Peripheral artery disease (PAD) is a circulatory condition characterized by narrowed arteries, reducing blood flow to the limbs. It often presents with pain during walking and indicates systemic atherosclerosis.
Risk factors for PAD include smoking, diabetes, hypertension, and high cholesterol. Early recognition is critical, as the disease increases the risk of stroke, heart attack, and limb amputation.
Diagnosis is commonly made using the ankle-brachial index, Doppler ultrasound, or angiography. These tests assess arterial obstruction and guide treatment strategies for effective management.
Treatment of PAD combines lifestyle changes, antiplatelet therapy, and revascularization when necessary. Supervised exercise programs play a significant role in improving symptoms and functional capacity.
| Definition | Reduced blood flow due to narrowing or blockage of arteries in the arms and legs (mostly legs) |
| Causes | Atherosclerosis (arteriosclerosis), smoking, diabetes, high cholesterol, hypertension, aging |
| Risk Factors | Smoking, diabetes, advanced age, hypertension, high cholesterol, obesity, sedentary lifestyle, family history |
| Symptoms | Pain in the legs when walking (claudication), numbness, coldness, discoloration, non-healing wounds, changes in nails and hair |
| Diagnostic Methods | Doppler ultrasonography, ankle-brachial index (ABI), CT-angiography, MR-angiography, blood tests |
| Treatment Methods | Lifestyle changes, minimally invasive bypass surgery |
| Complications | Tissue death in the foot or leg (gangrene), ulcer, amputation, infection, cardiovascular events (heart attack, stroke) |
| Prevention Methods | Smoking cessation, healthy nutrition, regular exercise, blood sugar and cholesterol control, blood pressure management |
How does peripheral arterial disease occur in our blood vessels?
The underlying process at the root of peripheral arterial disease is atherosclerosis, commonly known as “arteriosclerosis”. In this process, excess fat, cholesterol and some other substances circulating in our blood adhere to the inner walls of the arteries and accumulate over time. We call these deposits “plaque”.
The body’s vascular network can be compared to a city’s plumbing system. Healthy, young arteries are like smooth, flexible, clean pipes through which blood flows freely. However, over the years, especially with the influence of certain risk factors, plaques like lime and rust deposits begin to form on the inner walls of these pipes. As the plaques grow, they gradually narrow the area through which the blood flows, that is, the inner diameter of the pipe. This narrowing leads to a reduction in the amount of oxygen and nutrient-rich blood reaching the tissues supplied by the vessel, especially the leg muscles.
When you walk or climb stairs, your muscles need more oxygen than usual. While healthy blood vessels can expand to meet this increased demand, a narrowed vessel cannot send enough blood. When the muscles don’t get the blood they need, they feel pain, cramps or fatigue. This is what we call “claudication”. If these plaques crack or form clots, the blood vessel can suddenly become completely blocked, which can lead to much more serious consequences. It should be noted that this process of atherosclerosis is a general condition that affects the whole body, not just the leg veins.
Who is more at risk for peripheral arterial disease?
There are a number of factors that increase the risk of developing peripheral arterial disease. Some of these are beyond our control, but the factors that play the main role in the development of the disease and are the most dangerous are those that are directly related to our lifestyle and that we can change.
The risk factors that we cannot control are:
- Advancing age (especially after 50 years)
- Family history of cardiovascular disease
- Male gender
- Some genetic predispositions
But much more critical are the risk factors that determine the course and severity of the disease and that we can intervene on:
- Smoking and use of all kinds of tobacco products
- Diabetes (Diabetes)
- High blood pressure (Hypertension)
- High cholesterol (Dyslipidemia)
- Obesity (Overweight)
- Sedentary lifestyle
Among these factors, there are two that are like adding fuel to the fire: Smoking and diabetes. When these two come together, their destructive effects on blood vessels increase exponentially. Smoking directly destroys the delicate layer that covers and protects the inner surface of blood vessels (the endothelium), scratching it like sandpaper. Diabetes, on the other hand, with its high blood sugar levels, hardens the vessel walls, makes them less flexible and accelerates plaque formation tremendously. The combination of these two factors in one person causes peripheral arterial disease to start at a much earlier age, to progress faster and to increase the risk of the most severe consequences, such as loss of limbs, many times over. Therefore, a diabetic smoker is in the highest risk group for this disease.
Why peripheral arterial disease should not just be seen as a leg problem
The pain you feel in your legs when you walk is actually a very important warning signal that your body sends you. This is like the “engine fault light” on the dashboard of your car. When the light comes on, you think that the problem is not only in the tires, but that there may be a serious problem under the hood, in the engine. Peripheral arterial disease is like this. The plaques that narrow your leg arteries are very likely to build up in the coronary arteries that supply your heart and the carotid arteries that take blood to your brain.
This is why a person diagnosed with peripheral arterial disease unfortunately has a much higher risk of having a heart attack or stroke than someone without this disease. The symptom in the legs is actually evidence that your entire vascular system is in danger. Heeding this warning and consulting a cardiovascular surgeon is the best step to take to protect not only your legs but also your heart and brain. The medications and methods we use in treatment are aimed at not only increasing your walking distance, but also protecting you from these life-threatening risks. This symptom is an opportunity to take action before a bigger disaster strikes.
What are the symptoms of peripheral arterial disease?
The symptoms of peripheral artery disease can vary greatly depending on the stage of the disease and the degree of stenosis. Some patients may not even feel any symptoms, especially in the early stages.
The most common and typical symptoms of the disease are:
- Leg pain with walking (claudication)
- Foot pain that does not go away even at rest
- Chills or coldness in the legs or feet
- Skin discoloration or bruising
- Skin looks radiant, taut and refined
- Loss of hair on the legs
- Slow growth and thickening of toenails
- Wounds on the toes or heel that do not heal
- In more advanced stages, blackening of the fingers (Gangrene)
- Weak or absent pulses in the legs
- Erectile dysfunction in men
The most common of these symptoms, claudication, or walking pain, is a cramp-like pain that typically occurs in the calf, thigh or buttock muscles after walking a certain distance. When the patient stops and rests for a few minutes, the pain goes away completely, but it returns at the same distance when the patient resumes walking.
When the disease progresses, “rest pain” occurs, which is a sign of a much more serious condition. This is a severe, burning pain in the toes and the front part of the foot when the patient is resting, especially when lying in bed at night. It can wake the patient from sleep. Lowering the leg off the bed can temporarily relieve the pain by allowing gravity to bring a little more blood to the foot. The presence of rest pain is a sign that the limb is in danger and requires urgent treatment.
Which department should be consulted for peripheral arterial disease and how is it diagnosed?
If you are experiencing any of the symptoms listed above, the answer to the question “which department treats peripheral arterial disease?” is clear: Cardiovascular Surgery. Specialists in this field have the necessary equipment and experience to diagnose the disease and plan the most appropriate treatment.
The diagnostic process usually starts with a detailed interview with you. After learning when and how your complaints started, your risk factors and your general health status, a comprehensive physical examination is performed. In this examination, the color, temperature and skin condition of your legs and feet are evaluated. Most importantly, your pulses are checked at different points, such as the ankle and the back of the foot. A weak or absent pulse is an important clue that something is wrong with the blood vessels.
After the physical examination, a simple, painless and highly reliable test, the Ankle-Arm Index (ABI), is measured to confirm the diagnosis. This test uses a sphygmomanometer and a small ultrasound device (Doppler) that allows us to listen to the blood flow. The ratio of the blood pressure in your ankle to the blood pressure in your arm is calculated. A ratio below 0.9 largely confirms the diagnosis of peripheral arterial disease.
Once the diagnosis is confirmed, some imaging methods are used to see the exact location, length and severity of the stenosis or blockage in order to plan treatment:
- Color Doppler Ultrasonography
- Computed Tomography (CT) Angiography
- Magnetic Resonance (MR) Angiography
- Catheter Angiography (Classical angiography)
What are the first steps in the treatment of peripheral arterial disease?
Lifestyle changes and medication are the foundation and most important part of treatment for peripheral arterial disease. Even the most successful angioplasty or surgery to open the vessels will fail in the long term if the patient does not follow these basic steps. Treatment should therefore be approached as a whole.
Lifestyle changes, which are the cornerstones of treatment, include
- Strictly quit smoking and all tobacco products
- Regular exercise (especially walking)
- Eating a healthy and balanced diet
- Getting rid of excess weight
- Learning to manage stress
Quitting smoking is the most important and single most effective step on this list. As soon as you stop smoking, the progression of the disease slows down and treatment results are much more successful. Regular walking programs are like “vascular training”. Over time, your leg, which hurts as you walk, begins to develop its own bypass pathways by forming new small vessels (collaterals) and your pain-free walking distance gradually increases.
In addition to lifestyle changes, medication is essential to slow down the underlying atherosclerotic process and reduce the risk of clots:
- Blood thinners (Aspirin, Clopidogrel etc.)
- Cholesterol-lowering drugs (Statins)
- Blood pressure regulators
- Diabetes medicines for blood sugar control
- Special medicines to reduce walking pain (Cilostazol)
These medicines are vital to protect not only your leg arteries but your whole body from risks such as heart attack and stroke. Statins, in particular, not only lower cholesterol, but also stabilize plaques in the vessel wall, preventing them from becoming more dangerous.
What are angio (closed) methods in the treatment of peripheral artery disease?
In patients who continue to have difficulty walking despite lifestyle changes and medication, or who have more serious symptoms such as rest pain or non-healing wounds, the blocked vessels need to be opened to restore blood flow. Nowadays, most of these procedures are performed with “endovascular”, i.e. closed, angioplasty methods. With these methods, the entire procedure is performed intravenously without a large surgical incision, usually by inserting a needle into the artery in the groin.
These minimally invasive treatments include:
- Balloon Angioplasty
- Stent Placement
- Atherectomy (Vascular Shaving)
Balloon angioplasty is the most basic method. After accessing the blocked area with a wire, a deflated balloon is sent through the wire. The balloon is inflated at the site of the stenosis, crushing the plaques against the vessel wall and widening the vessel lumen. In some cases, special “drug-coated balloons” are used that release medication to reduce the risk of re-contraction.
In stenting, after the vessel is dilated with a balloon, a metal cage (stent) is inserted into the vessel to make the opening permanent. This stent acts like a scaffold and prevents the vessel from shrinking again. “drug-eluting stents” are often preferred to prevent re-narrowing.
Atherectomy is a method used especially in cases where very hard, calcified and petrified plaques cannot be opened with a balloon. In this method, special devices are used to shave, scrape or shatter the plaques from inside the vessel. This cleanses the vessel wall and opens a wider pathway for blood flow. This is usually followed by a complementary balloon angioplasty.
When is surgery (open) necessary for peripheral arterial disease?
In some cases where angioplasty is unsuitable or unsuccessful, surgery, i.e. “open” surgery, may still be the best and most permanent solution. Surgical treatment is used especially when the blockage involves a very long segment, is located at the mouth of important side branches that cannot be accessed by angiography, or in patients who have already tried angiography but failed.
There are two main methods used in open surgery:
- Bypass (Bridging)
- Endarterectomy (plaque removal)
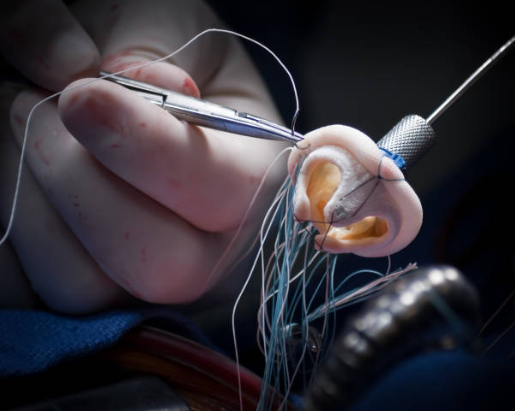
Bypass surgery is the most common surgical procedure. Just like building a new ring road around a blocked highway, a new vascular pathway is created to circulate blood flow around the blocked blood vessel. For this new pathway (graft), a vein from the patient’s own leg or an artificial vein made of synthetic material can be used. One end of the graft is sewn to the intact vein before the blockage and the other end to the intact vein after the blockage. The blood then flows over this new bridge and reaches the foot.
Endarterectomy is particularly suitable for short but dense plaques in easily accessible areas such as the groin. In this operation, the surgeon opens the vessel directly and peels off the plaque inside the vessel as a whole. The vessel is then repaired by enlarging it, usually using a patch.
Open surgery is a larger procedure than angioplasty and requires a longer recovery period. However, when performed in the right patient, it is extremely successful in saving the leg and ensuring a smooth blood flow for many years.
What is the most serious complication of peripheral artery disease?
The most advanced and dangerous stage of peripheral arterial disease is called “Critical Limb Threatening Ischemia” (CLTI). This is a condition that threatens the vitality of the limb and requires urgent intervention. At this stage, the blockage in the blood vessels is so severe that the leg or foot does not receive enough blood even at rest. This means that the tissues cannot receive nutrition and begin to die.
The most important symptoms of critical limb ischemia are:
- Rest pain (severe foot pain that occurs at night and does not go away)
- Non-healing wounds (ulcers)
- Gangrene (tissue death, blackening of the fingers)
CLTI carries a very high risk not only for the loss of the leg (amputation) but also for the patient’s life. The risk of heart attack and stroke peaks in these patients. Therefore, in the presence of any of these symptoms, it is vital to consult a cardiovascular surgeon without losing a second. The aim at this stage is to restore blood flow as quickly as possible to save both the limb and the patient’s life.
What should be the long-term expectation of an individual with peripheral arterial disease?
Peripheral arterial disease is a chronic, lifelong condition. However, this does not mean that you should despair. The prognosis depends on the steps you and your doctor take together.
If the disease is diagnosed, risk factors (especially smoking!) are controlled, medications are used regularly and, if necessary, vascularization procedures (angioplasty or surgery) are performed successfully, the progression of the disease can be slowed down significantly. In this way, patients can lead an active and long life with their quality of life intact.
It should not be forgotten that the biggest risk in this disease is not the loss of the leg, but a heart attack or stroke due to underlying arteriosclerosis. For this reason, it is essential to approach treatment holistically, with the goal of protecting the whole body, not just the legs. With the right and complete treatment, the course of the disease can be completely changed in a positive direction.
What are the most vital steps in the management and prevention of peripheral arterial disease?
The steps to prevent peripheral arterial disease and to manage it in diagnosed patients are the same and require a lifelong commitment. The patient himself or herself plays the biggest role in this process.
One of the most critical issues in this process, especially for people with diabetes, is daily foot care. Due to reduced blood flow and possible nerve damage due to diabetes (neuropathy), even the smallest wound, blister or callus on the foot may not be felt. In a foot with poor circulation, even a small wound cannot heal and can quickly become infected and turn into a dangerous ulcer or even gangrene. For this reason, daily foot care is not a simple cleaning routine but a life-saving action.
These are the foot care steps that must be applied every day:
- Examine the feet carefully every day (with the help of a mirror)
- Search for cuts, cracks, wounds, discoloration
- Wash with warm water and mild soap
- Dry gently, including between the fingers
- Moisturize the skin with a moisturizing lotion (except between the fingers)
- Wear clean and seamless cotton socks
- Choose comfortable and protective shoes that do not squeeze the foot
- Never walk barefoot
- Cut the nails straight, do not round the edges
- Never treat calluses or ingrown nails yourself
- Report even the smallest problem you notice in the foot to your doctor immediately.
Frequently Asked Questions
What is peripheral arterial disease?
Peripheral arterial disease is a circulatory disorder caused by narrowing or blockage of the arteries, usually in the legs.
Which areas does this disease affect?
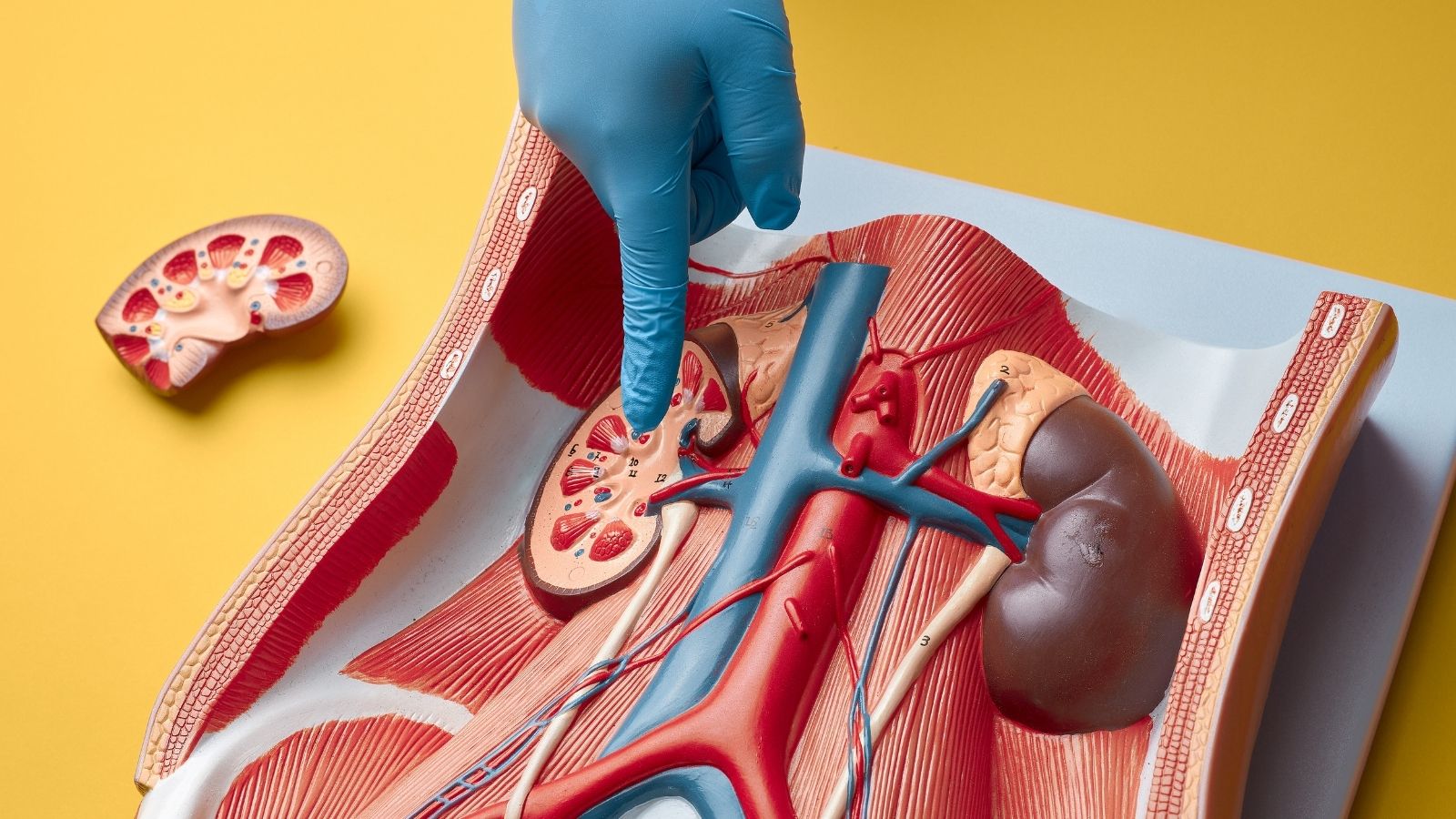
The legs are most commonly affected, but the arms, kidneys and brain vessels can also be involved.
Why does it happen?
The most common cause is atherosclerosis, the buildup of cholesterol and plaque on the vessel walls.
Who is at high risk?
The risk is increased in smokers, people with diabetes, hypertension, high cholesterol and in older people.
What are the symptoms?
Pain in the legs while walking, coldness, numbness, discoloration, late healing wounds on the feet and pain at rest in advanced cases may be observed.
How is it diagnosed?
Physical examination, pulse control, Doppler ultrasound, computed angiography and conventional angiography methods are used.
Does peripheral arterial disease affect heart health?
Yes, people with this disease also have an increased risk of heart attack and stroke because it is often part of a problem that affects the entire vascular system.
Can it be cured?
Yes. Lifestyle changes and medication can be applied in the early period, and angioplasty, stent or bypass surgery can be applied in the advanced period.
Is drug treatment enough?
It depends on the level of the disease. In mild cases, medication and a walking program may be effective; in severe cases, interventional methods may be required.
Is exercise beneficial?
Yes, walking programs in particular can support vascular reconstruction.
Is surgery always necessary?
No, surgery may be necessary depending on how long and extensive the blockage is.
What happens without treatment?
Left untreated, it can lead to serious complications such as tissue loss, gangrene and limb loss.
Which foods should be avoided?
Fatty, processed, salty and trans-fatty foods should be avoided; vegetables, fruits and whole grains should be preferred.
Will treatment be effective if smoking is not quit?
Smoking increases vasoconstriction and reduces the effectiveness of treatment. It must be stopped.
Which doctor should you consult?
Cardiovascular surgeons are authorized in the diagnosis and treatment of peripheral arterial disease.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.