Aortic valve surgery is a surgical procedure to treat serious disease of the aortic valve, the heart’s main pumping valve. It is usually performed in cases of advanced aortic valve stenosis or insufficiency to relieve the load on the heart and restore healthy blood circulation to the body. The surgery involves repairing the damaged valve (aortic valve repair) or replacing the dysfunctional valve with a completely new prosthetic valve. Today, these operations can be successfully performed with modern minimally invasive techniques such as closed aortic valve surgery as well as classical open surgery, allowing patients to recover faster.
| Category | Information |
| Application Area | The aortic valve in the left ventricular outflow of the heart |
| Indications | Aortic stenosis, aortic insufficiency, valve infection (endocarditis), valve degeneration |
| Types of Surgery | Valve repair or replacement through the armpit with closed heart or minimally invasive method. |
| Cover Types | Mechanical valve, bioprosthetic valve (from porcine or bovine tissue), human donor valve (homograft) |
| Surgery Process | 2-4 hours |
| Regeneration Process | Average 3-5 days in hospital; full recovery 10 days. |
| Success Rate | High (above) in experienced centers |
| Common Risks | Bleeding, infection, arrhythmias, risk of embolism, valve-related problems |
| Long Term Follow-up | Lifelong use of anticoagulants in mechanical valves, regular control in bioprostheses |
| Alternatives | TAVI method in patients of advanced age or at high risk of surgery |
| Prognosis | If done in time before the onset of heart failure, life expectancy is very long |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
When is surgery needed for aortic valve disease?
The decision to operate for aortic valve disease is directly related to how much strain the disease puts on your heart and how it affects your daily life. Our main goal here is to intervene before irreversible damage to your heart occurs. The timing of surgery usually depends on two main factors. These are the presence of symptoms and concrete evidence that the heart is getting tired.
If you have severe aortic valve disease and you start to experience some difficulties in your daily life, this is a sign that your heart is now sounding the alarm. When these alarm symptoms occur, it is vital to take immediate action, because left untreated, this condition can seriously reduce life expectancy. Here are the main symptoms to look out for:
- Shortness of breath (especially with exertion or at night)
- Chest pain (like a feeling of pressure)
- Head rotation
- Sudden fainting attacks
- Rapid fatigue and weakness
The presence of any of these symptoms, especially if severe aortic stenosis or insufficiency has been diagnosed, constitutes the strongest indication for surgery. All international medical guidelines strongly recommend aortic valve replacement (AVR) surgery in this situation.
How is the decision for aortic valve surgery made in asymptomatic patients?
Sometimes our patients come to us saying “I have no complaints, I feel fine”. But this does not always mean that the heart is also fine. The heart is a sacrificial organ that tries to manage the situation until the last moment. Therefore, even if you have no symptoms, in some cases we may recommend preventive surgery. Our aim is to nip the problem in the bud before the heart quietly tires and suffers permanent damage. There are some important circumstances that we take into account when making this decision:
Difficulty in Pumping the Heart: One of the most important objective indicators is the contractility of the heart. The “Ejection Fraction” (EF) value, which we measure with echocardiography (ECHO), shows how much blood the heart pumps into the body with each beat. In a healthy heart, we expect this ratio to be ` or above. If it has fallen below P without any symptoms, this is tangible evidence that the heart is now beginning to weaken and the danger bells are ringing. Some current guidelines even recommend considering a drop in this value to the U-60 range as a warning signal to consider surgery, especially in younger patients.
Abnormalities on Exertional Testing: Sometimes our patients mask their symptoms by slowing down their daily activities without realizing it. In such cases, a stress test, which we perform by walking you on a treadmill, can reveal hidden truths. If you experience shortness of breath or a sudden drop in blood pressure (blood pressure) during the test that you had not noticed before, this indicates that your valve is not able to meet the body’s increased blood demand, which may indicate the need for surgery.
Very High Risk Findings: In some cases, the valve stenosis is so advanced that it is classified as “very serious” or “critical”. Findings on echocardiography, such as a blood flow rate of more than 5 meters per second, or a rise in blood tests of a heart failure marker called BNP more than three times the normal level, indicate a very high risk of sudden deterioration in the near future. In such high-risk patients, it is often a safer strategy to intervene without waiting for symptoms to appear.
Necessity to Have Another Heart Surgery: If a patient needs another open heart surgery, such as a coronary bypass, and also has a moderate aortic valve problem, we usually do both at the same time. That is, we perform the bypass and repair or replace the aortic valve in the same surgery session. This approach protects the patient from the risk of having a second major heart surgery in later years.
What is a Heart Team and why is it important for aortic valve surgery?
In the past, decisions about the treatment of aortic valve disease were usually made by a single physician. However, in today’s modern medicine, this has completely changed. A board of doctors from different specialties, which we now call a “Heart Team” or “Heart Council”, jointly makes the best treatment decision for each patient. This is the gold standard of patient-centered treatment.
The Heart Team tries to see the big picture by putting the patient’s condition together like pieces of a puzzle. This team includes specialists who play different roles. These experts are as follows:
- Cardiovascular Surgeon
- Interventional Cardiologist
- Clinical Cardiologist (follow-up doctor)
- Cardiac Imaging Specialist (ECHO and tomography interpreter)
- Cardiac Anesthesiologist
Depending on the patient’s condition, this core team may also include heart failure specialists, geriatricians and intensive care physicians. The aim of the team is to discuss all the patient’s medical data, films, test results, risk scores, age, lifestyle and, most importantly, the patient’s own values, expectations and preferences. As a result of this detailed evaluation, the most accurate answer to the question “What is the best treatment option for this patient?” is sought. Open surgery, closed surgery, TAVI, mechanical valve or biological valve? The advantages and disadvantages of all these options are discussed on a patient-specific basis and the safest and most effective roadmap is drawn.
What evaluations are performed before aortic valve surgery?
In order to plan the most appropriate and safest treatment for you, we need to carry out a series of detailed pre-operative examinations. These examinations not only provide a clear picture of the current condition of your heart and blood vessels, but also help us understand the risks of the procedure. There are key assessments made during this process.
Echocardiography (ECHO): Also known as an ultrasound of the heart, this test is the basis for diagnosis and follow-up. It gives us a clear picture of how much your valve constricts or contracts, the force of contraction of your heart (EF value) and the size of its chambers.
Computed Tomography (CT) Angiography: CT is indispensable, especially when TAVI is an option. This three-dimensional film, taken in conjunction with an ECG, measures the diameter and area of the aortic annulus, where the new valve will be placed, to within tenths of a millimeter. This is critical information for selecting the right valve size and minimizing the risk of valve edge leakage. It also provides us with all the anatomical details, from the structure of the muscular vessels to be used for TAVI to the location of your coronary vessels, like a “road map”.
Coronary Angiography: It is performed to check for obstruction in the coronary vessels supplying the heart, especially in patients over 45 years of age or those with risk factors for heart disease. If a significant stenosis is detected, it is planned to solve the problem by bypassing this vessel during valve surgery.
Risk Scoring: We use internationally recognized risk calculation systems such as STS or EuroSCORE II to objectively assess your risk of surgery. These systems use information such as your age, gender, comorbidities and the type of surgery planned to statistically estimate the possible risks over a 30-day period. These scores help us classify you as low, intermediate or high risk, and this classification guides us when choosing the treatment method (surgery vs. TAVI). However, it is important to remember that these scores are not everything; they are only a guide. The Heart Team makes the final decision, taking into account all this information and your general condition.
How is aortic valve replacement surgery performed?
Aortic valve replacement, i.e. the removal of the dysfunctional valve and its replacement with a new prosthetic valve, has been the most reliable method of treatment for this disease for many years. This surgery can be performed with the traditional open method or with modern minimally invasive, or “closed” techniques, which are more preferred today.
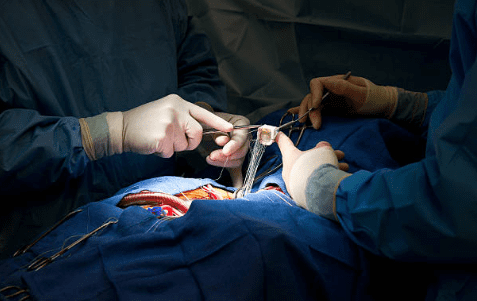
Classical Open Method: This is the most widely known method. Under general anesthesia, the chest bone (the sternum or the faith board) is opened through a vertical incision in the midline. During the operation, the heart-lung machine temporarily takes over your blood circulation and breathing. The heart is stopped with a special inhalation, allowing the surgeon to work safely in a bloodless and immobilized environment. The surgeon meticulously cleans your own valve, which has become frayed and deteriorated, and replaces it with your new prosthetic valve (mechanical or biological) with sturdy sutures. At the end of the procedure, the heart is restarted and the chest bone is closed with special wires. An aortic valve replacement surgery usually takes 3 to 5 hours and the average hospital stay is 5-7 days.
Minimally Invasive (Closed) Methods: Developed to reduce surgical trauma, accelerate recovery and achieve better cosmetic results, these techniques have become standardized, especially in the hands of experienced surgeons. when it comes to “closed aortic valve surgery”, there are two most common methods that come to mind:
Underarm Aortic Valve Surgery: In this technique, the chest bone is not cut at all. Instead, the heart is accessed through a small incision of about 4-5 cm on the side of the right chest, close to the axillary line, between the ribs. Because this method preserves the integrity of the breast bone, it significantly reduces postoperative pain, allowing patients to get up faster and return to their daily lives much sooner.
Mini Sternotomy: In this approach, only the upper part of the chest bone is cut in a “J” or “T” shape, about 6-10 cm, not the entire chest bone. This allows for a more stable recovery, preserving a large part of the bone while providing safe access to the heart.
These closed methods have many proven advantages, including reduced blood requirements, a shorter intensive care period and earlier discharge from hospital.
What is the TAVI method and who is it suitable for?
TAVI (Transcatheter Aortic Valve Implantation) is not an alternative to open heart surgery. It is a procedure only for elderly patients who are at very high risk of having heart surgery. In this procedure, the chest cage is not opened. Instead, a catheter (a thin tube) is inserted through an artery, usually in the groin. The new valve, which has been compressed, is guided through this catheter to the heart and inserted into the diseased aortic valve, where it is enlarged. The old lid acts as a kind of scaffolding, while the new lid starts to work inside it.
Should a mechanical or biological cover be preferred?
When the decision is made to have a surgical valve replacement, one of the most important choices for you and for us is the type of valve to be fitted. This choice is fundamentally based on the balance between resilience and the use of blood thinners and directly affects the rest of your life.
Mechanical Closures: These are ticking clockwork lids made of highly durable materials such as pyrolytic carbon. Its main features are as follows:
- Lifetime durability
- Very low risk of structural deterioration
- Obligation to use blood thinners (Coumadin/warfarin) for life
- Constant risk of bleeding
- Need for follow-up with regular blood test (INR)
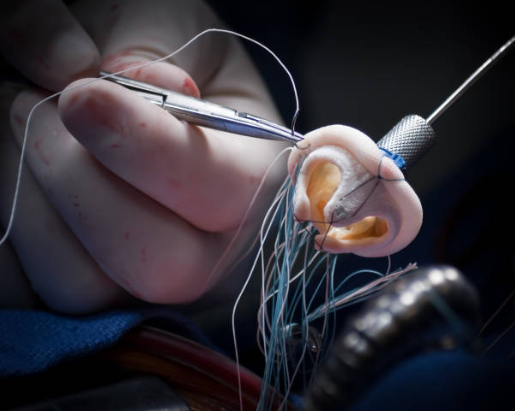
Biological Valves (Tissue Valves): These valves, usually made from the membrane of the bovine or porcine heart (pericardium), are closer to human tissue. They too have their own characteristics:
- No need for blood thinners (usually except for the first 3 months)
- Providing more natural blood flow
- Limited durability (average 15-20 years)
- Structural deterioration over time, requiring a second operation
So, how do we make the selection?
In general, in patients under 70 years of age, we generally prefer mechanical valves because of their lifelong durability. in patients over 70 years of age, biological valves are a better option to eliminate the risk of bleeding and because the valve is more likely to last over life expectancy. with our patients in the “gray zone” between 70 and 75 years of age, we make this decision together. We will discuss in detail your lifestyle, your occupation, how you feel about the idea of using a blood thinner and how you feel about the possibility of having a second operation in the future, and make the best decision for you
Is aortic valve repair possible?
It is not always necessary to remove and replace the valve. In some lucky groups of patients, especially those with aortic valve insufficiency and whose valve leaflets have not yet become too heavily scratched and hardened, it is possible to repair the patient’s own valve. Aortic valve repair is a very elegant and effective method that saves you from all the potential problems that prosthetic valves can bring.
The major advantage of repair is that it preserves your body’s own tissue. This eliminates the need to use blood thinners and minimizes the risk of clots and infection. The repair is particularly successful if the cause of valve failure is prolapse of the valves (prolapse) or an enlargement of the root of the aortic artery (aortic aneurysm). Repair may also be a suitable option in patients with bicuspid aortic valves, which are often congenitally bifurcated. In this operation, the surgeon reshapes the sagging valves with special suturing techniques and, if the aortic vessel is dilated, replaces the vessel with special techniques such as “David” or “Yacoub” while preserving the patient’s own intact valve. In experienced hands, aortic aneurysm and valve surgery can be combined to achieve excellent long-term results.
What is the Ross Procedure and what advantages does it offer?
The Ross procedure is a unique surgery, developed especially for young and middle-aged patients, which can be considered the pinnacle of biological solutions. In this surgery, the patient’s diseased aortic valve is removed and replaced with the patient’s own healthy pulmonary artery valve (pulmonary valve). This is a kind of autotransplantation (transplantation of the patient’s own tissue). The removed pulmonary valve is replaced with a human valve (homograft) from a donor.
The basic rationale for this seemingly complex procedure is to place a living, growing and self-repairing valve in the aortic position of the heart, where it works the hardest and is subjected to the highest pressure. The major advantages of the Ross procedure are the following:
- Does not require blood thinners.
- Its growth potential makes it ideal for pediatric patients.
- The blood flow is so natural that no prosthetic valve can mimic it.
- Long-term studies have shown that the life expectancy of patients who undergo this surgery is almost the same as healthy people of their own age.
- Although technically challenging, with the right patient selection and an experienced surgeon, the results are superior to all other valve replacement options.
What kind of treatment is the Ozaki Procedure (AVNeo)?
The Ozaki procedure is a technique to “custom-build” a new aortic valve using the patient’s own tissue. In this innovative method, the patient’s diseased aortic valves are completely removed. A piece of the patient’s own heart membrane (pericardium) is then made more durable with a special solution. Using special measuring instruments, the surgeon designs three new valves to fit the patient’s aortic root and meticulously hand-sews pieces of this heart membrane to the aortic annulus, creating a new valve that is all your own.
The basic philosophy of this method is to construct a valve that best fits the natural anatomy without introducing any foreign material into the body. This eliminates the need to use a blood irrigator. It is a very promising alternative, especially for young patients who are not amenable to standard repair or who do not want a mechanical valve, and the mid-term outcomes have been very successful.
Is it necessary to have aortic valve surgery again for an old biological valve?
The biggest handicap of biological valves is that they wear out over time. In this case, a second operation becomes unavoidable. In the past, this meant a second open heart surgery, the risk of which was higher than the first operation. Today, however, we have a much more comfortable option, especially for high-risk patients: Valve-in-Valve TAVI (Valve-in-Valve TAVI).
In this method, the chest cage is not reopened. Instead, as with TAVI, a new TAVI valve is inserted, usually through the muscle, into the old surgical valve that has worn out. This uses the old valve as a scaffold, allowing the new valve to operate within it. This less invasive approach reduces the length of hospital stay and speeds up recovery tremendously. However, it should be noted that the process requires careful planning according to the type and size of the old lid.
What complications can occur after aortic valve surgery?
As with any medical intervention, aortic valve interventions have potential risks. Surgical (open or closed) and TAVI methods have different risk profiles, and these differences are important considerations when making treatment decisions. The main conditions that come to mind when complications after aortic valve surgery are mentioned are as follows:
- The risks associated with surgery (SAVR) are usually related to the operation itself.
- Major bleeding
- New-onset atrial fibrillation (a type of arrhythmia)
- Acute kidney injury
- Wound site infection
- The risks associated with TAVI are more specific to the device and method used.
- The need for permanent pacemaker implantation
- Leakage from the edge of the cover (paravalvular scalp)
- Complications in the intervening vessels (usually the groin)
- Stroke (stroke)
In general, the risk of death from aortic valve surgery is quite low thanks to today’s technology and experienced teams. For a low-risk patient, this rate is usually around 1-2%. However, it is important to recognize the risks associated with each method and to strategize accordingly.
How long does a replaced aortic valve last?
This is the most critical question, especially for our younger patients. The durability of the fitted closure directly affects your long-term quality of life.
Surgical Bioprosthetic Valves: We have decades of experience with these valves. On average, the rate of intact functioning of these valves after 15 years is above . However, the younger the age of the patient, the faster the rate at which the valve tears.
TAVI Valves: The 5- to 8-year outcomes of current TAVI valves have demonstrated similar or sometimes even better durability than surgical valves. However, since TAVI technology is still new, we do not yet have clear data on the performance of these valves after 15-20 years. It is the most important research topic in this field.
How does life continue after aortic valve replacement?
A successful surgery is just the beginning of the story. Staying healthy for the long term requires effort on your part. Life after aortic valve replacement requires attention to some important points.
Recovery Process: After open surgery, it takes 6-8 weeks for the jugular bone to fuse and it may take 2-3 months to regain your energy. During this period, you need to follow some activity restrictions. Recovery after TAVI is much faster; our patients are usually discharged within a few days and return to their normal lives within a week.
Lifestyle Tips: Regardless of the method of treatment, it is very important to make some lifestyle changes to protect your heart.
- Quit smoking completely
- Reducing salt consumption
- Avoiding saturated fat and processed foods
- Adopting a Mediterranean-type diet (plenty of vegetables, fruits, fish, olive oil)
- Regularly doing the exercises prescribed by your doctor
Cardiac Rehabilitation: We strongly recommend that you participate in a cardiac rehabilitation program after surgery. These programs give you the habit of exercising in a safe environment and offer professional support for a healthy lifestyle.
What is the follow-up process after aortic valve surgery?
After aortic valve surgery or TAVI, all our patients need regular follow-up throughout life. The purpose of this follow-up is to check how well your new door is working, to detect possible wear and tear at a very early stage and to manage any long-term problems that may arise.
Our most important tool in follow-up is echocardiography (ECHO). We perform a baseline ECHO on all our patients who receive a bioprosthetic valve before discharge. This records the performance of the valve on the first day, providing a reference point for future comparisons. Subsequently, as recommended by international guidelines, we perform regular checks with ECHO at 1 month, 1 year and every year thereafter. Thanks to these annual checks, we can catch even the slightest deterioration of the valve before you feel any discomfort and, if necessary, intervene in a planned manner before an emergency occurs.
What are the prices for aortic valve surgery?
One of the most common concerns of our patients is, of course, the cost of the treatment. it is impossible to give a clear figure on “aortic valve surgery prices” because the cost varies greatly from person to person and from case to case. The main factors affecting the price are:
- Type of procedure performed (classic open surgery, underarm closed aortic valve surgery TAVI)
- Type of closure used (mechanical closure, biological closure, seamless closure)
- Hospital where the surgery was performed (private, university, state)
- Presence of additional procedures (e.g. simultaneous bypass surgery)
- Coverage rates of the Social Security Institution and private health insurance
Can a disability report be obtained after aortic valve surgery?
Whether or not you can get a disability report for aortic valve surgery depends entirely on your functional status after surgery. If your surgery was successful, your heart’s contractile force (EF) has returned to normal and your effort capacity has increased significantly, there is usually no disability. This is the purpose of the surgery.
However, if you have undergone surgery with advanced heart failure and the heart’s pumping power remains low despite the surgery, if you have severe rhythm disturbances or if you continue to have symptoms that severely limit your daily life activities, then after a detailed assessment by a Health Board, it may be possible to obtain a disability report with a certain percentage of disability according to the relevant legal regulations. This decision is based entirely on an objective assessment of your personal health.
Frequently Asked Questions
When is aortic valve surgery necessary?
Aortic valve surgery is necessary when the aortic valve, which you can think of as the main door to your heart, is severely narrowed (aortic stenosis) or incompletely closed (aortic insufficiency). Narrowing of the valve causes the heart to work harder and incomplete closure causes blood to back up. If you suffer from shortness of breath, chest pain, fainting and medication is not enough, surgery to improve your quality of life and protect your heart may become unavoidable.
How long is the recovery period after aortic valve surgery?
Full recovery after underarm aortic valve surgery usually takes 2-4 weeks. You may feel tired in the first days, this is very normal. If you have a desk job, you can usually return to work after 3-4 weeks. It is also recommended to wait 2-4 weeks to drive. Everyone’s recovery process is different; the important thing is that you listen to yourself and do not miss your doctor’s visits. Give yourself time to regain your former strength.
Should mechanical or biological valve be preferred for aortic valve replacement?
This decision is made together, based entirely on your lifestyle, age and general health. Mechanical valves last a very long time, but require the use of a blood thinner for life. Biological valves, on the other hand, usually last 15-20 years and are usually suitable for patients over 65 or those who cannot use blood thinners. Together we will decide which option is right for you, prioritizing both your safety and quality of life.
How long should I stay in hospital after aortic valve surgery?
After surgery, you will usually stay in intensive care for 1-2 days, followed by 4-5 days on the ward. During this time, our medical team will follow you closely and provide support with breathing exercises and wound care. If all goes well, the aim is for you to be discharged in 5-7 days in total. We are here to help you get back to your old life in no time!
Is aortic valve surgery risky and what are the possible complications?
As with any major surgery, aortic valve surgery has some risks, but today these risks have been greatly reduced (around 1-5%) thanks to minimally invasive techniques. Possible risks include bleeding, infection, stroke and arrhythmias. We minimize the risks with detailed pre-operative evaluations. Remember, the risk of not having surgery is usually higher than the risk of having surgery. Our goal is to bring you back to health safely!
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Heart diseases are conditions that impair the structure and function of the heart, leading to [...]
Aug
How the Heart Works
The heart functions as a muscular pump that circulates blood throughout the body. It consists [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Heart valve surgery duration varies depending on the complexity of the case and the valve [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Coronary bypass surgery duration depends on the number of blocked arteries and patient-specific factors. On [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Kalp kapakçığı değişimi, kapakların ileri derecede daralması (stenoz) veya yetersiz kapanması (yetmezlik) durumlarında, onarımın mümkün [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Kalp kapakçığı tamiri, mevcut kapağın korunarak yapısal bozukluklarının düzeltilmesi işlemidir. Kapak yaprakçıkları, kordonları veya halka [...]
Aug
Life After Heart Valve Surgery
Life after heart valve surgery involves a structured recovery period, with gradual improvement in physical [...]
Aug
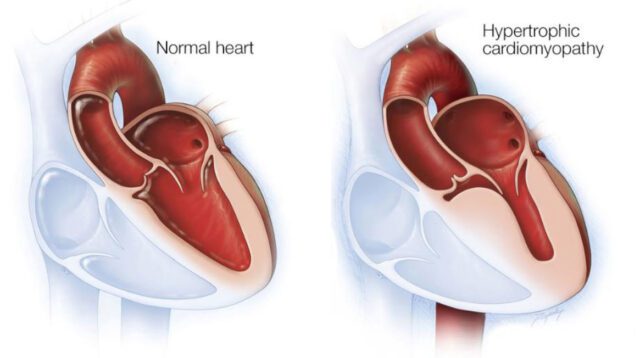
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Hypertrophic cardiomyopathy is a genetic heart disease characterized by abnormal thickening of the heart muscle, [...]
Aug