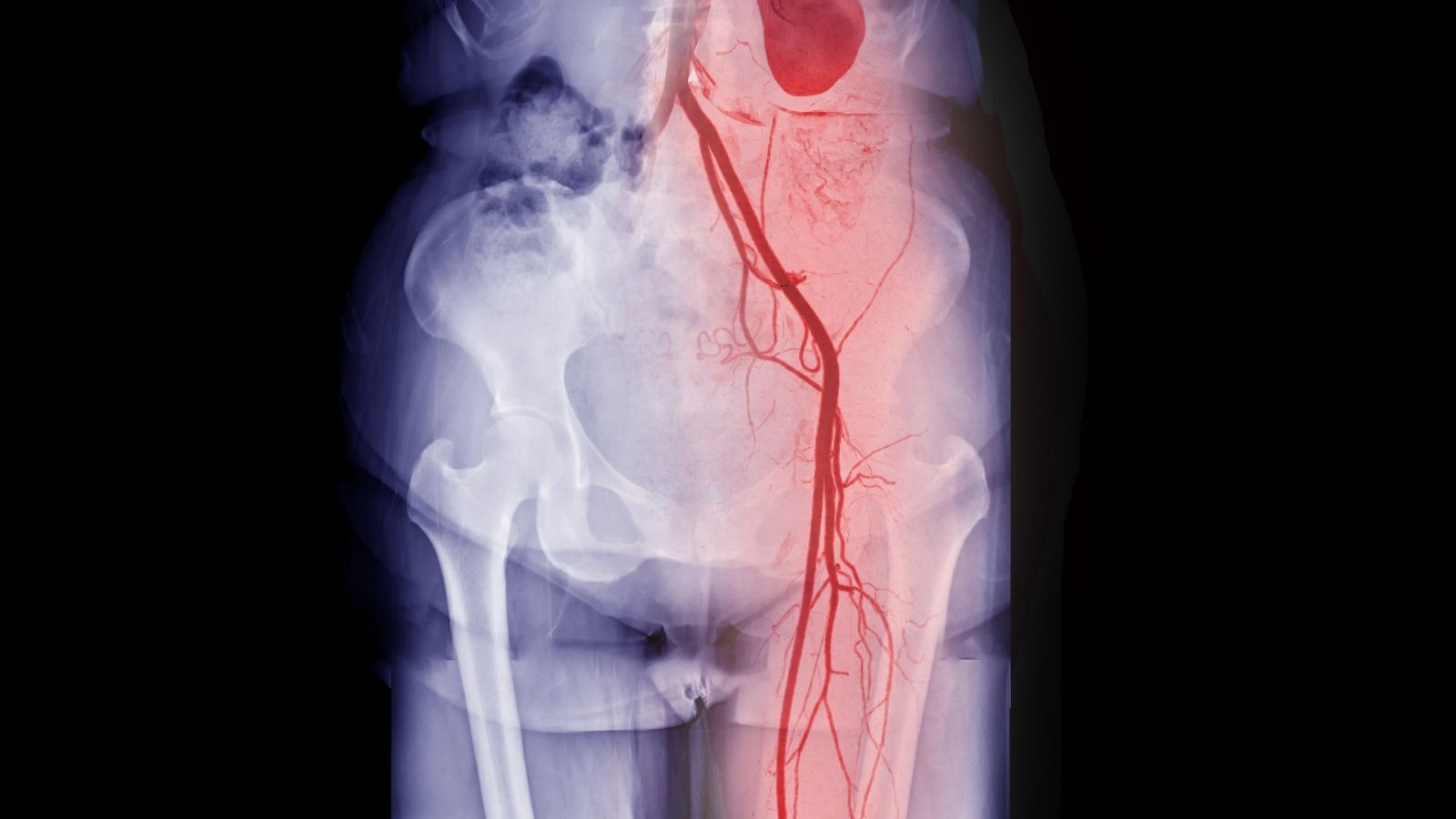
Peripheral bypass surgery is performed to restore blood flow in arteries blocked by atherosclerosis, especially in the legs. This operation improves circulation and reduces pain, preventing tissue loss and amputation.
Surgical techniques involve creating an alternative blood pathway using vein grafts or synthetic grafts. The bypass allows oxygen-rich blood to reach tissues beyond the occluded segment.
Indications for peripheral bypass include severe claudication, rest pain, non-healing ulcers, or gangrene. Without timely intervention, these complications may progress to limb-threatening ischemia.
Recovery requires strict control of cardiovascular risk factors, wound care, and rehabilitation. Long-term follow-up ensures graft patency and prevents recurrent arterial occlusion.
|
Other Names |
Peripheral Arterial Bypass, Lower Extremity Bypass Surgery |
|
Affected System |
Circulatory System (Peripheral arteries – especially leg arteries) |
|
Indications |
Peripheral arterial disease (PAD), critical limb ischemia, severe gait limitation, risk of gangrene |
|
Types of Surgery |
Femoro-popliteal bypass, femoro-distal bypass, aorto-bifemoral bypass |
|
Grafts Used |
Autogenous (patient’s own saphenous vein), synthetic grafts (PTFE, Dacron) |
|
Application Method |
A vascular graft is placed to restore blood flow from above to below the occluded artery segment |
|
Operation Process |
Under general or regional anesthesia; performed with minimally invasive surgical technique |
|
Recovery Process |
Hospital stay is usually 3-5 days; full recovery may take 10 days |
|
Common Risks |
Infection, graft occlusion, bleeding, wound healing problems, embolism |
|
Long Term Follow-up |
Regular doppler ultrasound follow-up, antiplatelet therapy, lifestyle changes |
|
Alternatives |
Endovascular treatments (balloon angioplasty, stenting), drug therapy |
|
Prognosis |
Successful results are achieved with appropriate graft selection; graft patency and relief of symptoms are aimed |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Peripheral Arterial Disease and what does it do to our body?
The arteries in our body are an enormous system of pipelines that carry oxygen-rich, clean blood pumped by our heart to all our organs, arms and legs. Peripheral arterial disease is a condition in which these life-carrying pipelines, especially those that carry blood to the legs, become narrowed and blocked over time. The main culprit behind this problem is the process of “atherosclerosis”, also known colloquially as “arteriosclerosis”. Over the years, excess fat, cholesterol and some other substances circulating in our blood adhere to the inner wall of the arteries and accumulate there. These deposits harden over time and form layers we call “plaque”. Just as limescale builds up in an old water pipe and narrows it, as these plaques grow, they narrow the blood flow path inside the artery and can eventually block it completely.
This narrowing or blockage causes the blood to not get where it needs to go in sufficient quantities. Just as the pressure of the water decreases when you step on the hose you are watering your garden with or when the hose is bent, not enough blood can get to the tissues through the narrowed vessels. This means that the tissues are deprived of oxygen and nutrients. The symptoms of the disease are actually caused by a simple imbalance of supply and demand. For example, when you start walking, your leg muscles need more energy and therefore more oxygen. Normally, the blood vessels dilate to meet this increased demand. However, narrowed vessels cannot fulfill this task. As a result, the muscles become “oxygen starved” and this manifests itself as a cramping walking pain (claudication), which is usually felt in the calf. This pain goes away when you stop and rest because the muscles’ need for oxygen is reduced. As the disease progresses, the basic needs of the tissues cannot be met even at rest. This leads to severe pain that wakes you up at night (rest pain) and eventually to non-healing wounds (ulcers) and gangrene, which is tissue death.
What classifications are used to understand the severity of the disease?
Determining how serious peripheral arterial disease is is vital both for determining the best course of treatment and for predicting the future course of the disease. For this purpose, we use certain classification systems that allow physicians around the world to speak a common language. These systems provide a clear picture of the stage of the disease.
The Fontaine classification, one of the most widely used clinical classifications, divides the disease into four main stages according to the severity of symptoms. These stages are as follows:
Stage I: Asymptomatic stage. Vascular narrowing has begun but the person does not feel any discomfort.
Stage II: Intermittent claudication (walking pain) stage. Pain, cramping or fatigue in the legs with walking or exertion, relieved by rest. This stage is divided into IIA (those who can walk more than 200 meters) and IIB (those who can walk less than 200 meters).
Stage III Resting pain stage. The person experiences severe, burning pain in the feet and fingers when lying down or resting, especially at night. This pain is usually relieved by lowering the leg off the bed.
Stage IV: Tissue loss stage. Non-healing wounds (ischemic ulcers) or gangrene (tissue death) has begun in the foot or fingers.
A more detailed system, the Rutherford classification, divides walking pain into mild, moderate and severe and defines tissue loss more precisely. Today, however, there is a need for a more comprehensive assessment of the actual risk to the leg, especially in the presence of additional problems such as diabetes.
One of the most modern systems to address this need is the WIfI (Wound, Ischemia, Foot Infection) classification. This system evaluates three key elements that together affect the fate of the leg. These critical areas assessed are:
Wound: The size, depth and extent of the wound on the leg.
Ischemia: The severity of the lack of blood supply. This is determined not only by the complaint but also by objective and sensitive measurements such as ankle-brachial pressure index (ABI) and finger pressure.
Foot Infection: Whether there is an infection in the foot and, if so, how widespread and severe it is.
Each of these three components is given a score from 0 to 3. The resulting total score gives us a much clearer picture of not only the severity of the disease, but also the risk of amputation within a year and how much the patient will benefit from treatment. So the WIfI answers the question “How much danger is this leg in?” rather than “How bad is the circulation?”.
In Which Cases Is Peripheral Bypass Surgery Necessary?
The decision for peripheral bypass surgery is made carefully for each patient and depends on the severity of the patient’s symptoms and the general condition of the leg. Not every vascular occlusion requires surgery.
Situations where surgery or a similar intervention is necessary are generally as follows:
Severe walking pain that impairs quality of life: Bypass may be an option in patients whose walking distance is very shortened (e.g. less than 50-100 meters), this situation prevents the person from doing daily chores and maintaining his/her social life, and does not improve despite medication and regular exercise programs. The aim here is to improve the patient’s quality of life.
Resting Pain: Severe pain in the leg while resting, especially at night, is a sign that the blood circulation cannot meet even the basic needs of the tissues. This situation indicates that the leg is in serious danger and requires urgent intervention.
Non-healing wounds (ulcers): The presence of wounds on the leg or foot that have not healed for months due to insufficient blood supply is an important reason for bypass surgery. It is not possible to close these wounds without opening the blood vessel and providing blood supply to the wound.
Gangrene The onset of tissue death (blackening) in the foot or fingers is the most serious condition that indicates the urgent need for blood flow to save the leg.
Sudden Leg Blockage (Acute Leg Ischemia): This is a vascular emergency when the blood vessel bringing blood to the leg is suddenly blocked by a clot. It is characterized by sudden onset of severe pain, pallor, coldness and loss of sensation in the leg. In this case, it is a race against the clock to save the leg and urgent clot removal or bypass surgery is required.
Which treatment method is right for me, surgery or angiography?
There are currently two main approaches to the treatment of peripheral artery disease: open surgery (bypass surgery) and endovascular treatment (angioplasty with balloon/stent). Which of these two methods to choose is not a simple question like “which is better?”. It is a completely personalized decision based on the patient’s age, general health condition, location, length and structure of the blockage.
Endovascular Treatment (Angioplasty, Balloon, Stent): In this method, the artery is entered through a small needle puncture, usually in the groin. Thin wires and catheters are used to access the blocked area. Here, the narrowed artery is inflated and dilated with a balloon (angioplasty) and a metal cage called a “stent” is usually inserted to prevent the artery from narrowing again.
Situations where endovascular treatment may be appropriate include
Elderly patients who are at high risk of surgery.
Those with additional health problems, such as serious heart, lung or kidney disease.
The blockage is short (usually less than 5 cm) and in a single area.
Situations where a less invasive, faster recovery process is desired.
Open Surgery (Peripheral Bypass Surgery): In this method, surgical incisions are made before and after the blocked vessel area and a new bridge vessel is created as described above.
The conditions in which bypass surgery is preferred are as follows:
Younger patients with good general health and a long life expectancy.
The blockage in the vessel covers a very long segment (e.g. 20-30 cm).
The blockage is widespread and complex in more than one area.
The vessel wall is very calcareous and not suitable for stent placement.
Previous angioplasty or stenting attempts have failed.
The main difference between the two methods is the balance between short-term comfort and long-term durability. Since angioplasty is a smaller procedure, the risk during the procedure is lower, the hospital stay is shorter and the patient can return to daily life more quickly. However, in the long term, these methods are more likely to re-clog and require re-procedure than bypass surgery. In particular, a peripheral bypass surgery using the patient’s own vein has the potential to remain open for many more years. Therefore, the decision is made with a strategic planning that will best protect the patient’s vascular health throughout his/her life. Sometimes angioplasty is the first choice, while sometimes bypass surgery, which is a more permanent solution from the start, may be the best option.
Which Vein is Used for Bypass and What are the Risks of Artificial Vein Surgery?
One of the most critical factors determining the success and longevity of bypass surgery is the type of vessel (graft) to be used as a bridge. Our options in this regard are divided into two: patient’s own vein or synthetic artificial veins.
Patient’s Own Vein (Saphenous Vein): The Gold Standard
Whenever possible, our first and best choice for bypass surgery in the infrainguinal region, i.e. the lower parts of the thigh or leg, is the saphenous vein from the patient’s own leg or arm.
Here are the reasons why the saphenous vein is the gold standard:
Living Tissue: Because it is part of the body, its inner surface is covered with living cells (endothelium) that prevent clot formation.
Long Life: Compared to all artificial veins, it stays open for many more years. This superiority is especially overwhelming in long bypasses performed below the knee in thin vessels.
Infection Resistance: Because it is the body’s own tissue, it is much more resistant to infection. Infection of a bypass vessel is a very serious problem that endangers both the leg and the patient’s life.
Flexibility: It is more resistant to bending and breaking when crossing joints (such as the knee).
Artificial Veins (Prosthetic Grafts): Alternative Solutions
In some cases, the patient’s own vein may not be usable. For example, it may have been used in a previous heart surgery (coronary bypass), its structure may have deteriorated due to varicose veins or its diameter may be too thin for bypass. In such cases, we use artificial veins made of synthetic materials.
The most commonly used types of artificial veins are:
PTFE (polytetrafluoroethylene): It is usually used in surgeries such as fem pop bypass above the knee. There are also types supported with external rings to increase its flexibility:
Dacron (Polyethylene Terephthalate): It is a fabric-like material that is mostly preferred in aortobifemoral bypass surgeries for large diameter vessels such as the main artery (aorta) in the abdomen.
The risks and disadvantages of artificial vein surgery are higher than with your own vein. The most important risks are clot blockage and infection. Since the surface of artificial veins is not alive, they are more prone to clot formation. Therefore, patients with artificial veins may need to use stronger blood thinners. They also have a higher risk of infection because they are a foreign body. When an artificial vein becomes infected, it is very difficult to treat and often requires complete removal of the vein. Therefore, the decision to use an artificial vein is only made if your own vein is unsuitable and all these potential risks are taken into account.
What is Femoral Bypass and Fem Pop Bypass and how is it performed?
The most commonly heard bypass terms are “femoral bypass” and “fem pop bypass”. In fact, they both describe a similar surgery. The answer to the question of what is femoral bypass is the general name of bypass surgeries performed to remove blockages in the “femoral artery”, the femoral artery. Fem pop bypass is the most common type of fem pop bypass.
In this surgery, the blockage is usually in the superficial femoral artery (SFA) in the middle of the thigh. We surgeons create a bridge to bypass the blood flow over this blocked area.
Starting Point (Proximal Anastomosis): We sew one end of the bridge to the healthy and high-pressure main femoral artery (CFA) in the groin area.
End Point (Distal Anastomosis): We connect the other end of the bridge to the healthy vein beyond where the blockage ends. This is usually the “popliteal artery” just above or just below the knee. The operation is therefore called “femoropopliteal” (fem-pop for short). If the connection is made above the knee, it is called “AK (Above Knee) Fem-Pop”; if it is made below the knee, it is called “BK (Below Knee) Fem-Pop”.
During the operation, these veins are accessed through incisions in the groin and knee area. If the patient’s own saphenous vein is to be used, it is usually carefully removed through an additional incision or several small incisions along the thigh. The prepared vein (graft) is then passed through a natural tunnel between the thigh muscles and the two ends are connected to the arteries with very fine sutures. Thus, blood begins to flow from the groin directly to the knee area through a new and open pathway without using the blocked pathway at all.
What are the Risks After Peripheral Bypass Surgery and What is the Recovery Process?
As with any surgical procedure, there are risks after peripheral bypass surgery. However, these risks have been minimized thanks to modern surgical techniques, anesthesia methods and intensive care facilities. It is important to know these risks in order to be prepared and to take precautions.
Possible problems that may be encountered after surgery are as follows:
General Surgery Risks: Bleeding, wound infection, lung problems (pneumonia) and anesthesia-related risks that can be seen in every major surgery.
Heart Problems: Since most people with peripheral arterial disease may also have problems with the heart vessels, there is a risk of heart attack during or after surgery. For this reason, preoperative cardiac evaluation is very meticulous.
Bypass Graft Blockage: The most important risk, especially in the first days or weeks after surgery, is the blockage of the newly inserted vessel with a clot. This can usually be caused by a technical problem, a very diseased blood vessel or the patient’s blood being too prone to clotting. When recognized early, it can usually be corrected with re-intervention.
Wound Site Problems: The wound, especially in the groin area, can sometimes take time to heal or become infected.
Leg Swelling (Edema): It is normal to have swelling in the leg in the first weeks and months after surgery due to the abundant blood supply to the leg and the lymphatic pathways being affected due to surgery, and it decreases over time.
The healing process depends on the extent of the surgery and the general condition of the patient. The hospital stay after a fem-pop bypass with an artificial vein in the leg or with your own vein is usually between 4 and 7 days. For larger operations, such as aortobifemoral bypass, this may be slightly longer. For the first few weeks after returning home, it is important to rest and keep the wound sites clean and dry. Regular short walks are encouraged to stimulate blood circulation and reduce the risk of clots. Full recovery and return to normal activities usually takes 4 to 6 weeks.
|
Recovery Time |
Average 10-15 days; depends on the type of graft, the location of the obstruction and the general health status of the patient. |
|
Physical Activity |
Early walking is recommended; it increases circulation and preserves graft patency. Heavy lifting is prohibited for the first 4 weeks. |
|
Medication Use |
Antiplatelet (aspirin, clopidogrel), statin, sometimes anticoagulant drugs should be taken regularly. |
|
Wound Care |
Surgical incisions (groin, leg, abdomen, etc.) should be kept clean; signs of infection should be monitored. |
|
Complications |
Graft occlusion, wound infection, hematoma, lymphedema, graft infection, leg discoloration. |
|
Leg Position |
Legs should be kept elevated while sitting and resting; promotes venous return. |
|
Doppler Monitoring |
Doppler ultrasound is performed at 1, 3, 6 and 12 months to monitor graft patency. |
|
Nutrition |
A heart-healthy, low-salt and balanced diet is recommended to control cholesterol and blood sugar. |
|
Smoking and Alcohol |
Smoking and alcohol should definitely be stopped as they increase the risk of graft occlusion. |
|
Sexual Activity |
It is usually possible after 10-15 days, when the physical condition improves. |
|
Psychological Support |
Support is recommended in patients at risk of amputation; compliance with lifestyle changes may be required. |
|
Vehicle Use |
It is usually possible within 2-4 weeks, once physical competence is achieved. |
|
Controls |
Vascular surgery control and imaging is recommended once a month for the first 3 months, then once every 3-6 months. |
What Can I Expect in the Long Term After Bypass Surgery?
Bypass surgery solves the problem of a blocked artery, but does not eliminate the underlying atherosclerosis. This disease is a chronic process that affects the whole body. Therefore, surgery is not the end but the beginning of a new and healthier lifestyle. In order for the surgery to be successful in the long term and to prevent further blockages in your arteries, there are some basic rules that you should follow for the rest of your life:
Here’s what you need to do for long-term success:
Never miss your medication: You should make the blood thinners (aspirin, clopidogrel, etc.) and cholesterol-lowering (statin) medications prescribed by your surgeon a part of your life. These medications will help keep your new blood vessel open and protect you from heart attack and stroke.
Absolutely Quit Smoking: Smoking is the number one enemy of arteriosclerosis and bypass blockage. No matter how successful the surgery is, if you continue to smoke, it is inevitable that both your bypass vessel and other vessels will become blocked again.
Keep Diabetes and Blood Pressure Under Control: If you have diabetes or high blood pressure, keeping these conditions under strict control is vital for your vascular health.
Eat a Healthy Diet: Adopt a diet low in saturated fats and rich in vegetables, fruits, whole grains and healthy fats, such as the Mediterranean diet.
Exercise Regularly: Regular walking, as recommended by your doctor, will improve your general health and support blood circulation in your legs.
Do not neglect your regular medical check-ups: This is one of the most important aspects. Your surgeon will call you for regular check-ups to check the condition of your bypass vessel. During these check-ups, the blood flow inside the vessel is usually evaluated with Color Doppler Ultrasound. This monitoring allows us to detect a possible narrowing early, before it leads to a complete blockage, and to correct it with a simple angioplasty procedure. This regular follow-up is the most important factor in prolonging the life of your bypass.
Pay Attention to Foot Care: Foot care is very important, especially for diabetics. Check your feet every day for possible cuts, sores, blisters or discoloration. Trim your nails carefully and wear comfortable shoes that fit your feet well. If you have even the slightest problem, contact your doctor immediately.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.