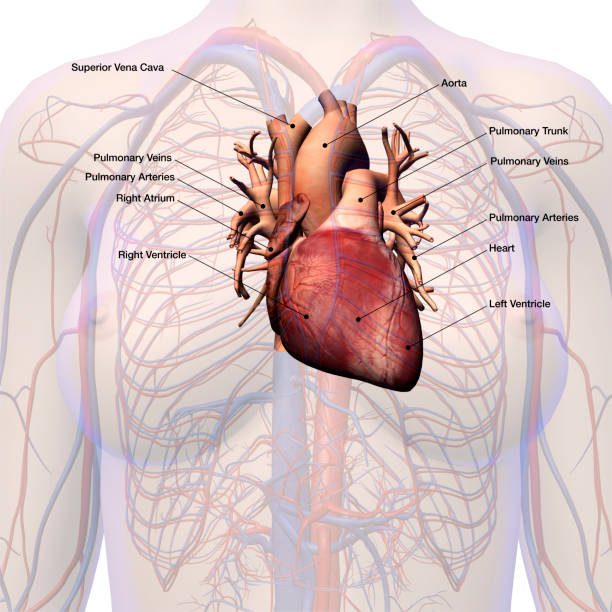
The pulmonary artery is a vital vessel that carries deoxygenated blood from the right ventricle of the heart to the lungs. Its primary role is enabling gas exchange by delivering carbon dioxide-rich blood to the pulmonary circulation.
Anatomically, the pulmonary artery branches into right and left divisions, ensuring blood distribution to both lungs. These branches further subdivide, reaching the alveoli where oxygenation occurs efficiently.
Diseases affecting the pulmonary artery include pulmonary hypertension, embolism, and congenital malformations. These conditions may impair blood flow, leading to respiratory and cardiovascular complications.
Diagnostic tools such as echocardiography, CT angiography, and catheterization help evaluate pulmonary artery disorders. Timely diagnosis and treatment significantly improve prognosis in patients with vascular or respiratory compromise.
| Anatomical Structure | Originates from the right ventricle of the heart; splits into two branches and carries deoxygenated blood to the right and left lungs |
| Physiological Function | It delivers the dirty (deoxygenated) blood returning from the body to the lungs, where it is oxygenated and returned to the left atrium |
| Associated Diseases | Pulmonary embolism, pulmonary hypertension, congenital heart disease (e.g. tetralogy of Fallot), arteriovenous malformations |
| Diagnostic Methods | CT pulmonary angiography, echocardiography, cardiac catheterization, chest x-ray, MRI, D-dimer |
| Surgical Interventions | Pulmonary endarterectomy (in chronic thromboembolic hypertension), arterial reconstruction (in congenital defects) |
| Complications | Right heart failure, hypoxemia, sudden cardiac death (especially in embolism), pulmonary edema |
| Clinical Significance | Essential vessel for gas exchange in the lungs; assessed as an indicator of right heart function |
What Does the Pulmonary Artery Do in Our Body?
We can think of the function of the pulmonary artery as the main pipeline to a treatment plant. All cells in the body use oxygen to produce energy and in the process produce carbon dioxide as waste. This carbon dioxide-laden, oxygen-depleted blood needs to be cleaned as soon as possible. This is where the pulmonary artery comes into play.
This small but vital cycle in the circulatory system works step by step as follows: Contaminated blood flows through the large veins into the right atrium of the heart. From there it passes into the right ventricle. Each time the heart beats, the right ventricle pumps this blood with a strong contraction through the pulmonary valve and directly into the main pulmonary artery.
After a short journey, this main artery splits into two, like the trunk of a tree splits into main branches, going to the right and left lung. These branches, which enter the lungs, gradually become thinner and thinner, eventually wrapping like a spider web around the millions of tiny air sacs we call alveoli. When we breathe in, these air sacs are filled with oxygen. As the blood passes through the walls of these sacs, it expels the carbon dioxide it carries and binds fresh oxygen to itself. This blood, now cleaned and filled with oxygen, returns to the left side of the heart through the pulmonary veins (lung veins) and from there is distributed throughout the body via the aorta. This cycle goes on endlessly and is the basis of life.
What is the Anatomical Structure of the Pulmonary Artery?
The pulmonary artery is located in the middle of our rib cage, above the heart, in very close proximity to the aorta, the main artery of the body. Its structure is designed to be perfectly suited to the specific task it undertakes.
Main Pulmonary Artery (Pulmonary Trunk): This main artery originates from the right ventricle of the heart and has a fairly wide beginning. It is about 5 centimeters long and about 3 centimeters in diameter. This width allows the heart to comfortably accept a large volume of blood with each contraction.
Right and Left Pulmonary Arteries: The main trunk divides into two main branches that pass behind the aorta and go to the right and left lung. The branch to the right lung is usually slightly longer than the one to the left.
Branching: Once inside the lungs, these main branches branch continuously, parallel to the lobe and segment structures of the lungs. Thanks to this dense branching, blood can reach the smallest air sacs where gas exchange takes place.
Wall Structure: Like other arteries, it consists of three layers. However, there is one important difference that distinguishes it from the aorta. The aorta has to withstand a very high pressure to deliver the blood pumped from the left side of the heart throughout the body, which is why its walls are thicker and more muscular. The pulmonary artery, on the other hand, carries blood only to the adjacent lungs, a much shorter distance and at a lower pressure, so its walls are thinner and more flexible. This structure is an excellent adaptation that prevents unnecessary strain on the right heart.
What is the Difference Between Pulmonary Artery and Pulmonary Vein?
Although the names of these two vessels are similar, their functions are completely opposite and understanding this distinction is crucial to grasping the logic of the circulatory system. Both have the word “pulmonary” in their names, indicating that they are related to the lungs. The main differences are:
Pulmonary Artery It carries low oxygen (“dirty”) blood from the heart to the lungs.
Pulmonary vein It carries oxygen-rich (“clean”) blood from the lungs to the heart.
The simple rule to remember is this: Arteries take blood away from the heart and veins (veins) bring it to the heart. Whether the blood they carry is clean or dirty depends on where it is going or coming from. This exceptional situation in the pulmonary circulation is due to the original purpose of the system, namely to purify the blood.
Which diseases can affect the pulmonary artery?
Unfortunately, this vital vessel and its branches can be affected by certain diseases. These diseases put a serious strain directly on the right side of the heart by making blood flow difficult and can have dangerous consequences over time. The most common situations are the following.
Pulmonary Hypertension: This is a condition in which the blood pressure in the arteries of the lungs is much higher than normal. Over time, this can cause the arteries to harden, narrow and become blocked. The right side of the heart has to constantly exert more and more force to move blood through this narrowed pathway. This can be compared to the fatigue of a car engine when it tries to drive up a hill by constantly upshifting gears. Over time, the right heart enlarges and begins to lose function, leading to right heart failure.
Pulmonary Embolism: This is when a blood clot, which usually forms in the veins in the legs, breaks loose and travels through the bloodstream to the lungs, where it blocks an artery. This is a life-threatening condition that develops suddenly and requires urgent medical intervention. Depending on the size of the blocked blood vessel, it can cause sudden onset of shortness of breath, sharp chest pain or even fainting.
Congenital Structural Problems: Some babies may be born with heart defects that directly affect the pulmonary artery. Some of these defects include:
- Pulmonary Stenosis (Stenosis)
- Pulmonary Atresia (no development of the valve)
- Transposition of the great arteries (replacement with the aorta)
- Truncus Arteriosus (emerging as a single vessel with the aorta)
- Tetralogy of Fallot (a complex combination of four different heart defects)
Pulmonary Artery Enlargement (Aneurysm): This is a weakening and ballooning of an area of the pulmonary artery wall. It is a rare condition that usually develops due to underlying causes such as long-term pulmonary hypertension or certain connective tissue diseases. Pulmonary artery dilatation is most dangerous because of the risk of rupture, which can lead to sudden and fatal internal bleeding.
How to Suspect Pulmonary Artery Disease in a Person
Unfortunately, the symptoms of pulmonary artery disease can often be easily confused with other conditions. Therefore, early diagnosis is sometimes difficult. Nevertheless, it is important to consult a specialist, especially when several symptoms come together. Here are some common symptoms to look out for:
- Shortness of breath, which increases especially during exertion and is felt even at rest over time
- Unexplained, persistent fatigue and weakness
- Pain or pressure in the chest, especially when breathing deeply or coughing
- Attacks of dizziness or fainting
- Heartbeat acceleration or irregularity (palpitations)
- Swelling in the ankles, legs and eventually in the abdomen (edema)
- Bluish or purplish discoloration of the lips and nails (cyanosis)
- Rarely, coughing up blood (hemoptysis)
If you experience any of these symptoms, especially more than one, you should not take it lightly and should consult a cardiologist or cardiovascular surgeon.
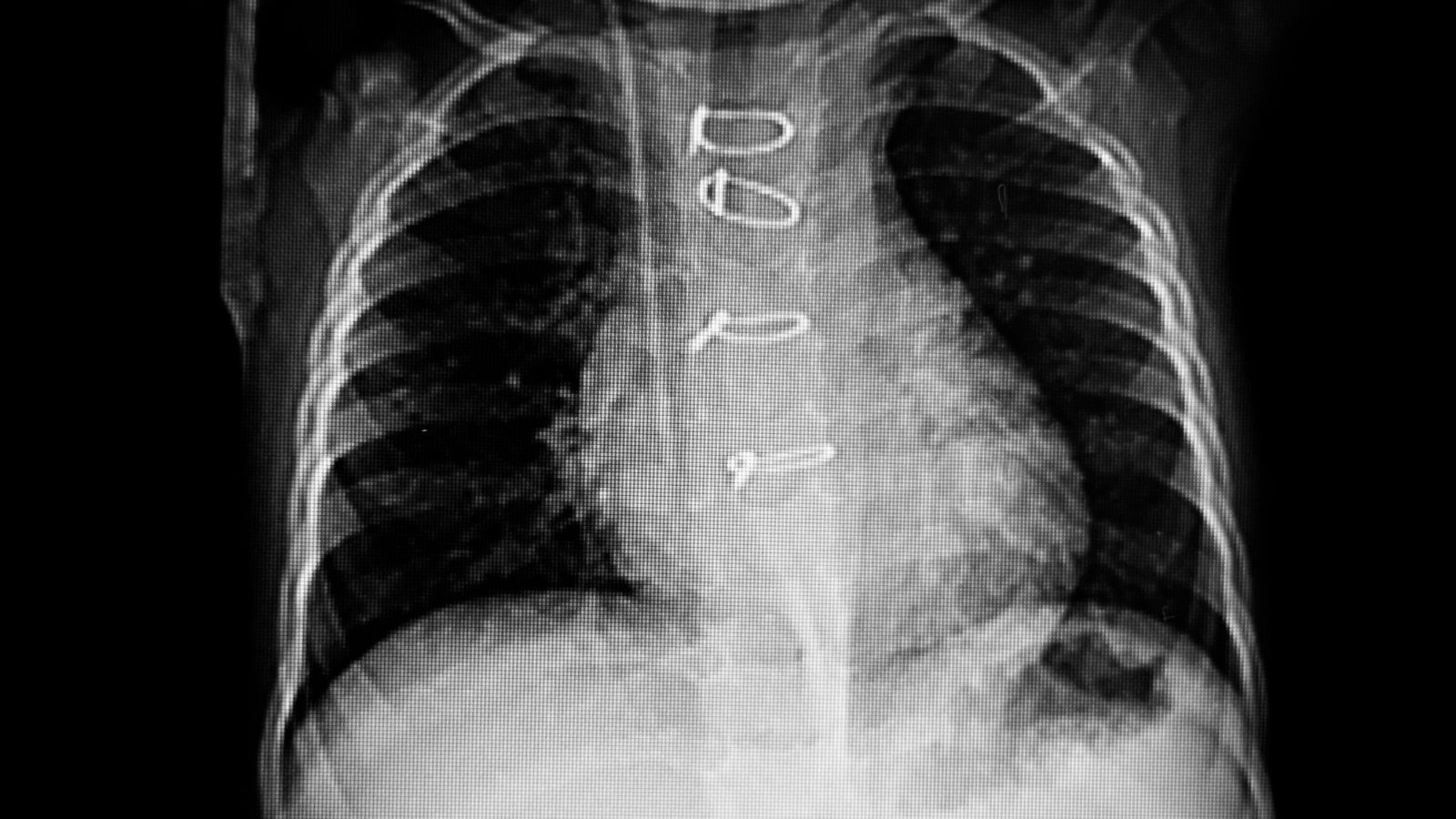
How is Pulmonary Artery Disease Diagnosed?
Reaching the correct diagnosis requires gathering clues like a detective. After listening to the patient’s complaints and performing a physical examination, various tests are used to confirm the diagnosis and understand the severity of the disease. These tests complement each other to give us a clear picture of the condition of the blood vessels and heart.
The main diagnostic methods we use are:
Echocardiography (Heart Ultrasound – ECHO): This is usually our first step. Using sound waves, we obtain moving images of the heart. With this test we can see the size of the heart chambers, how well the valves work and the strength of the heart’s contraction. Most importantly, it gives us valuable preliminary information about the pressures on the right side of the heart and reinforces the suspicion of pulmonary hypertension.
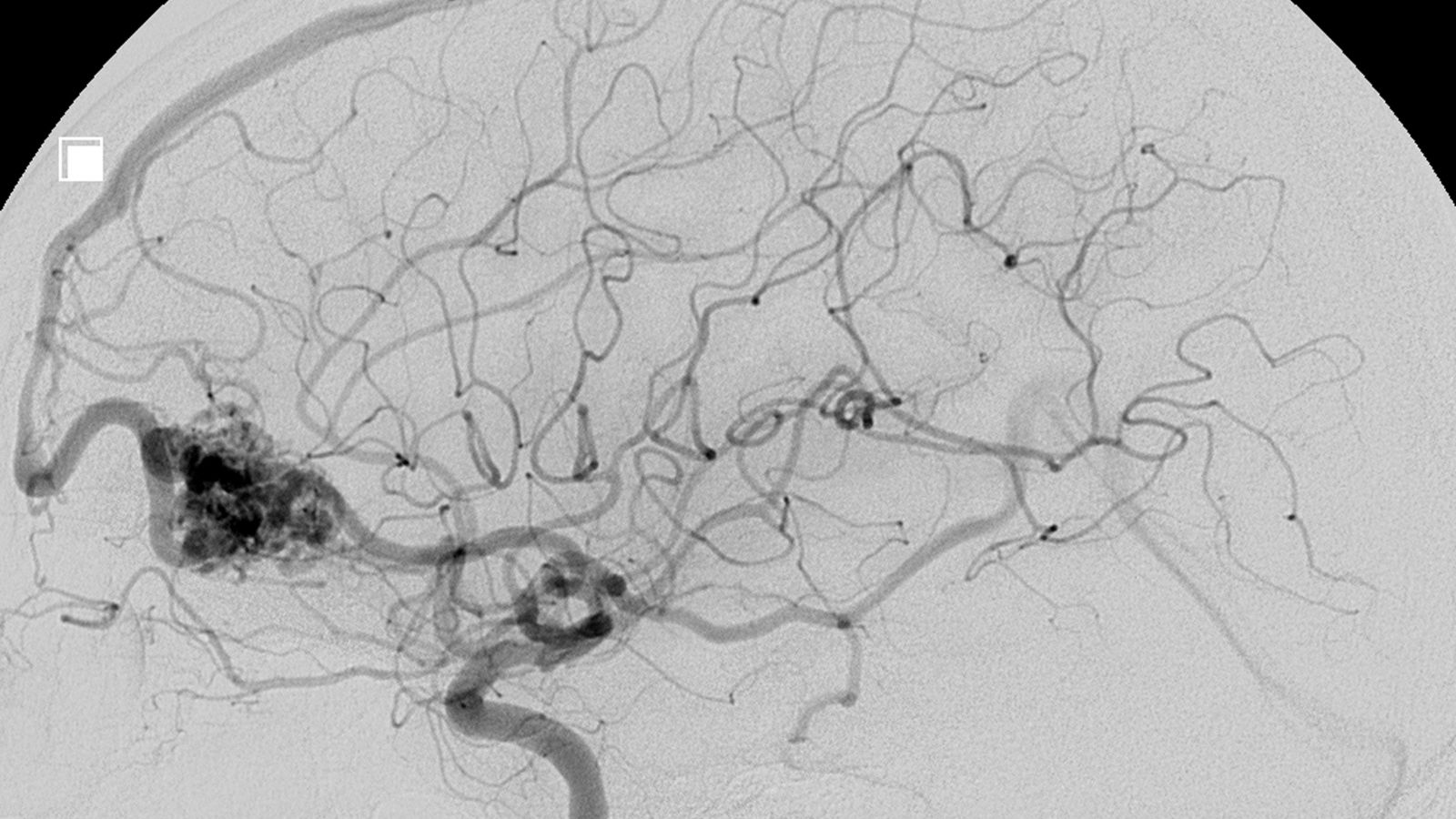
Computed Tomography (CT) Pulmonary Angiography: It is the gold standard especially in suspected pulmonary embolism. It is performed with an intravenous dye (contrast dye) that makes the vessels visible. It shows the inside of the pulmonary arteries like a road map, allowing us to clearly detect clots, stenosis or aneurysms such as pulmonary artery dilatation.
Right Heart Catheterization: This is the most reliable way to confirm the diagnosis of pulmonary hypertension and to measure pressures millimetrically. Under local anesthesia, a very thin catheter is inserted through a vein in the groin or neck to access the right side of the heart and from there the pulmonary artery. In this way, the actual pressure values inside the vessel are measured and the treatment plan is shaped according to these precise results.
Ventilation/Perfusion (V/Q) Scintigraphy: A nuclear medicine test that shows how well the lungs are ventilated (ventilation) and blooded (perfusion). It is used for the diagnosis of pulmonary embolism, especially when CT angiography cannot be performed.
Electrocardiogram (ECG): Records the electrical activity of the heart. It may show signs that the right side of the heart is strained.
Blood Tests: It is used to check oxygen levels in the blood, clotting tendency (such as D-dimer) or markers that indicate that the heart muscle is under strain.
6 Minute Walk Test: It is a simple but very useful test to understand the functional capacity of the patient, i.e. how much effort they can exert.
What are the Treatment Options for Pulmonary Artery Disease?
The treatment plan is completely individualized according to the type and stage of the disease and the individual characteristics of the patient. Modern medicine has made significant advances in this area in recent years and many treatment options are now available.
Treatment can be categorized under three main headings:
Drug Treatments:
Medicines are the cornerstone of the treatment of many pulmonary artery diseases.
Pulmonary Vasodilators: They are used especially in the treatment of pulmonary hypertension. By relaxing and widening the narrowed pulmonary arteries, these medicines improve blood flow and reduce the burden on the heart.
Anticoagulants (blood thinners): They are vital in the treatment of pulmonary embolism and in preventing the formation of new clots.
Diuretics (Diuretics): By removing excess fluid accumulated in the body, they reduce the volume of blood the heart has to pump and provide relief, especially in patients with edema.
Digoxin: It may help to regulate the heartbeat and slightly increase the contractile force of the heart.
Interventional and Surgical Treatments:
These methods are used when drug treatment is inadequate or when the nature of the disease requires surgery.
Pulmonary Thromboendarterectomy (PTE): This is a very specialized open-heart surgery for pulmonary hypertension caused by chronic (persistent) pulmonary embolism (CTEPH). The operation peels away the layers of old, organized clots that line the inside of the arteries like a lining. A successful PTE surgery has the potential to restore the patient to full health.
Balloon Pulmonary Angioplasty (BPA): This is a catheter-based procedure for CTEPH patients who are not suitable for PTE surgery or who are at very high risk of surgery. Through angiography, the narrowed vessels are accessed and widened with a balloon.
Repair of Congenital Defects: Conditions such as pulmonary stenosis can be treated without surgery by balloon dilation. However, more complex problems, such as Tetralogy of Fallot or Pulmonary Atresia, are usually corrected by open heart surgery in infancy or childhood.
Lung or Heart-Lung Transplant: It is a treatment option considered as a last resort in cases where all other treatment methods have failed and the disease has reached the last stage.
Lifestyle Changes and Supportive Therapies:
They are important steps that directly affect the success of medical treatments and improve quality of life:
- Salt restriction
- Complete smoking cessation
- Regular exercise as permitted by the doctor (e.g. walking)
- Maintaining ideal weight
- Regular flu and pneumonia vaccinations
- Oxygen therapy if necessary
- Stress management and psychological support
Remember that treatment is a team effort. The best results are achieved when the patient, family and doctor work in harmony.
Frequently Asked Questions
What is the pulmonary artery?
The pulmonary artery is the main artery that comes from the right ventricle of the heart and carries deoxygenated blood to the lungs.
What is the function of the pulmonary artery?
It delivers oxygen-poor blood to the lungs where it is oxygenated. This process is vital.
Where is the pulmonary artery located?
It leaves the right ventricle of the heart, travels a short distance and divides into the right and left lungs.
Why does the pulmonary artery carry deoxygenated blood?
Unlike other arteries, the pulmonary artery carries blood that leaves the heart but is not oxygenated. In this respect, it is an exception.
What is the difference between a pulmonary artery and a vein?
The pulmonary artery carries deoxygenated blood, while the pulmonary vein brings oxygenated blood back to the left atrium of the heart.
What happens if the pulmonary artery narrows?
This condition is called “pulmonary stenosis”. The lungs do not get enough blood and the heart has to work harder.
How does pulmonary embolism affect the pulmonary artery?
It is a condition in which this blood vessel to the lung is blocked and can lead to sudden shortness of breath, chest pain and life-threatening consequences.
What does pulmonary hypertension mean?
Blood pressure in the pulmonary artery is higher than normal. Over time, it can seriously affect heart health.
Who has pulmonary artery disease?
It is more common in people with heart disease, long-term lung diseases and coagulation disorders.
How is pulmonary artery occlusion diagnosed?
Diagnosis is made by methods such as computed tomography (CT), echocardiography and pulmonary angiography.
Do pulmonary artery problems disrupt heart rhythm?
Yes, increased pulmonary pressure can affect the right side of the heart, leading to rhythm disturbances.
Is pulmonary artery a congenital disease?
Yes, some babies may have stenosis, obstruction or localization anomalies of the pulmonary artery.
What are the treatment methods?
Depending on the underlying cause, medication, balloon angioplasty, stenting or open heart surgery may be required.
Are pulmonary artery problems fatal?
Left untreated, pulmonary embolism or pulmonary hypertension in particular can be life-threatening.
Which specialty deals with these vascular diseases?
Cardiology, pulmonology and cardiovascular surgery departments evaluate together.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.