Bicuspid valve surgery is a procedure performed to repair or replace the aortic valve in patients born with only two valve leaflets instead of three. This congenital abnormality may cause stenosis or regurgitation, impairing blood flow and straining the heart. Surgery ensures proper circulation and valve function.
Indications for bicuspid valve surgery include severe valve narrowing, significant regurgitation, or symptomatic heart failure. Advanced imaging such as echocardiography and CT scans guides surgical decision-making. Timely surgery prevents complications like aortic aneurysm and left ventricular dysfunction.
Surgical techniques vary from valve repair to mechanical or biological valve replacement. Minimally invasive approaches and transcatheter procedures are increasingly used, depending on patient condition and risk factors. Each method aims to restore effective blood flow and reduce cardiac workload.
Post-surgery follow-up involves lifelong cardiac monitoring, anticoagulant therapy in mechanical valve patients, and lifestyle modifications. Regular imaging is essential to assess valve function and detect potential complications early. Successful surgery significantly improves prognosis and life expectancy.
| Definition | Congenital bicuspid aortic valve with two leaflets instead of three |
| Causes | Congenital structural anomaly; genetic predisposition |
| Risk Factors | Family history of bicuspid aortic valve, some genetic syndromes (Turner syndrome etc.) |
| Symptoms | Most of the time asymptomatic in childhood; shortness of breath on exertion, fatigue, chest pain, palpitations, murmur in later years |
| Diagnostic Methods | Echocardiography (the most important diagnostic method), ECG, cardiac MRI, CT-angiography |
| Treatment Methods | Regular follow-up, medication (if symptoms are present), surgery (valve repair or replacement) in severe stenosis or insufficiency, endocarditis prophylaxis |
| Complications | Aortic stenosis, aortic insufficiency, aortic aneurysm, infective endocarditis, heart failure |
| Prevention Methods | No specific prevention; regular cardiologic follow-up, infective endocarditis prophylaxis in risky procedures, family screening |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is a bicuspid aortic valve and how does it differ from a normal aortic valve?

When the left ventricle, the main pump of the heart, contracts, the aortic valve opens to allow oxygen-rich blood to flow throughout the body. When the contraction is over, it closes immediately, preventing blood from escaping back into the heart. A normal valve has three leaflets and this structure distributes the mechanical stress and pressure generated during opening and closing to three equal points, providing a perfect balance. It is like three people carrying a load; each one has less weight and wear and tear is slow.
In a bicuspid aortic valve, there are only two leaflets that carry this load. This causes the stress of each heartbeat to be placed on only two points. Just as the two wheels of a car are subjected to more and more stress, the bicuspid valve leaflets wear out faster over time. In addition, the flow of blood through the bicuspid valve becomes more turbulent, rather than smooth. This abnormal mechanical stress and turbulent blood flow over many years sets the stage for hardening, thickening and, most importantly, calcification of the valve leaflets. This process leads to either incomplete opening of the valve (aortic stenosis) or incomplete closure (aortic insufficiency) and is the basis of major heart problems.
What is the prevalence of bicuspid aorta in the population?
Contrary to popular belief, a bicuspid aortic valve is not a rare condition. In fact, it is the most common of all congenital heart anomalies. It is thought to affect around 1% to 2% of the general population. This means that roughly one in every 50-100 people has this condition. It is also noteworthy that it is about two to three times more common in men than in women.
The fact that this condition is so common means that the medical community is highly experienced in diagnosing, monitoring and treating bicuspid aorta and the potential problems associated with it. But it also means that it is a risk factor that millions of people carry without realizing it, which can affect their heart health in the future. It is therefore important to be informed about the condition and to be under medical supervision when necessary.
What are the underlying causes of a bicuspid aortic valve?
A bicuspid aortic valve is a phenomenon that occurs during fetal development in the womb, in the early weeks of the heart’s formation. The three separate pads of tissue that would normally form the aortic valve do not separate as they should during development and two remain joined. As a result, the valve completes its development with two leaflets. Although the cause of this developmental defect remains unclear, the evidence points very strongly to a genetic basis.
One of the most critical points in understanding bicuspid aorta is to know that it is not just an isolated valve problem. It is part of a broader syndrome often referred to as “valvulo-aortopathy”, which affects both the valve (valvulo) and the aortic vessel (aortopathy). This is because both the aortic valve and the main body of the aortic vessel develop embryologically from the same set of stem cells. Therefore, an error in the genetic program that governs the development of these cells can cause both the valve to be abnormal and the wall of the aortic vessel to be congenitally weaker, less flexible and more prone to dilate over time. This connection scientifically explains why an aneurysm (dilatation) of the aortic vessel can develop even in patients with a bicuspid aorta with completely normal valve function.
Is bicuspid aorta a hereditary condition and what does the risk of familial transmission mean?
Yes, bicuspid aortic valve definitely has a strong hereditary component. Scientific studies show that this condition clusters in families. When a person is diagnosed with bicuspid aorta, his or her first-degree relatives (i.e. parents, siblings and children) are about 10 times more likely to have the condition than the general population. This risk is reported to vary between 9% and %.
This high genetic transmission has a very important practical consequence: Family screening. When one person is diagnosed with bicuspid aorta, it is no longer just a concern for that individual, but a potential health screening for the whole family. Even more interestingly, some studies have shown that even first-degree relatives who do not have a bicuspid valve themselves have an increased risk of aortic dilatation (aortopathy). For these reasons, all leading cardiology organizations, such as the American Heart Association (AHA) and the American College of Cardiology (ACC), strongly recommend that all first-degree relatives of every person diagnosed with a bicuspid aortic valve should be screened at least once with echocardiography (ultrasound of the heart), even if they have no symptoms. This is a vital and proactive step to protect family members who may be asymptomatic and at risk.
What are the most common symptoms of bicuspid aortic disease?
One of the most deceptive aspects of a bicuspid aortic valve is that it can remain completely silent for years, even decades. Many people have an active childhood and adolescence without realizing that they are living with this structural difference. Symptoms usually appear when the wear and tear of the valve progresses and begins to affect heart function, i.e. when the valve becomes severely narrowed (stenosis) or leaky (regurgitation). This usually occurs in middle age and beyond. Symptoms of a bicuspid aortic valve are a sign that the heart is no longer able to cope with the increased workload. The most common symptoms are:
- Shortness of breath (especially with exertion or going uphill)
- Feeling of pressure, tightness or pain in the chest (angina)
- Dizziness or darkening of the eyes with exertion
- Fainting (syncope)
- Fatigue more quickly than usual and decreased effort capacity
- Palpitations (feeling that the heart beats irregularly, rapidly or very strongly)
How is bicuspid aorta diagnosed?
Bicuspid aorta is often diagnosed unexpectedly, during a routine medical examination for another reason. Often the first clue is an abnormal sound called a “murmur”, which the doctor hears while listening to the heart with a stethoscope. This murmur is the sound of the turbulent flow of blood as it passes through the abnormal, two-leaflet valve. Sometimes, in addition to the murmur, a sharp “clicking” sound can be heard as the hardened valve opens.
Based on these findings, the doctor will order additional tests to clarify the situation. The gold standard method for diagnosing bicuspid aorta is echocardiography (ECHO), an ultrasound of the heart. This painless and harmless test uses sound waves to create moving images of the heart and valves. ECHO provides a clear view of the valve’s two-leaflet structure and can measure whether there is calcification, how narrow it is or how much it is leaking. It also assesses how much the heart is affected, whether the heart muscle has thickened and its pumping capacity. To measure the diameter of the aorta in more detail, advanced imaging methods such as computed tomography (CT) or cardiac magnetic resonance imaging (MRI) can be used.
What serious complications can a bicuspid aortic valve cause?
Over time, a bicuspid aortic valve can set the stage for a number of important complications that can seriously affect the functioning of the heart and aortic artery. These complications usually develop gradually and over many years. The main potential problems are:
- Aortic Stenosis (Stenosis)
- Aortic Insufficiency (Regurgitation)
- Aortopathy (Enlargement or Aneurysm of the Aortic Vessel)
- Aortic Dissection (Rupture of the Aortic Vessel)
- Infective Endocarditis (Heart Valve Infection)
- Heart Failure
Each of these complications is a serious health problem in its own right and makes it clear why patients with bicuspid aorta should be under regular lifelong monitoring. Early detection and follow-up allows intervention before these complications reach a dangerous level.

What causes an enlargement of the aortic vessel (aneurysm) in the presence of a bicuspid aorta?
In patients with bicuspid aorta, progressive dilatation of the aorta, especially the first part where it exits the heart (ascending aorta), is quite common. There is a “two-hit” mechanism behind this situation.
The first is the genetic weakness we mentioned earlier. The genetic factors that cause bicuspid valve formation also affect the structure of the elastic fibers and smooth muscle cells that are the building blocks of the aortic wall, making it congenitally weaker and prone to dilation.
The second is hemodynamic stress. The blood flow out of the two-leaflet valve is jet-like, asymmetric and turbulent, rather than smooth and laminar as normal. Over many years, this abnormal flow continually hits a specific area of the aortic wall like water from a hose. This chronic mechanical bombardment causes the already genetically weak aortic wall to become even more worn and weakened, and over time to expand like a balloon (aneurysm). The combination of these two factors puts patients with a bicuspid aorta at higher risk for aortic aneurysm and its most feared complication, aortic rupture (dissection).
Does a bicuspid aortic valve carry a risk of death?
This question is the biggest concern of patients and their relatives and the answer clearly depends on the management. A diagnosis of bicuspid aorta alone does not mean a risk of death. If a person is followed regularly by a cardiologist, adheres to the necessary lifestyle changes, and if surgical intervention is performed at the right time when complications develop (such as severe valve disease or aortic aneurysm), life expectancy is no different or very close to that of the general population.
However, the risk of death from a bicuspid aorta becomes a real danger when the condition is neglected and untreated. For example, if aortic stenosis with severe symptoms is left untreated, the risk of heart failure and sudden death within a few years is very high. Similarly, an aortic aneurysm that has reached a critical diameter of 5.5 cm can rupture (dissection) at any time if left untreated, often with fatal consequences. Therefore, it is not the bicuspid aorta itself that carries the risk of death, but its serious complications that go untreated. Proactive monitoring and timely intervention is the most effective way to eliminate this risk.
What should be the management of patients with bicuspid aorta who do not require surgery?
For patients with bicuspid aorta who do not have severe valvular disease or dangerously large aortic aneurysms, the treatment is “active monitoring and risk management”, not surgery. This is not a passive “wait and see” approach; rather, it involves proactive steps to slow disease progression and delay the need for surgery as long as possible. The cornerstones of this process are:
-
- Regular lifelong cardiologist check-ups
-
- Echocardiography follow-up at intervals determined according to the severity of the disease
-
- Follow-up of the aortic vessel with CT or MRI if necessary
-
- Keeping blood pressure (blood pressure) under strict control
-
- Absolute cessation of smoking
-
- Maintaining a healthy weight
-
- Good oral and dental hygiene (to reduce the risk of infective endocarditis)
-
- Adopting a heart-friendly diet
What are the exercise recommendations for patients with bicuspid aorta?
Regular physical activity is beneficial for overall heart health and is also encouraged for patients with bicuspid aorta. However, the exercise plan must be individually tailored to the severity of the disease.
Generally safe and recommended exercises include the following:
-
- Brisk walking
-
- Swimming
-
- Cycling
-
- Light jogging
-
- Resistance exercises with light weights that do not require breath holding
However, patients with severe aortic stenosis, severe aortic insufficiency or significant aortic dilatation should avoid certain activities that can raise blood pressure suddenly and excessively, posing a risk. Types of exercise to avoid include the following:
-
- Heavy weight lifting (bodybuilding, weightlifting)
-
- Competitive sports requiring maximal effort
-
- Isometric movements with breath holding such as push-ups, pull-ups
-
- Sports with contact and impact risk such as boxing, wrestling, rugby
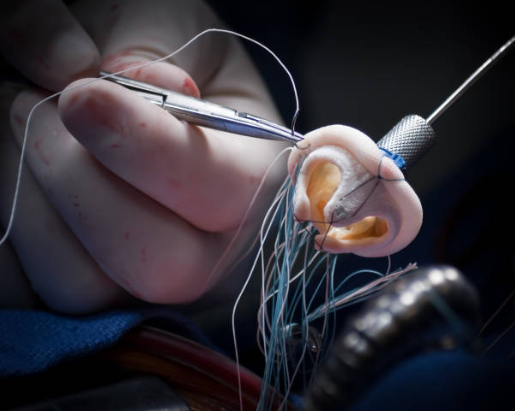
When is surgical treatment for bicuspid aorta mandatory?
 Bicuspid Aortic Valve Surgery
Bicuspid Aortic Valve Surgery
The decision to perform surgery for a bicuspid aortic valve is made in a preventive manner, without waiting for irreversible damage to the heart or aortic vessel. The timing of surgery is based on objective measurements obtained from tests such as echocardiography rather than the patient’s complaints. The main conditions that necessitate surgical intervention are as follows:
- Symptoms (shortness of breath, chest pain, fainting) due to severe valve disease (stenosis or insufficiency).
- Decreased pumping power of the heart (left ventricular ejection fraction below U), even if there are no symptoms.
- Excessive enlargement of the heart, even if there are no symptoms.
- Even if there are no symptoms, aortic stenosis has reached a very advanced stage (blood flow velocity through the valve exceeds 5 m/s).
- The diameter of the aorta reaches a critical threshold (usually 5.5 cm in those without risk factors and 5.0 cm in those with risk factors), which puts them at risk of rupture.
- In a patient scheduled for another heart operation (e.g. coronary bypass), if the aortic diameter exceeds 4.5 cm, repair of the aorta in the same session to prevent a second operation in the future.
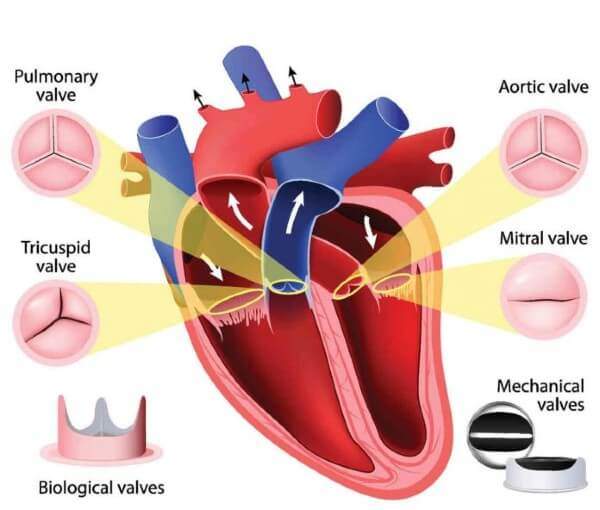
Which valve types are used in bicuspid aortic surgery? mechanical or biological?
When aortic valve replacement surgery is required, one of the most important decisions that the patient and surgeon must make together is the type of new valve to be implanted. Both options have their own advantages and disadvantages.
Mechanical Covers: They are usually made of very durable carbon materials.
Advantages:
- Lifetime durability (theoretically they do not wear out).
Disadvantages:
- Obligation to take blood thinners (Coumadin) for life.
- Need for regular blood test (INR) monitoring.
- Increased risk of bleeding.
- A slight “clicking” sound that some patients can hear.
Bioprosthetic (Biological) Valves: They are usually made from specially treated bovine or porcine heart tissue.
Advantages:
- No need to use blood thinners (except in special cases).
- More natural blood flow and quieter operation.
Disadvantages:
- Limited durability (usually 10-20 years).
- The possibility of deterioration over time and the need for reoperation.
In general, mechanical valves are preferred for young and active patients under the age of 60-65 due to their durability, while bioprosthetic valves are preferred for patients over the age of 65-70 because they do not require blood thinners and are less likely to require reoperation. However, this decision is a joint decision to be made by the patient and his/her doctor in line with the patient’s lifestyle, expectations and personal preferences.
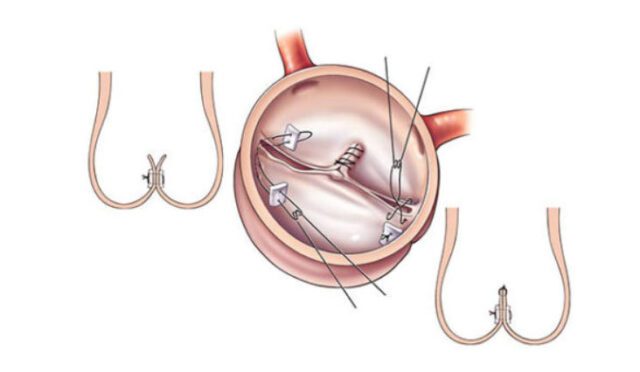
Is TAVR (catheterized valve replacement) an option in patients with bicuspid aorta?
TAVR (Transcatheter Aortic Valve Implantation) is a less invasive procedure that has revolutionized the treatment of aortic stenosis in recent years. Instead of open heart surgery, a catheter is usually inserted through an artery in the groin to deliver a new compressed bioprosthetic valve to the heart and insert it into the narrowed old valve.
It is a viable alternative, especially for older patients or those with additional health conditions who are at high risk for open heart surgery. However, TAVR in patients with bicuspid aorta presents some special challenges. The non-circular elliptical structure and irregular calcification of bicuspid valves can make it difficult for standard TAVR valves to fit. This may slightly increase the risk of leakage from the edge of the new valve (paravalvular leak) and the need for a permanent pacemaker. Therefore, for young and low surgical risk bicuspid aortic patients, traditional open heart surgery (SAVR) is still considered the gold standard, with proven long-term results and the possibility to repair an aortic aneurysm at the same time. TAVR is a valuable option for selected patients with bicuspid aorta and appropriate anatomy.
What is the long-term life expectancy of patients with bicuspid aorta?
The clearest and most reassuring answer to this question is the following: With proper follow-up and timely intervention, the life expectancy of individuals with bicuspid aortic valves is very close to that of the general population. Thanks to modern medical and surgical techniques, it is possible for patients to achieve a normal or near-normal life expectancy and quality.
However, an important distinction needs to be made here: “overall life expectancy” versus “event-free life expectancy”. Although patients may live a normal life, there is a high probability that they will experience a major cardiac event (usually surgery) during this lifetime. Studies show that a significant proportion of patients (% to P) will need surgery at some point in their lives. This shows that bicuspid aortic management is not a sprint but a lifelong marathon. In particular, it should be kept in mind that a patient who undergoes surgery at a young age may need a second intervention, for example, 15-20 years later due to a bioprosthetic valve wearing out. Adopting this concept of “lifelong management” is the key to a long and healthy life.
Why is lifelong follow-up important after a diagnosis of bicuspid aorta?
A bicuspid aortic valve is a lifelong companion from the moment of diagnosis. Due to the progressive nature of the condition, it is vital that the patient remains under lifelong cardiologic follow-up, even if they have no complaints or have had a successful surgery. The main objectives of this follow-up are:
- Early detection of the slightest deterioration in valve function.
- Closely monitor the increase in the diameter of the aortic vessel.
- Determining the best and safest time for surgical intervention.
- To check the condition of the prosthetic valve after surgery.
- Continue to monitor the parts of the aortic vessel that were not replaced during surgery.
- Keeping risk factors such as blood pressure under constant control.
This regular follow-up protocol is a safety net that protects the patient from potential dangers. Thanks to this network, complications can be detected and necessary interventions planned before they cause irreversible damage. This proactive approach is the most important factor in ensuring that patients with bicuspid aortic valves live long, healthy and high-quality lives.
After Bicuspid AORT (BAK) Surgery
| Type of Surgery | Aortic valve repair, valve replacement (mechanical or biological), in some cases ascending aortic replacement if aortic dilatation is present. |
| Recovery Time | Average 10-15 days depending on the valve type and the presence of concomitant aortic surgery. |
| Medication Use | Lifelong warfarin (with INR monitoring) for mechanical valves, usually short-term anticoagulant therapy for biological valves. |
| INR Monitoring | For mechanical valve, the target is usually 2.5-3.5; regular follow-up is required. |
| Imaging and Control | Valve function and aortic diameter, if present, should be monitored by regular echocardiography. More frequent follow-up is recommended in the first year. |
| Complications | There is a risk of valvular dysfunction, thromboembolism, endocarditis, aortic dilatation and arrhythmia. |
| Blood Pressure Control | It is especially important in patients with aortic dilatation; beta-blockers are often used. |
| Physical Activity | Light to moderate exercise is recommended; heavy lifting and activities that cause a sudden increase in pressure are not recommended. |
| Nutrition | A heart-friendly diet with attention to vitamin K balance (especially for those on warfarin) is recommended. |
| Smoking and Alcohol | Definitely not recommended; it poses a serious risk for aortic and valve health. |
| Sexual Activity | It can usually be started within 4-6 weeks once physical competence is achieved. |
| Psychological Support | Long-term medication use and the need for monitoring may lead to the need for psychological support. |
| Vehicle Use | It can usually be started after 2-4 weeks when reflex and attention are appropriate. |
| Controls | Cardiology follow-up is required for life; frequent follow-up is recommended in the first year after surgery, and annual follow-up thereafter. |
Frequently Asked Questions
What is the risk of death from bicuspid aorta?
Living with a bicuspid aortic valve is usually not a serious risk. However, if the valve develops stenosis or insufficiency, it can fatigue the heart and lead to heart failure and the risk of enlargement of the aortic artery (aneurysm). In advanced and untreated cases, it can be life-threatening. Regular cardiology check-ups are therefore vital.
What percentage of bicuspid aorta is obstructed?
There is no standard obstruction rate for bicuspid aorta. The disability rate is determined individually according to the condition of the valve and the heart. Having only two petals is not an obstacle; however, if there is severe stenosis, insufficiency or enlargement of the heart, the health committee makes a detailed assessment.
Can bicuspid aorta play sports?
If the valve functions are normal and there is no dilatation of the aortic artery, sports that are not overly demanding such as walking, swimming and cycling can be practiced. However, sports that require breath-holding, pushing or competitive sports such as weightlifting may be risky. Your cardiologist’s approval is essential for the safest exercise program.
Can a bicuspid aorta make a pilot?
The health requirements for becoming a pilot are very strict. Bicuspid aortic valve alone may not be a definite obstacle, but even the smallest risk of stenosis, insufficiency or aortic dilatation makes it difficult to apply. Detailed cardiological examinations are decisive; in practice, piloting with this diagnosis is usually not possible.
Does bicuspid valve prevent police and military service?
Yes, a bicuspid aortic valve is generally considered a disqualification for police work and active military service. This is because these professions require high effort and stress, and even mild stenosis or insufficiency is considered “unfit”. Health regulations have very clear rules for cardiovascular health.
What should be considered in bicuspid aorta?
It is essential not to miss annual cardiology check-ups. Blood pressure should be kept at an ideal level, heavy lifting and sudden exertion should be avoided. Inform your doctor before dental intervention or surgery; antibiotics may be recommended in case of infection.
Does bicuspid aorta cause pain?
Bicuspid valve alone usually does not cause pain. However, if severe stenosis or leakage develops in the valve, there may be pressure, tightness and pain in the chest with exertion. If these complaints are present, a cardiologist should be consulted immediately.
When is bicuspid aorta surgery?
The decision to operate is based on the severity of the stenosis or leak, the level of fatigue of the heart and whether the aorta is enlarged. Surgery is considered if the stenosis is severe, if the aortic diameter reaches 5.0-5.5 cm or if the heart starts to enlarge. Chest pain, shortness of breath and fainting are important signals for surgery.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.