In infants and children, a heart hole is a congenital opening in the walls between the atrial or ventricular chambers of the heart. The most common symptoms of this condition include rapid breathing, excessive sweating during feeding, rapid fatigue and failure to gain weight. Today, a hole in the heart is effectively managed with treatment methods planned depending on the type and size of the problem. Modern approaches range from regular follow-up to non-surgical closure through the groin to open-heart surgery with high success.
What is a Heart Hole in Babies and Children and How Does It Affect the Heart?
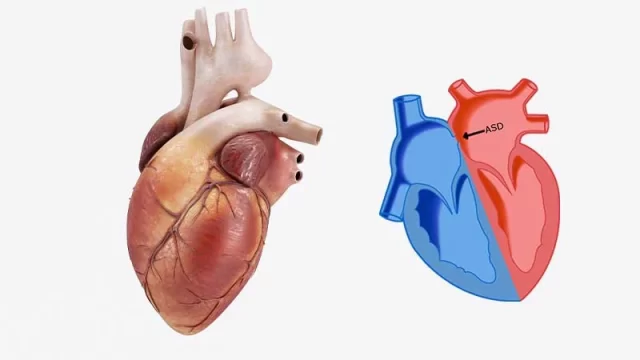
A hole in the heart in infants and children is simply a congenital opening in the walls separating the chambers of the heart. This causes the blood to follow an abnormal route through the heart and increases the workload of the heart.
To understand this better, let’s think about how our heart works. Our heart is like a house with four chambers: two upper floors (atria) and two lower floors (ventricles). The right side of this house collects “dirty” blood from the body, which is low in oxygen, and sends it to the lungs to be cleaned. The left side receives “clean” blood, which is enriched with oxygen in the lungs, and pumps it throughout the body. There are normally strong walls between these two sides and clean blood and dirty blood do not mix.
One or more openings in these walls (septum) is what we call a “hole in the heart”. Because the pressure on the left side of the heart is always higher than on the right side, some of the clean blood, instead of going to the body as it should, escapes through the hole back to the right side, where the dirty blood is. In medicine, we call this a “left-to-right shunt”.
The most important consequence of this abnormal blood flow is that the lungs receive much more blood than normal. While the lungs are trying to cope with this unexpected flood of blood, the heart, especially the right side of the heart, has to work harder and harder to pump this extra blood to the lungs. Over time, this overwork exhausts both the heart and the lungs and can have a negative impact on growth and development. The size and location of the hole are the main determinants of how severe this impact will be.
Why Do Heart Holes Occur in Babies and Children and Are There Risk Factors?
This is the question that parents ask most often and question themselves the most: “Why? Did we do something wrong?” I would like to answer this question in the clearest way possible: In most cases, the exact cause of the hole in the heart is unknown and beyond your control.
The heart is a miraculous organ that completes its formation while the baby is in the womb, in the first weeks of pregnancy, when many women are not even aware that they are pregnant. Starting from a simple tube structure, it folds, divides and walls into its final four-chambered form. Any small glitch in this complex construction process can cause the walls to fail to close and leave a hole. Therefore, it is very important not to wear yourself out with thoughts like “I wish I had done this” or “I wish I had not done that”.
However, it is known that some conditions may slightly increase the risk. These factors are:
- Down syndrome
- Turner syndrome
- Other genetic syndromes
- Congenital heart disease in the family (mother, father, sibling)
- Some maternal conditions during pregnancy can also affect the risk.
- Uncontrolled diabetes (diabetes)
- Having infections such as rubella
- Some medications used outside the doctor’s control (such as some epilepsy and acne medications)
- Alcohol and cigarette consumption
- Maternal obesity
So, let’s clarify the question “can a hole in the heart be acquired?”. These holes are congenital, meaning the baby is born with them. They are not caused by an accident or disease. However, sometimes the hole is so small that there are no symptoms in childhood and it is only detected in adulthood by chance or during a check-up for some other reason.
Which Types of Heart Holes are Most Common in Infants and Children?
although “heart hole” is a general term, there are different types of heart holes and the treatment plan depends on the type. The two main types we encounter most often are the following:
Atrial Septal Defect (ASD): This is a hole in the wall between the upper chambers (atria) of the heart. Symptoms usually appear at a later age. It has different subtypes.
Secundum ASD: It is the most common type and is usually most suitable for catheter closure (without surgery).
Primum ASD: It is close to the heart valves and is often accompanied by additional problems in the valves. The treatment is surgical.
Sinus Venosus ASD: It is close to where the great vessels enter the heart and its treatment again requires surgical intervention.
Ventricular Septal Defect (VSD): This is a hole in the wall between the lower chambers (ventricles) of the heart. It is the most common of all congenital heart defects. It is more likely to cause symptoms in babies than ASD. VSDs also have subtypes according to their different locations.
Perimembranous VSD: The most common type of VSD. It is located just below the aortic valve.
Muscular VSD: It is in the muscular part of the wall. There is a good chance that such holes will close spontaneously as the baby grows.
Outlet (Subarterial) VSD: Close to the outflow valves of the heart. Since these holes can cause the aortic valve to sag, they usually need to be closed surgically, even if they are small.
Inlet VSD: It is close to the inlet valves of the heart and is usually more common in children with Down syndrome.
Knowing the type of defect is vital both for predicting the course of the disease and for choosing the best treatment method (surgery, catheterization or just follow-up).
What Symptoms Does a Perforated Heart Cause in Babies and Children?
The symptoms of a heart hole depend entirely on the size and location of the hole and the child’s general health. A small hole can remain unnoticed for a lifetime, while a large hole can cause serious symptoms shortly after birth.
The symptoms of a heart hole in babies that parents should pay particular attention to are as follows:
- Difficulty breathing in and out or breathing much faster than normal
- Tired quickly during feeding (breastfeeding or bottle feeding)
- Intense sweating of the forehead or head during feeding
- Frequent cessation of feeding, crying, restlessness
- Inadequate weight gain compared to peers, growth retardation
- Pallor or bruising of the skin, especially when crying or sucking
- General weakness and reluctance to play
- Recurrent and difficult-to-heal lung infections (bronchitis, pneumonia)
In older children and adolescents, symptoms can often be milder:
- Tired more quickly than their peers when playing games or sports
- Panting during exertion
- Palpitations in the chest
- Chest pain (more rare)
If you observe one or more of these symptoms in your child, you should always discuss this with a pediatrician or directly with a pediatric cardiologist. Sometimes these symptoms can be confused with other simple conditions, but it is always safest to rule out an underlying heart problem.
How is a Heart Hole Diagnosed in Infants and Children?
The process of diagnosing a heart hole often means an anxious wait for the family. However, the steps in this process are fairly standardized and reliable. Usually the diagnosis starts with a suspicion and is followed by tests to confirm it.
Often the first clue is an innocent “murmur” that the pediatrician hears while listening to the child’s heart with a stethoscope during a routine check-up. A murmur is an abnormal sound made by blood flowing through a hole. However, it should be emphasized again that not every murmur heard in children is a sign of heart disease. so-called “innocent murmurs”, which are completely harmless, are also quite common.
When a murmur is heard or a hole in the heart is suspected, the child is referred to a pediatric cardiologist. The most important and standard methods used to confirm the diagnosis are the following.
Echocardiography (ECHO): This is a detailed ultrasound of the heart using sound waves, which is considered the “gold standard” for diagnosing heart holes. It is completely painless and harmless. ECHO allows us to clearly see where the hole is, its size, the number of holes, how dilated the heart chambers are, the condition of the valves and how much blood is passing through the hole.
Electrocardiogram (ECG): This simple test, which records the electrical activity of the heart, gives us valuable information about whether the heart chambers are enlarged or whether there is a rhythm disturbance.
Telecardiogram (Chest X-ray): It allows us to see the overall size and shape of the heart and whether there is increased blood flow to the lungs (whether the lungs are filling with blood).
Cardiac Catheterization and Angiography: This is an advanced method that we rarely use for diagnosis. It is usually performed in complex cases where ECHO is insufficient, when it is necessary to precisely measure lung pressure or when it is planned to close the hole with a catheter method in the same session. Through a vein in the groin, the heart is accessed and detailed measurements and imaging are performed.
What Complications Can Develop in Infants and Children If a Heart Hole is Not Treated?
“What if we wait to see if it closes on its own?” or “What are the risks if left untreated?” These are the most legitimate concerns of parents. Small holes that do not burden the heart usually do not cause any problems and many even close on their own over time. However, if left untreated, medium and large holes can lead to serious and irreversible problems over time. These conditions, which we can define as the harms of having a hole in the heart, are as follows.
Heart Failure: The heart muscle, which is constantly overworked, becomes tired over time and cannot effectively pump the blood the body needs. This is the main reason for feeding difficulties and lack of weight gain in infants.
Pulmonary Hypertension: The constant supply of blood to the lungs at high pressure and volume causes the walls of the pulmonary arteries to thicken and harden over time. This is an increase in pulmonary pressure to dangerous levels.
Eisenmenger Syndrome: This is the last and most dangerous stage of pulmonary hypertension. The damage to the lung vessels progresses so far that there is no going back. At this point, the blood flow in the heart is reversed (dirty blood mixes with clean blood) and the body turns blue (cyanosis). In a patient who has reached this stage, closing the hole is now life-threatening. Intervening at the right time is therefore critical to avoid reaching this point of no return.
Infective Endocarditis: A rare but very serious infection of the inner lining of the heart caused by the nesting of blood-borne microbes in areas with abnormal blood flow.
Arrhythmias (Arrhythmia): Heart chambers that enlarge and become unstructured due to excessive blood load can cause irregular heartbeats later in life.
Stroke (Paralysis): Especially in cases such as ASD, a stroke can occur when a small blood clot formed elsewhere in the body passes through the hole, reaches the brain and blocks the blood vessels.
What are the Current Treatment Methods for Heart Hole in Infants and Children?
There is no magic formula for treating a heart hole; treatment is completely individualized to the child and the characteristics of the hole. A team of a pediatric cardiologist and a cardiovascular surgeon will determine the best approach. General treatment approaches are as follows.
Monitoring (Wait and See Approach): This is the best approach for small holes (especially some types of VSD) that do not put a significant load on the heart and do not cause symptoms. The child is followed up at regular intervals with an ECHO to see if the hole closes spontaneously or if it enlarges.
Medication Medicines do not close the hole. However, they are used to reduce the workload of the heart, remove excess fluid from the body, and help the child breathe and gain weight more easily, especially in children who are preparing for surgery or interventional treatment, or who show signs of heart failure. This serves as a “bridge” to the actual treatment.
Nutrition Support: It is one of the most important steps of treatment, especially for babies who have difficulty gaining weight. Special high-calorie formula or enrichment of breast milk aims to strengthen the baby until the operation and to catch up with the growth curve.
Closing the hole (Interventional or Surgical Treatment): If the hole does not close spontaneously, is large, impedes the child’s growth or causes serious symptoms, it must be closed. There are two main modern methods for this: Catheter Method (Non-Surgical) and Open Heart Surgery.
When and How Is Heart Hole Surgery Performed in Babies and Children?
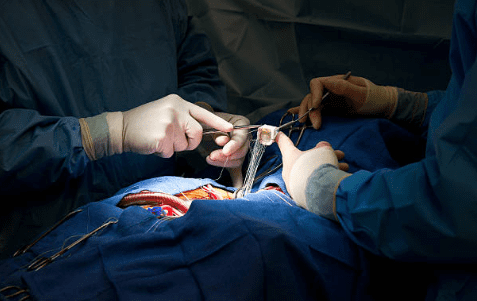
Open heart surgery is a safe and permanent solution for the treatment of heart defects that has been used with high success for many years. although the term “open heart surgery” can be frightening for families, today these operations are performed very safely in experienced centers.
The decision to operate is usually taken in the following cases:
- The hole is too big
- Persistence of heart failure symptoms despite medication
- Failure to gain weight and growth retardation despite adequate nutritional support
- Lung pressure starts to rise (risk of pulmonary hypertension)
- The type of hole carries a risk of damage to the aortic valve (such as outlet VSD)
The operation is performed under general anesthesia. The surgeon opens the sternum and accesses the heart. While the heart-lung machine temporarily takes over the function of the heart and lungs, the heart is stopped and the repair is carried out in a calm environment. The hole is closed either with simple sutures or, more commonly, with a patch made from the child’s own heart membrane (pericardium) or synthetic materials. Over time, this patch is covered with the body’s own tissue and becomes part of the heart. After the procedure is finished, the heart is restarted, the sternum is joined with special wires and the skin is closed. After surgery, the child is monitored in intensive care for a few days and can usually return home within a week.
Who is Suitable for Catheter Closure (Non-Surgical) for Heart Hole in Infants and Children?
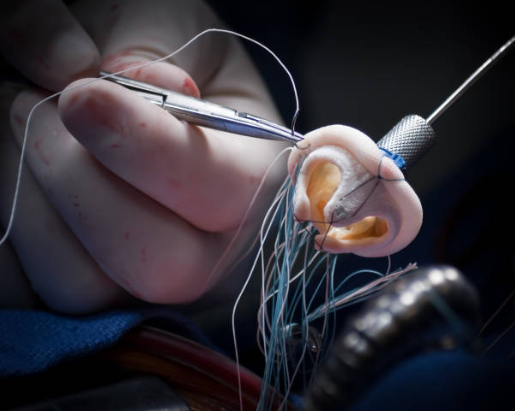
Thanks to advances in technology, we can now close many heart holes of suitable structure without the need for open-heart surgery, by entering through the groin. This is a modern method that is less traumatic and the healing process is much faster.
However, this method is not suitable for all holes. The hole must meet certain conditions to be closed with a catheter. This decision is made by the interventional cardiologist after a detailed ECHO and sometimes catheter angiography.
Conditions that are usually suitable for catheter closure include
Secundum type ASDs: This method is most commonly and successfully used for this type of ASD. The hole should not be too large and there should be an edge of tissue around it that is strong enough to hold the closure device.
Some muscular VSDs: Some VSDs in the muscular wall of the heart, which can be difficult to access surgically, can also be closed with this method.
Selected perimembranous VSDs: Some perimembranous VSDs with appropriate anatomical structure that do not pose a risk of damage to the heart’s conduction system and valves can also be closed with this method in experienced centers.
The procedure is performed under anesthesia in the catheterization laboratory. A thin tube (catheter) is inserted through a vein in the groin to the heart. Through this tube, a special umbrella-like closure device is inserted into the hole and the hole is closed. The hospital stay after the procedure is usually only one night and the child can return to normal life within a few days.
How Should Recovery and Home Care Be After Heart Hole Treatment in Babies and Children?
The recovery period after treatment, especially after open heart surgery, is a time when the family needs to be careful and attentive. Here are some important points to consider in this process.
For postoperative wound care:
- Keep the wound clean and dry.
- Dress as prescribed by your doctor.
- Avoid rubbing and scratching the wound.
- Be alert to signs of infection.
If you notice any of the following signs of infection, contact your doctor immediately:
- fever above 38°C
- Increased redness or swelling at the wound site
- Yellow, green or foul-smelling discharge from the wound site
- Opening of the wound edges
- Worsening of the child’s general condition, constant drowsiness
Things to consider about activity:
- Never lift the child by pulling under the arms for the first 6-8 weeks.
- Do not allow heavy lifting, pushing or pulling movements.
- Avoid activities such as cycling, running and jumping, where the child may be hit in the chest, until the doctor gives permission.
- Plan with your doctor the timing of his/her return to school and his/her participation in physical education classes.
General care recommendations:
- Give the medicines prescribed by your doctor on time and in the correct dosage.
- Make sure that the child receives adequate and balanced nutrition.
- Keep away from crowded environments and sick people to protect them from infections during the recovery period.
- Never miss scheduled check-up appointments.
It is normal for your child to be more moody, tearful or more fond of you than usual during this time. Giving her lots of love, patience and understanding will have a positive impact on her healing process, both physically and emotionally.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Prof. Dr. Yavuz Beşoğul » General » Heart Disease: Types, Causes, and SymptomsHeart diseases are [...]
Aug
How the Heart Works
Prof. Dr. Yavuz Beşoğul » General » How the Heart WorksThe heart functions as a [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Prof. Dr. Yavuz Beşoğul » General » How Many Hours Does Heart Valve Surgery Take?Heart [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Prof. Dr. Yavuz Beşoğul » Coronary Artery Bypass » How long does coronary artery bypass [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Prof. Dr. Yavuz Beşoğul » Kalp Kapak Hastalıkları » Kalp Kapak Değişimi Ameliyatı Nedir? Kalp [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Prof. Dr. Yavuz Beşoğul » General » Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki [...]
Aug
Life After Heart Valve Surgery
Prof. Dr. Yavuz Beşoğul » General » Life After Heart Valve SurgeryLife after heart valve [...]
Aug
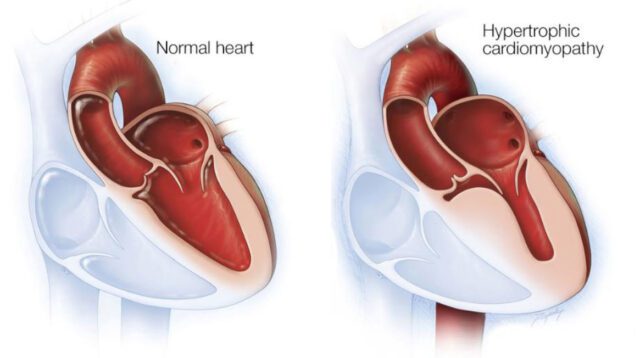
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Prof. Dr. Yavuz Beşoğul » General » Hypertrophic Cardiomyopathy: Symptoms & TreatmentHypertrophic cardiomyopathy is a [...]
Aug