Raynaud’s syndrome is a circulatory disorder triggered by conditions such as cold weather or stress, leading to vasoconstriction in extremities such as the hands and feet. Also known as Raynaud’s phenomenon, it can occur as a primary (Raynaud’s disease) or secondary condition. The most common symptoms of Raynaud’s phenomenon are sudden pallor, often of the hands, followed by bruising and redness. Raynaud’s disease or phenomenon can negatively affect patients’ daily life due to bruising and swelling of the hands.
The Raynaud’s phenomenon test is used to diagnose this condition, while the stages of Raynaud’s phenomenon are assessed to determine the severity and duration of symptoms. Complaints of Raynaud’s phenomenon are usually based on the frequency and severity of the attacks that people experience. Raynaud’s syndrome can also occur in the area of the foot and the veins in this area can also be affected.
The causes of Raynaud’s disease are unknown, but genetic predisposition, stress and connective tissue diseases may play a role. in answer to the question “Is Raynaud’s disease fatal?”: it is not directly fatal, but secondary forms may be associated with serious diseases. The treatment of Raynaud’s phenomenon is a complete surgical sympathectomy. Reviews of Raynaud’s patients who have used vasodilator drugs are unfortunately that they did not benefit.
| Category | Information |
| Other Names | Raynaud’s Disease (Primary), Raynaud’s Syndrome (Secondary) |
| Affected System | Circulatory System, Peripheral Vessels (especially hands) |
| Causes | It is particularly common in young women but can also occur in men. It is common in people with a highly active sympathetic nervous system. Connective tissue diseases such as scleroderma may also be seen. The result of spasm of the small arteries in the hands under stress. |
| Risk Factors | Cold weather, stress, female gender, connective tissue diseases (e.g. scleroderma, lupus) |
| Symptoms | Whitening, bruising, reddening of the fingers (hands and feet); tingling, numbness, pain, wounds on the fingers in advanced stages and infection. |
| Diagnostic Methods | Clinical history and physical examination, cold and hot water tests |
| Complications | Finger ulcers, skin changes, rarely tissue death |
| Treatment Methods | The only treatment is surgical sympathectomy. |
| Prevention | Avoiding cold environments, quitting smoking, reducing stress |
| Frequency of Appearance | Common; more common in young women |
| Prognosis | Complete recovery occurs after successful surgical treatment. |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Raynaud’s Disease?
To better understand Raynaud’s disease, let’s take a look at the normal functioning of the body. When our body encounters cold, it activates a defense mechanism to keep our vital organs warm. It slightly constricts the blood vessels close to the skin, especially at the extremities such as the hands and feet, and redirects blood to more central parts of the body. This is a completely normal and life-saving reflex.
In Raynaud’s patients, however, this reflex “goes out of control”. The vessels contract much more violently and suddenly than they should. This excessive contraction (in medical terms, vasospasm) almost completely stops the blood flow to the area. This is the main difference that distinguishes Raynaud’s disease from the ordinary sensation of a cold. The condition is named after Dr. Maurice Raynaud, the French physician who first described it in the 19th century, and contrary to popular belief, it is quite common in the community. Knowing this is often comforting for newly diagnosed people, as they realize that they are not alone in this journey.
What are the Types of Raynaud’s Disease?
There is no single type of Raynaud’s disease and the most important factor determining the treatment approach is to decide which type it is. It is basically divided into two main groups: Primary and Secondary. Knowing the difference between the two is vital both to understand the course of the disease and to chart the correct course of treatment.
Primary Raynaud’s (Raynaud’s Disease): This is the most common and usually more “innocent” form of the condition. Primary Raynaud’s occurs on its own, without any other underlying disease. The cause is unknown, but it usually starts in young women between 15 and 30 years of age and may have a familial predisposition. Symptoms are often mild and usually do not cause serious problems, such as sore fingers. In some cases, it may even resolve on its own over time.
Secondary Raynaud’s (Raynaud’s Phenomenon): This form, as the name suggests, occurs as a “consequence” of another health problem. It usually begins after the age of 40 and tends to be more severe than the primary form. The underlying cause is usually a connective tissue disease, a vascular disorder or a medication. In secondary Raynaud’s, there is a higher risk of tissue damage such as painful sores on the tips of the fingers (digital ulcers) and, rarely, gangrene. Therefore, when Raynaud’s phenomenon is detected in a person, it should be considered as a “symptom” and the underlying cause should be thoroughly investigated.
Here are some key points to get a clearer picture of the main differences between the two types:
- Absence of underlying disease (Primary)
- Dependence on another disease (Secondary)
- Onset usually between 15-30 years of age (Primary)
- Onset usually after 40 years of age (Secondary)
- Mild and manageable symptoms (Primary)
- More severe symptoms and risk of complications (Secondary)
- Very low risk of tissue damage (Primary)
- Higher risk of ulcers on the fingers (Secondary)
What are the Symptoms of Raynaud’s Disease and What Triggers Attacks?
The symptoms of Raynaud’s disease usually appear in periods called “attacks”, which are triggered by specific triggers. What happens during these attacks is quite characteristic. Most patients describe that the attack typically progresses with a gradual discoloration.
Color changes during an attack usually follow this sequence:
- White (Pallor)
- Blue (Bruising)
- Red (Redness)
First, when the veins contract, the blood supply is cut off and the fingers take on a white, almost “deadly” appearance. This stage is usually accompanied by coldness and complete numbness. Then the fingers turn bluish or purple due to the lack of oxygenated blood in the area. When the attack ends and the blood vessels relax, the blood flow resumes. With this sudden rush of blood, the fingers turn bright red and are often accompanied by uncomfortable sensations such as throbbing, pricking, tingling and burning.
So what triggers these attacks? Triggers vary from person to person, but the most common ones are the following:
- Cold weather
- Contact with cold water
- Getting something from the refrigerator or freezer
- Direct impact of the air conditioner
- High emotional stress
- Anxiety or excitement
Raynaud’s does not only affect the fingers and toes. Other parts of the body can also be affected by attacks:
- Nose tip
- Earlobes
- Lips
- Nipple tips
Attacks can last anywhere from a few minutes to several hours. The frequency is also completely individualized; some people experience an attack every day, while for others it may be a recurring event only a few times a year.
What Causes Raynaud’s Disease and Who is at Risk?
“Why did this happen to me?” is one of the most common questions asked by diagnosed patients. The causes of Raynaud’s disease vary depending on whether it is primary or secondary.
In primary Raynaud’s there is no clear disease. The main problem is thought to be that the nerves that control the blood vessels are too sensitive to cold and stress. So much so that the blood vessels “slam on the brakes” much more easily and powerfully than in a normal person. There is strong evidence that genetic factors also play a role, so if Raynaud’s runs in your family, you are more likely to get it.
Secondary Raynaud’s is different, because here Raynaud’s is a precursor to another problem. The underlying causes are mainly connective tissue diseases. These are autoimmune conditions in which the body’s immune system attacks its own healthy tissues.
The most common conditions and factors that can lead to secondary Raynaud’s include
- Scleroderma
- Lupus (SLE)
- Rheumatoid Arthritis
- Sjegren Syndrome
- Atherosclerosis (arteriosclerosis)
- Buerger’s Disease
- Constant use of vibrating tools (construction workers, miners, etc.)
- Repetitive hand movements (pianists, typists)
- Past trauma to the hand or foot area (fracture, frostbite, etc.)
- Smoking (Nicotine is a powerful vasoconstrictor)
Some of the medicines we take can also trigger or worsen Raynaud’s attacks:
- Some blood pressure medicines (Beta blockers)
- Some medicines used in the treatment of migraine
- Attention deficit and hyperactivity disorder (ADHD) medications
- Some chemotherapy drugs
- Cold sensing and allergy medicines containing pseudoephedrine
It is therefore extremely important that when talking to your doctor you provide a complete list of all prescription and non-prescription medicines and herbal supplements you are taking.
What methods are used to diagnose Raynaud’s Disease?
The diagnosis of Raynaud’s disease is usually based on the typical history given by the patient. However, certain steps are taken to confirm the diagnosis and, most importantly, to understand whether the condition is primary or secondary. This distinction forms the backbone of the treatment plan.
The process begins with your doctor listening carefully to you. You will be asked extensive questions about your medical history, details of your symptoms, triggers, family history and lifestyle habits. In the physical examination that follows, your circulatory system, skin and fingers are examined in detail.
In addition to patient history and physical examination findings, some special tests may be used to clarify the diagnosis.
Fingernail Capillaroscopy: This test is the gold standard for the detection of secondary Raynaud’s. It is a simple, painless and microscopic method to examine the structure of the capillaries at the base of the nail. In primary Raynaud’s, these capillaries usually have a normal and regular appearance, whereas in secondary Raynaud’s, especially due to connective tissue diseases such as scleroderma, typical abnormalities such as dilation, damage or loss of vessels can be detected.
Blood Tests: If secondary Raynaud’s is suspected, blood tests are ordered to look for an underlying autoimmune or inflammatory condition.
The main blood tests that are likely to be ordered are the following:
- Antinuclear Antibody (ANA)
- Erythrocyte Sedimentation Rate (ESR or sedim)
- Complete Blood Count (CBC)
- Rheumatoid Factor (RF)
The results of these tests help the doctor determine the type of Raynaud’s and diagnose the underlying disease if it is secondary. It should be remembered that the diagnosis of “Primary Raynaud’s” is usually made after secondary causes have been carefully investigated and ruled out. In addition, the best diagnostic method is computed angiography or conventional peripheral angiography. On angiography, the radial and ulnar arteries appear thin or faint, and the vessels of the hand are not visible.
What Approaches Are Available for the Treatment of Raynaud’s Disease?
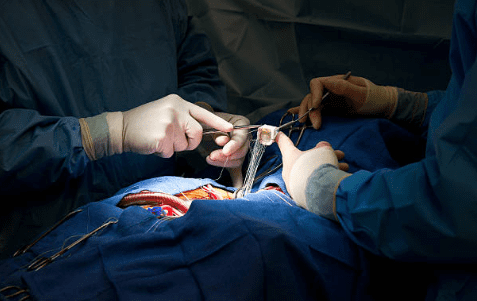
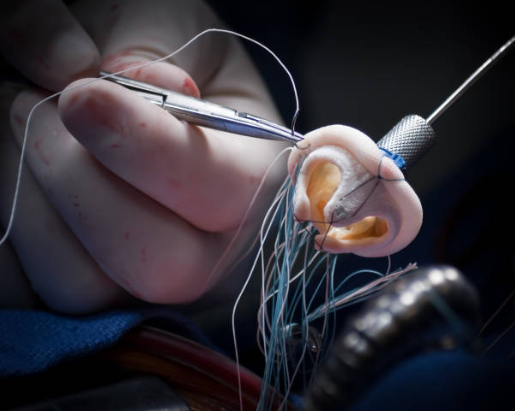
Many patients wonder, “Is there a cure for Reyno’s disease?” The only definitive treatment to completely eliminate Raynaud’s disease is thoracic sympathectomy, which is performed surgically to reduce sympathetic activation. . For this purpose, at least 3 of the sympathetic ganglia and their chain must be completely removed. Vasoconstriction (spasm) in the capillary, i.e. thin-capillary arterial circulation in the hands Immediately after surgery, warming of the hands begins, and in the long term, discoloration improves. Other medications such as calcium channel blockers and blood thinners are not beneficial. Conversely, in large and thin patients, it can increase the severity of the disease by lowering blood pressure and causing spasm of the thin-aproned arteries.
Is Raynaud’s Disease a Dangerous Condition?
This question is one of the biggest concerns of patients. the answer to the questions “Is Raynaud’s disease dangerous?” or “Is Raynaud’s disease fatal?” depends on the type and severity of the disease.
Primary Raynaud’s is usually benign, manageable and not life-threatening. The risk of complications is extremely low.
However, secondary Raynaud’s or very severe, untreated cases of Raynaud’s can carry some serious risks. Rather than being life-threatening, these risks impair quality of life and threaten limb health.
The most important potential complications are the following:
- Digital ulcers (painful and difficult to heal wounds on the tips of the fingers)
- Infection of wounds
- Permanent damage and disfigurement of the skin and nails
- Tissue death (gangrene) and resulting finger loss (amputation)
This list of complications may seem alarming. However, it should be remembered that they are rare and usually only occur in the most severe, untreated cases of secondary Raynaud’s. The most effective way to prevent these serious complications is to perform a sympathectomy to reduce the spasm of the thin-valved arteries in the hands that impair nutrition.
After Raynaud’s Disease Surgery
| Type of Surgery | Usually thoracic or lumbar sympathectomy for the feet |
| The Progression of Renewal | Average 7-10 days; may vary depending on the type of surgery and the region where it is performed. |
| Physical Activity | Rest is recommended for the first week, after which there may be a gradual return to daily activities. |
| Effectiveness | Decrease in vasospasms and increase in temperature, decrease in pain. |
| Drug Use | Some patients may also require vasodilator treatment after surgery. |
| Wound Care | The incision (or thoracoscopic access) site should be kept clean and dry; signs of infection should be monitored. |
| Complications | Rare; Compensatory sweating, Horner’s syndrome (in thoracic sympathectomy), |
| Cold Protection | Although postoperative symptoms subside, protection from cold is important; gloves and warm clothing are recommended. |
| Nutrition | A general healthy diet to support circulation is recommended; no special diet is required. |
| Smoking and Alcohol | Smoking in particular should be stopped; it increases vasoconstriction. Alcohol should be limited. |
| Psychological Support | Psychological counseling may be helpful for chronic discomfort and recurrent attacks. |
| Sexual Activity | It is usually possible within 1-2 weeks, after general improvement has been achieved. |
| Tool Usage | It can be started as soon as reflexes and mobility return to normal (usually after 1 week). |
| Controls | Surgical control is recommended in the first month postoperatively and thereafter according to symptoms. |
Frequently Asked Questions
What is the difference between Raynaud’s phenomenon and Raynaud’s disease, and which part is it?
Raynaud’s phenomenon refers to temporary circulatory disorders such as bruising, swelling and discoloration of the fingers in the cold, with triggers such as stress. If there is no other systemic disease underlying these symptoms, it is called “Raynaud’s disease” (primary Raynaud’s) and is the most benign type. If there are additional symptoms such as difficulty swallowing, joint pains, etc., this is called “Raynaud’s phenomenon” and is most often a symptom of an underlying rheumatic disease. For diagnosis and treatment, it is first necessary to consult Cardiovascular Surgery and, if there are systemic findings, the Department of Rheumatology. This is a team game!
Where does Raynaud’s disease occur?
Raynaud’s is most common on the fingers and toes, rarely on the tip of the nose, earlobes, lips or tongue. In the cold or under stress, the fingers may first turn white, then bruise and finally turn red. Sometimes similar symptoms can occur in the nose and ears.
When does Raynaud’s phenomenon happen?
Raynaud’s attacks usually start suddenly after cold air, contact with cold objects or emotional stress. It can start with simple triggers such as going outside in winter without gloves or taking something from the refrigerator. Sometimes it can also be seen in people using vibrating tools.
How is Raynaud’s phenomenon diagnosed?
The most important diagnostic clue is the history of discoloration of the fingers in the cold. If necessary, a cold stress test and nail bed capillaroscopy are performed. Various blood tests may be ordered to see if there is an underlying disease. Whether it is primary or secondary is important for diagnosis.
How does Raynaud’s phenomenon go away?
To completely relieve Raynaud’s, the nerves must be removed with a thoracic sympathectomy. Other than that, quitting smoking and managing stress are the best preventive approaches. In some patients, vasodilator drugs may be tried. Protection from the cold is also very effective.
Does Raynaud’s phenomenon spread?
Raynaud’s is not contagious, but over time it can spread to other fingers and even toes. If there is an underlying disease, the severity and spread of Raynaud’s can increase. The course of the condition should be monitored by regular medical check-ups.
What is the Raynaud’s phenomenon test and how is it done?
The most valuable test is nail bed capillaroscopy. A drop of oil is applied to the base of your nail and the vasculature is examined under a microscope. Blood tests are also performed to see if there is any other underlying disease. It is a painless and easy process.
What is Raynaud’s phenomenon with connective tissue disease?
In this case, Raynaud’s is a symptom of another disease. Raynaud’s phenomenon is common in connective tissue diseases such as scleroderma, lupus and rheumatoid arthritis. This increases the risk of scarring of the fingers and treatment is usually directed at the underlying disease.
What is Raynaud’s disease?
Raynaud’s disease is the most common benign type of Raynaud’s disease that occurs in the absence of another disease (primary). It usually starts at a young age, especially in women. Symptoms are mild, often manageable with cold protection and lifestyle changes.
In which diseases is Raynaud’s phenomenon most common?
Raynaud’s phenomenon is most common in rheumatic diseases such as scleroderma, lupus, Sjögren’s syndrome, rheumatoid arthritis, but also in some vascular diseases or drug side effects.
Does Raynaud’s disease cause pain?
Yes, during an attack, the fingers first turn white and the pain is usually mild. As the blood flow returns, i.e. the fingers turn from blue to red, there may be a throbbing, tingling and stabbing pain. The pain may be more pronounced in prolonged attacks or if a wound develops.
What foods are good for Raynaud’s Syndrome?
There is no miracle diet, but omega-3-rich fish, ginger, turmeric, antioxidant-rich dark green leafy vegetables and berries support vascular health. It is useful to avoid substances that can shrink blood vessels, such as caffeine and alcohol.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Prof. Dr. Yavuz Beşoğul » General » Heart Disease: Types, Causes, and SymptomsHeart diseases are [...]
Aug
How the Heart Works
Prof. Dr. Yavuz Beşoğul » General » How the Heart WorksThe heart functions as a [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Prof. Dr. Yavuz Beşoğul » General » How Many Hours Does Heart Valve Surgery Take?Heart [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Prof. Dr. Yavuz Beşoğul » Coronary Artery Bypass » How long does coronary artery bypass [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Prof. Dr. Yavuz Beşoğul » Kalp Kapak Hastalıkları » Kalp Kapak Değişimi Ameliyatı Nedir? Kalp [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Prof. Dr. Yavuz Beşoğul » General » Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki [...]
Aug
Life After Heart Valve Surgery
Prof. Dr. Yavuz Beşoğul » General » Life After Heart Valve SurgeryLife after heart valve [...]
Aug
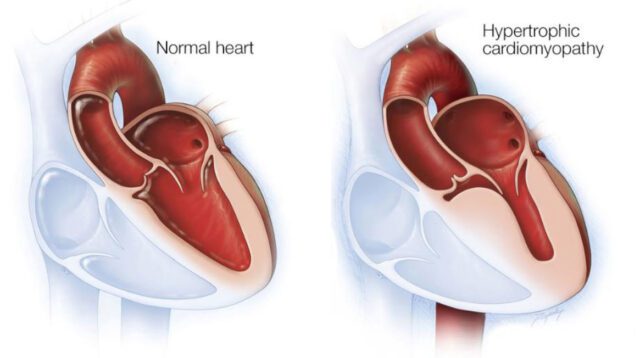
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Prof. Dr. Yavuz Beşoğul » General » Hypertrophic Cardiomyopathy: Symptoms & TreatmentHypertrophic cardiomyopathy is a [...]
Aug