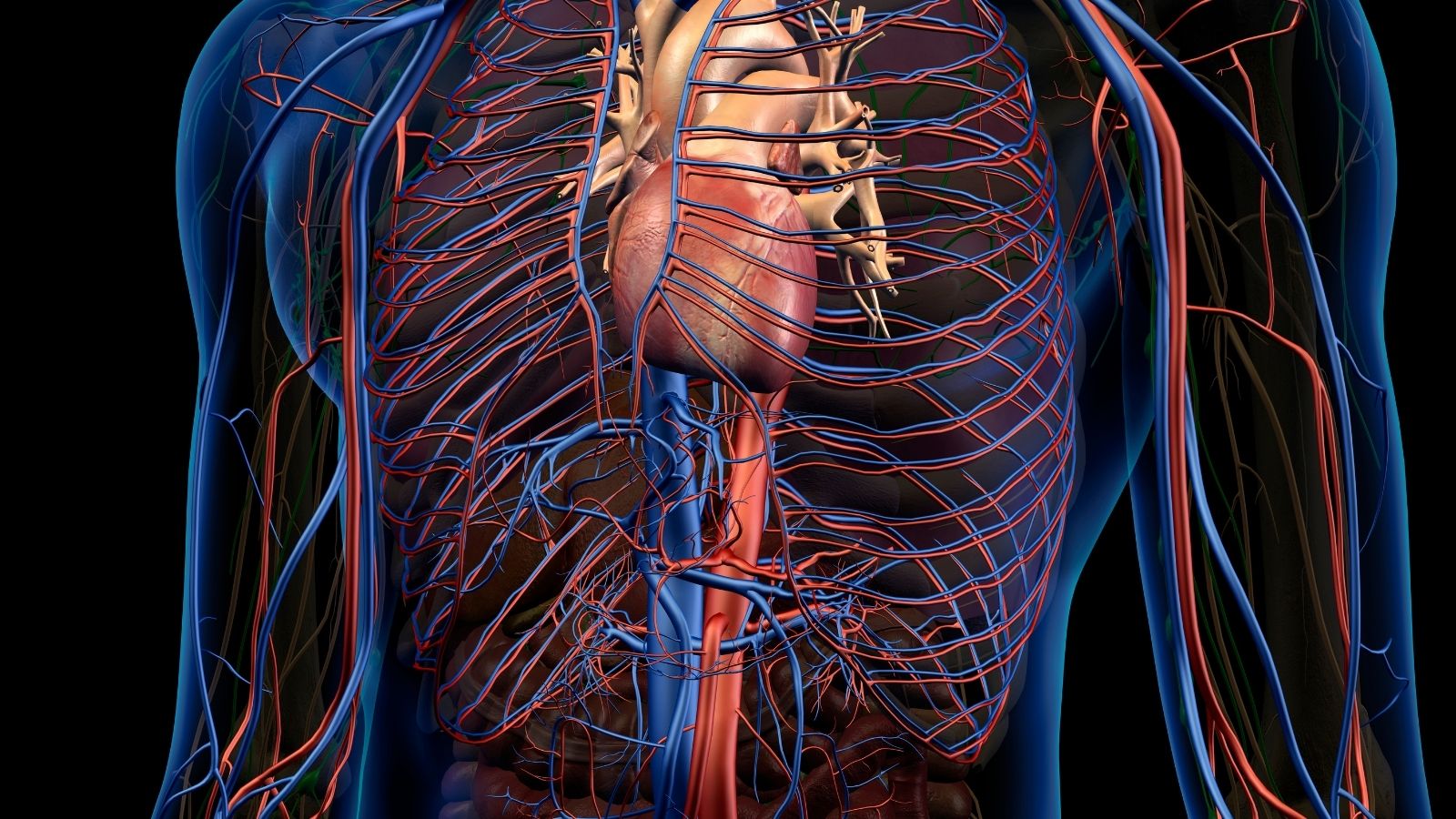
Myocarditis is inflammation of the heart muscle, often caused by viral infections, autoimmune reactions, or toxic exposures. The condition impairs the heart’s ability to pump effectively, leading to arrhythmias and heart failure.
Symptoms of myocarditis include chest pain, fatigue, palpitations, and shortness of breath. In severe cases, sudden cardiac arrest may occur, making early recognition and treatment essential for prognosis.
Diagnostic tools include electrocardiogram, echocardiography, cardiac MRI, and blood markers of inflammation. Endomyocardial biopsy may be required in unclear cases to identify the underlying cause.
Treatment varies depending on severity, ranging from rest and supportive care to immunosuppressive drugs and mechanical circulatory support. In advanced cases, heart transplantation may become necessary.
| Definition | Inflammation of the heart muscle (myocardium) by infection or autoimmune mechanisms |
| Causes | Viral infections (most common), bacterial infections, fungal infections, autoimmune diseases, toxins, certain medications |
| Risk Factors | Immune system weakness, previous infections, autoimmune diseases, chronic diseases, alcohol and drug use |
| Symptoms | Chest pain, shortness of breath, weakness, palpitations, fainting, swelling of the legs, in some cases flu symptoms |
| Diagnostic Methods | ECG, echocardiography, cardiac MRI, blood tests (troponin, CRP), biopsy (if necessary) |
| Treatment Methods | Rest, symptomatic treatment (painkillers, antipyretics), heart failure treatment, antiviral/antibiotic treatment (depending on the cause), immunosuppressive drugs (if necessary) |
| Complications | Heart failure, arrhythmia, cardiomyopathy, sudden cardiac arrest, thromboembolism |
| Prevention Methods | Prevention of infections, vaccinations, compliance with hygiene rules, avoidance of risky drugs and substances |
What Causes Heart Muscle Inflammation?
Inflammation of the heart muscle can have a surprisingly large number of different causes. In the vast majority of cases, however, a viral infection plays a leading role. However, the picture is not always so clear. Sometimes bacteria, fungi, parasites, autoimmune diseases in which the body attacks its own tissues, and even certain medications and toxins can trigger the condition. It is also important to know that in almost half (P) of all cases of myocarditis, no definite cause can be identified despite all the detailed investigations. In medical language, we call this condition “idiopathic myocarditis”. This uncertainty can sometimes make diagnosis and treatment of the disease even more challenging.
The most common infectious causes of myocarditis are the following:
- Adenovirus (common cold virus)
- SARS-CoV-2 (COVID-19 agent)
- Coxsackie virus (gastrointestinal infections)
- Parvovirus B19 (causative agent of rash in children)
- Influenza (flu virus)
- Hepatitis B and C viruses
- Epstein-Barr virus (kissing disease)
- HIV
- Herpes virus (cold sore virus)
- Staphylococci and Streptococci bacteria
- Borrelia burgdorferi (Lyme disease bacterium)
- Fungi such as Candida, Aspergillus
- Parasites such as Trypanosoma cruzi, Toxoplasma
The non-infectious causes of myocarditis are also quite varied. This group includes situations where the body’s own immune system is out of control, drug reactions and various environmental factors:
- Lupus
- Sarcoidosis
- Giant cell arteritis
- Rheumatoid arthritis
- Some cancer drugs (chemotherapy, immunotherapy)
- Antibiotics such as penicillin
- Some epilepsy medicines
- Cocaine
- mRNA COVID-19 vaccines (as a rare side effect)
- Radiation therapy
- Heavy metals (such as lead)
- Carbon monoxide poisoning
Who is at Risk of Heart Muscle Inflammation?
This disease can theoretically affect people of all ages and sexes. However, some groups seem to be statistically one step ahead. Young adults and men in particular seem to be at higher risk. It is important to understand that the concept of “risk” for myocarditis works a little differently from traditional heart disease, such as coronary artery disease as we know it. Rather than lifestyle factors that accumulate over the years, such as smoking or high cholesterol, the risk of myocarditis often depends on unpredictable, sudden events, especially infection. Prevention strategies therefore focus on avoiding these acute infections as much as possible, rather than managing a chronic disease. In fact, the basic hygiene measures we all know – washing hands frequently, avoiding close contact with sick people and keeping the vaccination schedule up to date – are the most practical and effective ways to reduce the risk of exposure to these unexpected triggers.
We can summarize the groups that can be considered at risk as follows:
- Young adults (especially 12-40 years old)
- Men
- Those with a genetic predisposition (although not directly inherited)
- Diabetes patients
- HIV/AIDS carriers
- Those with end-stage renal failure
- Those with eating disorders
- People on dialysis treatment
- Radiotherapy recipients
- Those with devices such as pacemakers or central venous catheters
What are the Symptoms of Heart Muscle Inflammation?
The symptoms of myocarditis are like a chameleon; they vary greatly from person to person and can mimic many other diseases. While some people can survive with almost no symptoms (asymptomatic), others can develop severe, life-threatening symptoms. The most common symptoms of heart infection include chest pain, shortness of breath, extreme fatigue, palpitations and flu-like symptoms.
Perhaps the most critical clue in the diagnostic process is a history of upper respiratory tract infection, diarrhea or fever in the few days or weeks before the onset of cardiac symptoms. Most of our patients tell us a story like, “Doctor, I had a severe flu a week ago, and just when I was recovering, this chest pain and shortness of breath started”. This temporal connection is a very valuable clue for us.
The most common heart-related symptoms are:
- Chest pain (sharp, stabbing or pressing)
- Shortness of breath (both at rest and with exertion)
- Palpitations (fast, strong or irregular beating of the heart)
- Extreme fatigue and exhaustion
- Swelling in the legs and ankles (edema)
- Dizziness
- Fainting (syncope)
Are Heart Muscle Inflammation Symptoms Different in Children?
Definitely yes. The symptoms of heart inflammation in children, especially infants, can be quite different and more deceptive than in adults. This is why parents need to be very careful.
Symptoms that can be seen in newborns and infants are usually the following:
- Fire
- Constant restlessness and crying
- Difficulty breathing (rapid breathing)
- Refusal to feed or fatigue when sucking
- Excessive fatigue and drowsiness
- Pale or mottled appearance of the skin
- Inability to gain weight
In older children, the symptoms begin to more closely resemble those of adults:
- Complaint of chest pain
- A persistent and dry cough
- Extreme fatigue
- Rapid breathing
- Fainting spells
- Significant decrease in exercise capacity (you used to run and play but now get tired quickly)
When to Seek Emergency Medical Assistance?
If you are experiencing unexplained chest pain that you have never experienced before, severe shortness of breath, fainting or palpitations that you can’t stop, these symptoms can indicate both myocarditis and a heart attack. It is impossible to recognize the symptoms of these two deadly conditions on the phone or by yourself at home. You should therefore seek emergency medical help immediately, without hesitating for a second.
You should be especially alert to these “red flag” symptoms:
- A feeling of pressure, tightness or heaviness in your chest that lasts longer than 15 minutes
- Pain radiating to the arms, back, neck or jaw
- This pain is accompanied by shortness of breath
- Cold sweats or nausea
If any of these symptoms are present, the 112 emergency service should be called immediately or the emergency department of the nearest hospital should be consulted.
How Is Heart Muscle Inflammation Diagnosed?
Diagnosing myocarditis is a process that requires piecing together clues like a detective. This is because the symptoms can be very generalized and can be confused with many other conditions. The diagnosis is based on your detailed medical history, a careful physical examination, a series of blood tests, an electrocardiogram (ECG) and the results of various cardiac imaging tests. The assessment and experience of an experienced cardiologist is invaluable in this process. As we listen to you, we will use a stethoscope to try to hear any abnormal sounds or rhythms coming from your heart, and we will question you in detail about any recent infections, whether you have traveled and any medications you are taking. Remember, early diagnosis is the most critical step to prevent permanent damage to your heart.
The main tests we use in the diagnostic process are the following:
- Troponin (the most important blood test showing heart muscle damage)
- CRP and Sedimentation (shows general inflammation in the body)
- Complete Blood Count (CBC)
- Antibody tests or Viral PCR (to find the causative infection)
- Electrocardiogram (ECG)
- Chest X-ray
- Echocardiogram (ECHO – Heart Ultrasound)
- Cardiac Magnetic Resonance (Cardiac MR)
When Is Endomyocardial Biopsy Necessary?
Endomyocardial biopsy, the removal of a very small piece of tissue from your heart, is the “gold standard” diagnostic procedure for myocarditis. However, because this is an invasive procedure that involves accessing the heart through a vein in the groin or neck, it is not routinely performed in all patients. It is usually reserved for special and difficult cases where the diagnosis remains unclear despite all other methods, the patient’s condition deteriorates very rapidly (so-called fulminant myocarditis) or there is no response to standard treatments.
The purpose of a biopsy is not just to say “yes, this is myocarditis”. Its main purpose is to determine the type and character of the inflammation. For example, if the biopsy reveals a very rare and aggressive form of Giant Cell Myocarditis, it completely changes our treatment plan. Instead of standard supportive therapies, we need to immediately start strong immunosuppressive drugs. Biopsy is therefore a key step that opens the door to the right treatment and saves lives, especially in selected patients with severe conditions.
Are There Different Types of Heart Muscle Inflammation?
Yes, “myocarditis” is an umbrella term that encompasses a spectrum of diseases with different causes, different courses and different treatment approaches. We subdivide inflammation of the heart muscle into various subtypes based on the underlying cause, the speed of onset, the severity and the type of inflammatory cells seen on biopsy. This classification helps us to predict the future course of the disease and determine the most effective treatment strategy.
The most common types of myocarditis are the following:
- Acute Lymphocytic Myocarditis (most common type, usually after viral infection)
- Chronic Myocarditis (long-lasting, recurrent inflammation)
- Fulminant Myocarditis (sudden and very severe onset, the most dangerous form)
- Giant Cell Myocarditis (GCM) (very rare, very aggressive, autoimmune origin)
- Eosinophilic Myocarditis (often associated with drug allergies)
- Myopericarditis (inflammation of both the heart muscle and the lining of the heart)
How to Treat Heart Muscle Inflammation?
The treatment of myocardial infarction is like a tailor making a personalized suit. The treatment plan is completely individualized according to the severity of the disease, its underlying cause, its type and your general health. This treatment, which requires a multifaceted approach, has key goals. Eliminate the underlying cause if possible, reduce the workload on your heart to give it the time and space it needs to heal, and effectively manage dangerous complications that arise along the way, such as heart failure or arrhythmias.
In very mild cases, complete recovery can be achieved with just bed rest and some simple medicines to relieve symptoms. However, the most severe cases, such as fulminant myocarditis, can suddenly turn into life-threatening emergencies. At this point, a large team of cardiologists, cardiovascular surgeons, cardiologists and intensive care specialists get involved and a complex treatment process involving advanced surgical interventions and mechanical support devices begins.
The main groups of medicines we use in treatment are as follows:
- Heart failure medications (beta-blockers, ACE inhibitors, diuretics)
- Anti-inflammatory and immunosuppressive drugs (such as corticosteroids, only in special types)
- Antiarrhythmic drugs (to control rhythm disturbances)
- Anticoagulants (blood thinners, to prevent the risk of clots)
How is the Treatment of Fulminant Heart Muscle Inflammation Different?
Fulminant myocarditis, as the name suggests, is a stormy and lightning-fast progression. This is the form of myocarditis that requires the most urgent and aggressive intervention. Within hours or days, these patients rapidly reach a point called cardiogenic shock, in which the pumping function of the heart completely fails. In this situation, standard drug therapies alone are absolutely insufficient. This is when cardiovascular surgeons, cardiologists and intensive care specialists come into play as a multidisciplinary team. The main goal of the treatment is to give the heart an invaluable “window of time” to recover, using high-tech life support systems to temporarily take over the function of the failing heart.
The advanced life support strategies we use during this critical period are the following:
- Inotropic support (intravenous drugs that increase the contractile force of the heart)
- ECMO (Extracorporeal Membrane Oxygenation – temporary artificial heart-lung machine)
- VADs (Ventricular Assist Devices – assistive pumps implanted in the heart)
- Heart Transplant (the last and definitive solution for hearts that do not heal despite all support)
These devices are temporary bridges that allow the heart to rest and recover. Sometimes the heart heals completely under this support (“bridge to recovery”), sometimes it buys time for patients with permanent damage until a suitable donor heart can be found (“bridge to transplant”).
What are the Possible Complications of Heart Muscle Inflammation?
Unfortunately, inflammation of the heart muscle can lead to serious and sometimes permanent problems, especially if it is not treated in a timely and correct manner or if it is very severe.
The most common potential complications are the following:
- Heart failure
- Dilated cardiomyopathy (permanent weakening and enlargement of the heart muscle)
- Life-threatening arrhythmias (rhythm disturbances)
- Blood clot formation inside the heart
- Stroke or heart attack (as a result of a blood clot)
- Sudden cardiac death
How is the Recovery and Long-Term Outlook after Heart Muscle Inflammation?
The recovery process varies greatly from person to person, depending on the initial severity of the disease and how much damage it has done to your heart. It can take anywhere from a few months to a year or even longer. The most important and absolutely uncompromising rule during this period is to give your heart enough time to rest and repair itself.
The most important points to be considered during the healing process are the following:
- Absolute rest (especially the first 3-6 months)
- Avoiding competitive sports and heavy exercise
- Low salt diet
- Avoid alcohol and smoking
- Slow and gradual return to activity (under medical supervision)
- Regular and lifelong cardiologist follow-up
As for the long-term outlook, a significant proportion of our patients, especially mild cases, recover and return to their normal, active lives. Even patients who survive the most severe cases, such as fulminant myocarditis, can have surprisingly good long-term outcomes. But large and important studies in recent years have shown us a critical fact. Even cases of myocarditis that initially appear to be “uneventful” or “mild” have a significantly higher risk of heart failure, arrhythmias and other serious cardiovascular problems later in life than the general population. This finding taught us that myocarditis should not be seen as a “once and done” disease. Even if the inflammation completely resolves clinically, microscopic scar tissue or electrical sensitivity left behind can leave you more vulnerable to future heart problems. It is therefore vital that every patient diagnosed with myocarditis, no matter how well they feel, is followed up regularly by a cardiologist to protect their future health.
Frequently Asked Questions
What is myocarditis?
Myocarditis is an inflammation of the heart muscle. It often develops due to viral infections and can affect the pumping power of the heart.
What causes myocarditis?
Viruses are the most common cause. It can also be caused by bacterial infections, immune system diseases, drug reactions and toxins.
What are the symptoms?
Chest pain, shortness of breath, palpitations, weakness and sometimes fainting are the most common symptoms.
Is myocarditis contagious?
The virus that causes it, rather than the disease itself, can be contagious. However, myocarditis is not transmitted directly from person to person.
Is it a dangerous disease?
Yes, it can cause heart failure, arrhythmias and sudden cardiac arrest, especially if left undiagnosed and untreated.
How is the diagnosis made?
It is diagnosed by ECG, echocardiography, blood tests, cardiac MRI and rarely biopsy.
Does myocarditis leave permanent damage?
While mild cases may recover completely, some patients may develop permanent heart muscle damage and heart failure.
Is myocarditis the same as a heart attack?
Answer. While a heart attack is caused by blockage of blood vessels, myocarditis is an inflammatory condition.
What is the treatment?
Depending on the underlying cause, antiviral or antibiotic treatment, medication to support heart function and bed rest are recommended.
How long does the healing process take?
In mild cases, recovery can be achieved within a few weeks. Severe cases may require months of treatment and follow-up.
Does myocarditis recur?
It can rarely recur. The risk increases especially if there are underlying immune problems.
Can I exercise?
Exercise is not recommended during active myocarditis. The exercise plan after recovery should be under the supervision of a doctor.
What should be considered in nutrition?
It is important to eat heart-healthy foods low in salt and fat and to ensure adequate fluid intake.
Do vaccines cause myocarditis?
In rare cases, myocarditis associated with some vaccines has been reported. But this risk is very low and the benefits outweigh the risks.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.