic Shock – Very rare heart muscle rupture |
| Diagnostic Methods | – Electrocardiography (ECG)- Blood tests (troponin etc.)- Echocardiography- Coronary angiography- Cardiac MRI |
| Treatment Methods | – Supportive treatment (rest, stress management)- Medications for heart failure- Medications such as beta blockers, ACE inhibitors- Follow-up and monitoring |
| Prevention Methods | – Stress management techniques- Psychological support or therapy- Regular exercise- Healthy lifestyle |
What are the Symptoms of Broken Heart Syndrome?
The most frightening aspect of broken heart syndrome is that its symptoms are almost indistinguishable from a heart attack. It is therefore vital that anyone with such symptoms should immediately contact their nearest health care provider. The symptoms usually start suddenly, minutes or hours after an intense event. The main symptoms that a person with broken heart syndrome may experience are the following:
- Sudden and severe chest pain
- Shortness of breath
- Cold sweating
- Head rotation
- Nausea
- Distortion
- Fainting or feeling like fainting
Chest pain is a pressing or squeezing pain, usually felt in the center of the chest. This pain can radiate to the jaw, left arm or back, just like a heart attack. Shortness of breath occurs when the heart’s pumping function suddenly weakens, causing blood to stagnate in the lungs and can leave a person breathless even at rest. When you go to the emergency room with these symptoms, the first thing that comes to doctors’ minds is always the possibility of a heart attack and all tests are performed accordingly. The actual diagnosis of the syndrome is based on the results of these tests.
What Emotional Causes Can Trigger Broken Heart Syndrome?
The main reason why this syndrome is known as “broken heart” is that a large proportion of cases occur after an intense emotional upheaval. The way our brain perceives stress can directly affect the health of our heart. There are some traumatic emotional events that can trigger this:
- Sudden death of a loved one
- Separation from a spouse or partner
- Deception news
- A violent quarrel within the family
- Receiving a frightening medical diagnosis
- Suffering a large financial loss
- To be removed from the interior
- Witnessing an accident or having an accident
- Experiencing a natural disaster (earthquake, flood, etc.)
- Situations that cause intense anxiety, such as public speaking
Interestingly, not only negative emotions but also overly positive and exciting events can trigger this syndrome. This is called “happy heart syndrome”. For example, winning a big jackpot in the lottery or suddenly meeting a loved one you haven’t seen for years can cause a similar burst of stress hormones in the body. This shows us that the root of the problem is not so much the good or bad emotion, but the suddenness and severity of the physiological response.
Which Physical Conditions Can Lead to Broken Heart Syndrome?
Broken heart syndrome is not only triggered by emotional shocks. It can also be triggered by any physical condition that puts the body under severe stress. In fact, cases with a physical cause are often more severe and can lead to more serious complications in the hospital. There are some important physical stressors that can trigger this syndrome:
- Undergoing a major and difficult surgical operation
- Serious illnesses requiring hospitalization in intensive care
- Sepsis (infection of the blood with germs)
- Respiratory failure
- Severe asthma attack
- Acute neurological events such as stroke or brain hemorrhage
- Having an epileptic seizure
- A serious bone fracture in the body
- Excessive and unaccustomed exercise
- Some aggressive medical treatments such as chemotherapy
In such cases, broken heart syndrome is actually a complication of a serious underlying disease. When the body is already fighting a major battle, the excessive stress hormones released also affect the heart, creating this picture. The course of the syndrome, which can therefore be triggered by a physical trigger, often depends on the severity of the underlying disease.
Why is Broken Heart Syndrome More Common in Women?
When we look at cases of broken heart syndrome, we notice a striking demographic characteristic: nearly all patients are post-menopausal women. This raises the questions “why women?” and “why postmenopausal?”. Research in this area raises several important points.
One of the most powerful theories concerns the protective role of the hormone estrogen. Estrogen is found in high levels during women’s reproductive years and has many positive effects on the cardiovascular system. It increases the elasticity of the vessels, protects the inner surface of the blood vessels (endothelium) and acts as a shield against the damaging effects of stress hormones on the vessels. When estrogen levels drop dramatically with menopause, this natural protective shield disappears. This makes the heart, and especially the small vessels that feed it (microvascular circulation), more vulnerable to the damaging effects of stress hormones. So the same level of stress may not affect the heart of a pre-menopausal woman, but may trigger broken heart syndrome in a post-menopausal woman.
Another important factor is the different physiological and emotional responses of men and women to stress. Some studies suggest that women have a more intense autonomic nervous system response to sudden emotional stress. This may cause women’s bodies to release more stress hormones such as adrenaline and noradrenaline in the face of the same stressful event. This flood of hormones “locks up” receptors (receptors that are sensitive to these hormones), which are concentrated in the apex of the heart, causing the heart muscle to become temporarily dizzy (stunning).
What Tests Are Used to Diagnose Broken Heart Syndrome?
Diagnosing broken heart syndrome is like detective work. Because the first goal is to rule out a heart attack, which is much more common and requires urgent intervention. The diagnostic process is therefore based on the principle of exclusion followed by confirmation. The main diagnostic tools and tests used in this process are:
- Electrocardiogram (ECG)
- Blood tests (Cardiac enzymes)
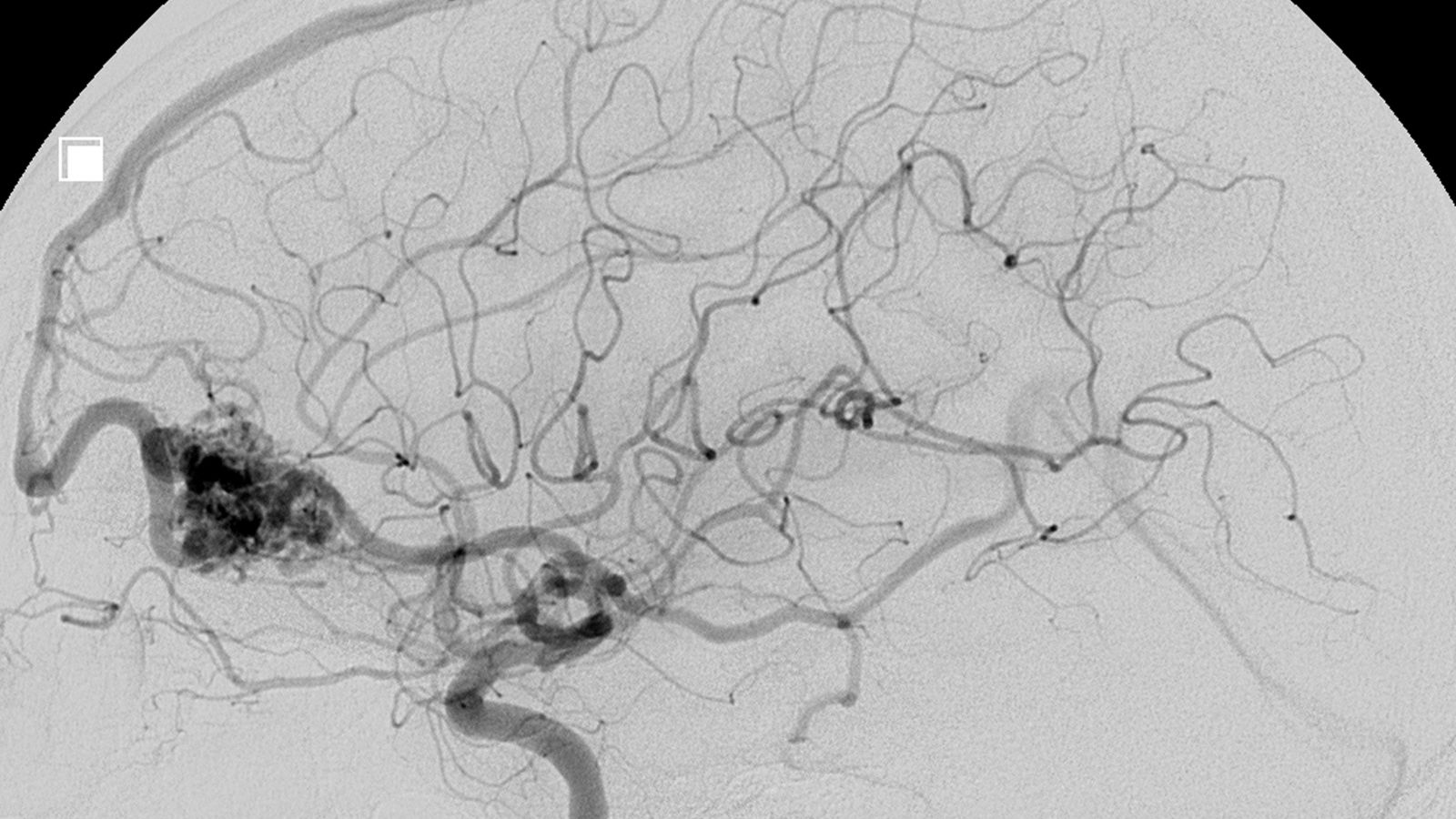
- Coronary angiography
- Left ventriculography
- Echocardiography (ECHO)
- Cardiac Magnetic Resonance (Cardiac MR)
The ECG is the first test performed in the emergency department and usually shows findings suggestive of a heart attack (such as ST elevation). This finding usually results in the patient being rushed to the angiography laboratory.
Blood tests reveal one of the most typical features of the syndrome. The enzyme troponin, which indicates heart muscle damage, is elevated, but the elevation is much milder than expected compared to the widespread dysfunction of the heart. In contrast, BNP or NT-proBNP levels, which reflect the stretching of the heart wall, rise much more than in a heart attack patient in a similar situation. This “troponin-BNP mismatch” is an important clue for the doctor.
The most critical step in diagnosis is coronary angiography. In this procedure, the vessels supplying the heart are visualized through the groin or arm. In broken heart syndrome, no significant clogging or clots are detected in these vessels, which would explain the damage to the heart muscle. The left ventriculography performed during angiography clearly shows the typical “takotsubo” image of the heart, i.e. its apex balloons and its base contracts excessively.
Once it is clear that there is no vascular congestion, the diagnosis is confirmed by echocardiography (ECHO) and Cardiac MRI. ECHO quickly shows the heart’s motility, pumping power and possible complications. Cardiac MRI gives the clearest information at the tissue level. It shows widespread edema (water retention) in the heart muscle, confirming that, unlike a heart attack, there is no permanent damage or scar tissue (Late Gadolinium Retention). These findings confirm the diagnosis and differentiate the condition from other causes such as myocarditis (inflammation of the heart muscle).
How is Broken Heart Syndrome Treatment Planned?
The treatment of broken heart syndrome is based on giving the heart time to recover and managing the dangerous complications that can arise during this process. It is not aimed at opening a blood vessel, like a standard heart attack treatment, because the problem is not in the blood vessels. Treatment is tailored to the severity of the patient’s condition.
All patients must be admitted to hospital, preferably to a coronary intensive care unit because of the risk to life. Here the heart rhythm and blood pressure are continuously monitored. The main goals of treatment are:
- Reducing the workload of the heart
- Controlling symptoms of heart failure
- Preventing and treating arrhythmias
- Prevent clot formation
- Keeping blood pressure stable
In patients with stable general condition and mild signs of heart failure (such as shortness of breath), standard heart failure medications are used. Diuretics (diuretics) to remove excess fluid from the body, vasodilators (ACE inhibitors or ARBs) to reduce the load on the heart, and beta-blockers to reduce the heart’s oxygen demand form the basis of treatment.
The most critical point is in the setting of cardiogenic shock, where the patient’s blood pressure drops dangerously low. In this situation, treatment may require a completely different approach than standard treatment of Aok, and this distinction is life-saving. Therefore, echocardiography is performed immediately in every patient in shock to look for the presence of a specific complication.
Why Is Treatment Different in the Case of Broken Heart Syndrome?
The cardiogenic shock associated with broken heart syndrome, i.e. the inability of the heart to pump blood adequately, can be caused by two different mechanisms and the treatment of the two conditions is 180 degrees opposite. The wrong treatment can worsen the condition. Therefore, it is vital to understand the cause of the shock by emergency echocardiography.
Condition: The Cause of the Shock is Pure Pump Failure.
In this condition, a large part of the left ventricle of the heart contracts so weakly that it cannot deliver enough blood to the body. This is similar to the standard picture of Asok caused by heart failure. The goal of treatment is to increase the contractile strength of the heart. Inotropic drugs such as dobutamine, dopamine or levosimendan are used to strengthen the heart’s contractility. Vasopressor drugs such as noradrenaline may also be given to support blood pressure. If necessary, mechanical assist devices such as an intra-aortic balloon pump (IABP) or Impella can be used to reduce the heart’s workload.
Condition: The Cause of Shock is Left Ventricular Outflow Obstruction (LVOTO).
This is a similar and much more dangerous scenario to ruptured heart syndrome. Here, the top of the heart balloons and does not contract, while the base contracts too strongly to compensate. This excessive contraction mechanically blocks the outflow pathway, where blood is ejected from the heart into the aorta, the main artery, with a muscle ripple. So the problem is not that the pump is weak, but that the pump’s output is faulty.
In this case, applying standard Aok treatment can be fatal. Because:
Inotropic drugs that increase the contractility of the heart (Dobutamine, etc.) are strictly prohibited. These drugs exacerbate the excessive contraction of the sole, increasing the tightness and further lowering blood pressure.
Correct treatment is aimed at relieving this mechanical obstruction:
Beta-Blockers: The cornerstone of treatment. Short-acting beta-blockers (such as esmolol) are given intravenously to slow the heart rate and the force of contraction. This curbs excessive contraction in the sole, relieving clogging.
Fluid Support: Fluids are carefully administered intravenously to increase the internal volume of the heart. This may help to widen the escape route a bit.
Pure Alpha-Agonist Vasopressors: If a drug is needed to raise blood pressure, drugs such as phenylephrine, which only constricts blood vessels without affecting the heart’s contraction, are preferred.
Does Broken Heart Syndrome Kill and How Long Does It Take to Recover?
It is now clear that broken heart syndrome, which was once considered a “benign” and “transient” condition, actually carries serious risks. Therefore, the answer to the question “does broken heart syndrome kill?” is, unfortunately, yes. In-hospital mortality rates vary between 1% and 4%, depending on the severity of the cases. This is very close to the death rate of patients who have had a heart attack. This shows how seriously the condition should be taken. In the long term, the risk of death, especially in patients triggered by a physical stressor, is comparable to that of patients who have had a similar heart attack.
However, an important point here is that the risk of death is highly dependent on the cause that triggered the syndrome. Patients who experience this syndrome after an emotional stress usually have a better long-term prognosis. In contrast, the prognosis is worse for patients who develop the syndrome while in intensive care, after major surgery or during a serious infection. Because in these cases, broken heart syndrome is a consequence of an already existing severe disease and the patient’s general state of health determines the prognosis.
But how long does recovery take? The most promising feature of the syndrome is that the damage to the heart is usually not permanent. The widespread impaired movement of the heart muscle and weakness in pumping power return completely to normal in most patients within a few weeks to a month. This improvement is clearly visible on follow-up echocardiograms.
However, a normalization of the heart’s pumping force (ejection fraction) does not always mean that the patient feels completely well. A significant proportion of patients may experience symptoms that persist months, sometimes even years, after the event. The most common of these complaints are shortness of breath on exertion, fatigue, atypical chest pains and palpitations. Further research shows that even when cardiac function is normal on paper in these patients, hidden tissue-level edema, disturbances in cardiac muscle energy metabolism and fine contractile defects may persist. This means that even if the heart has recovered from acute shock, it may not be exactly “back to normal” and this can affect the patient’s quality of life for a long time.
Does Broken Heart Syndrome Recur and What to Watch Out For in the Long Term?
One of the most common questions asked by patients who have suffered from broken heart syndrome is “will I experience it again?”. Yes, broken heart syndrome can recur, but this is not common. According to studies, the recurrence rate of the syndrome is about 1-2% per year. Over a ten-year follow-up period, it is estimated that about 5 to 10 out of every 100 patients have a second attack. A recurrent attack can be triggered by a completely different stressor than the one that triggered the first one (e.g. the first one can be an emotional stress, the second a physical stress) and affect a different part of the heart.
Having experienced this condition once requires more attention to some issues in the long term. The goal of long-term follow-up and treatment is both to maintain heart health and to minimize the risk of recurrence. There are some important points to consider in this process.
Regular Use of Drug Therapy: There is strong evidence that blood pressure medications, particularly ACE inhibitors or ARBs, both improve long-term survival and reduce the risk of recurrence. It is very important to take the medication prescribed by your doctor regularly. Although the long-term role of beta-blockers is more controversial, they may be necessary for other concomitant conditions (high blood pressure, arrhythmia, etc.).
Stress Management: Since stress is at the root of the syndrome, developing skills to cope with stress is critical:
- Receiving professional psychological support or psychotherapy
- Learn relaxation techniques such as yoga or meditation
- Regular and light exercise (with doctor’s approval)
- Getting enough and quality sleep
- Keeping social support networks (family, friends) strong
Regular Cardiology Check-ups: After discharge from hospital, a follow-up examination is usually performed in 1-3 months. At this check-up, an ECHO will confirm that the heart function has completely normalized. Afterwards, it is important to continue check-ups at intervals determined by your doctor (usually annually) in order to detect possible problems early.
Treatment of Underlying Diseases: If the syndrome is triggered by a physical illness, effective treatment of this underlying condition (cancer, chronic lung disease, etc.) is vital for both general health and heart health.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.