| Medical Name | Aortic Stenosis (Aortic Valve Stenosis) |
| Type | Valve disease |
| Affected System | Cardiovascular system |
| Causes | Degenerative (age-related calcification), congenital bicuspid aortic valve, rheumatic fever |
| Symptoms | Chest pain, shortness of breath on exertion, syncope, fatigue, signs of heart failure in advanced cases |
| Diagnostic Methods | Transthoracic echocardiography (main diagnostic tool), ECG, CT/MR, cardiac catheterization (when necessary) |
| Treatment Methods | Follow-up in mild cases; surgical valve repair or replacement (AVR) in severe cases |
| Complications | Left ventricular hypertrophy, heart failure, arrhythmia, sudden cardiac death |
| Monitoring | Regular ECHO follow-up, referral to surgery according to symptom development and valve opening measurement, control of risk factors |
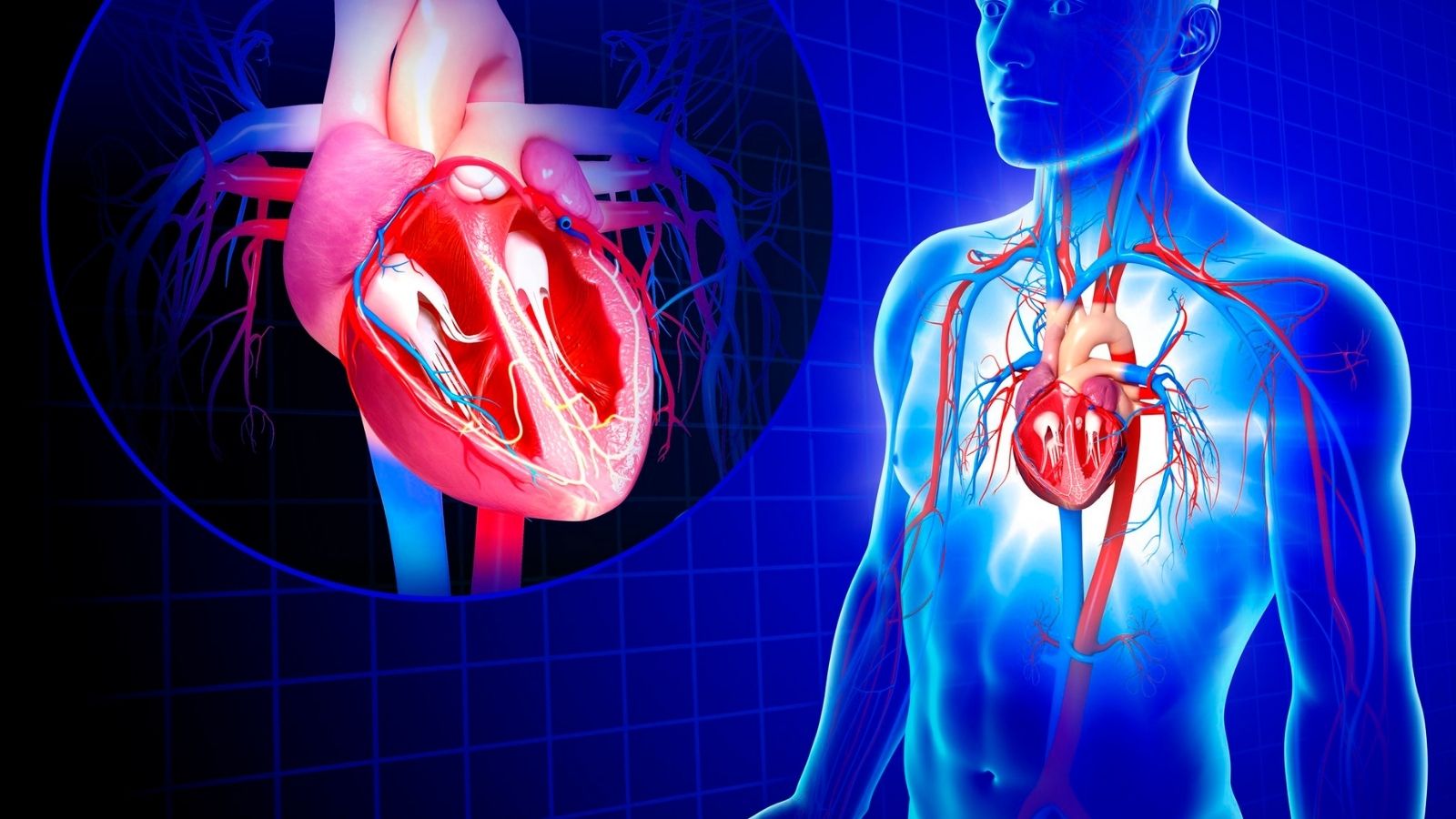
How the Heart Works and What is Aortic Valve Stenosis?
How Does Aortic Valve Stenosis Disrupt Heart Functioning?
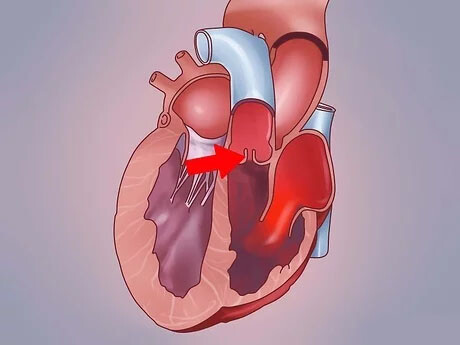
When aortic valve stenosis develops, the heart becomes like a pump trying to push water from a dam in order to push blood through the narrowed valve. In order to meet the body’s blood demand, the left ventricle of the heart has to create a much higher pressure than normal. This can be likened to a garden hose with a narrower and narrower end; as the flow of water becomes more difficult, the pressure inside the hose increases dangerously. The heart develops a defense mechanism to protect itself against this ever-increasing pressure and load. To cope with this increased workload, the muscle wall of the left ventricle thickens and strengthens over time. Just as the muscles of a weight-training athlete develop, the heart muscle increases in volume (hypertrophy) to cope with this demanding task. This allows the heart to function without interruption for a while and the disease can progress insidiously for years without symptoms. However, this compensation mechanism comes at a cost. On the one hand, thickening heart muscle increases pumping power, but on the other hand it reduces the internal volume of the heart chamber and reduces the heart’s capacity to fill with blood. More importantly, the thickened muscle becomes stiff over time and cannot relax as flexibly as before. After a while, the heart’s compensatory efforts are exhausted. Constantly overworked, stiffened and undernourished, the heart muscle tires and eventually begins to weaken. At this point, the heart’s pumping power (ejection fraction) decreases. The inability of the heart to pump blood forward effectively causes blood to pool backwards, in the lungs. This leads to the classic symptoms of heart failure, such as shortness of breath, extreme fatigue and swelling of the legs, which severely impair the patient’s quality of life.What Causes the Development of Aortic Valve Stenosis?
Aortic valve stenosis is usually caused by three main causes. Knowing these causes gives us important clues about who may develop the disease and when. The main causes of aortic valve stenosis are:- Age-related calcification (Degenerative calcification)
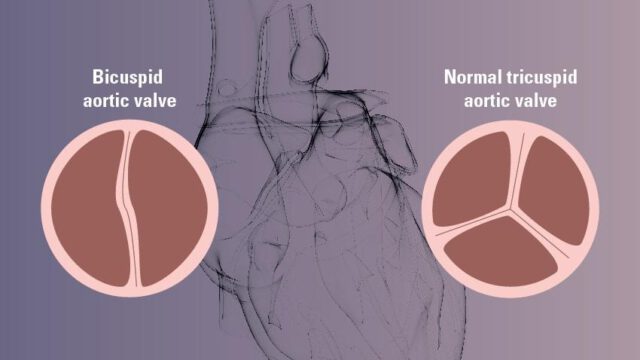
- Congenital valve structure disorders (congenital defects)
- Previous rheumatic fever
Who is at Risk for Aortic Valve Stenosis?
Some people are more prone to aortic valve stenosis because of their lifestyle or genetic heritage. Risk factors are divided into two main groups: modifiable and non-modifiable. Non-modifiable Risk Factors:- Advanced Age: Aging is the most important risk factor as it is a process in which valve calcification naturally increases.
- Male Gender: Aortic stenosis, especially the type due to congenital bicuspid aortic valve, is more common in men than in women.
- Congenital Valve Abnormalities: Structural defects present at birth, such as a bicuspid aortic valve, significantly increase the risk.
- High Blood Pressure (Hypertension): Increases stress on the heart valves and accelerates the calcification process.
- High Cholesterol (Dyslipidemia): Disrupts the valve structure with mechanisms similar to arteriosclerosis.
- Diabetes (Diabetes): High blood sugar triggers inflammation and calcification in valve tissue.
- Smoking: Increases the risk of calcification by disrupting the vascular structure.
- Chronic Kidney Disease: Calcium and phosphate imbalance in the body accelerates valve calcification.
- Previous Infections: A history of rheumatic fever or infective endocarditis can leave permanent damage to the valves.
- Receiving Radiation Therapy to the Chest: Radiotherapy to the chest, especially for the treatment of cancers such as lymphoma, can lead to hardening and calcification of the valves years later. Controlling these factors is as important for valve health as it is for the treatment of cardiovascular calcification.
What are the Warning Signs of Aortic Valve Stenosis?
Aortic valve stenosis is an insidious disease that can progress asymptomatically for many years. The heart can compensate for the increased workload for a long time. However, as the disease progresses and aortic stenosis becomes more severe, the heart’s compensatory mechanisms begin to struggle and the first symptoms usually appear during physical exertion when the body’s oxygen demand increases. These symptoms indicate that the disease has reached a stage that requires treatment. Early Symptoms: These symptoms are usually mild and may be seen by patients as a natural part of aging, which can delay diagnosis:- Tired more quickly than usual
- Gasping for breath, especially when climbing stairs or hills
- Decreased overall physical activity capacity
- Feeling of pressure, tightness or pain in the chest (angina)
- Dizziness, blackouts or fainting (syncope)
- Severe shortness of breath when lying flat or waking up at night
- A feeling that the heart beats fast, irregularly or very strongly (palpitations)
- Swelling in the ankles and legs (edema)
What Are the Classic Triple Signs of Advanced Aortic Valve Stenosis?
The appearance of three main symptoms in the course of advanced aortic valve stenosis indicates that the disease has now reached a critical point and is life-threatening. These three symptoms are the alarm that the heart’s compensatory mechanisms are completely exhausted and can no longer meet the body’s basic needs. The presence of these symptoms indicates a much more serious condition than milder conditions such as the symptoms of grade 1 aortic insufficiency. These are the classic three symptoms:- Chest Pain (Angina): This occurs when the heart muscle, which has thickened and needs more oxygen, does not receive enough oxygen due to insufficient blood flow through the narrowed valve. If the valve is not replaced after the onset of this symptom, life expectancy is reduced to about 5 years.
- Fainting (Syncope): Usually occurs during exertion, when the heart is unable to meet the body’s increased blood demand due to a narrowed valve, resulting in a momentary decrease in blood flow to the brain. When this symptom develops, if left untreated, life expectancy decreases to approximately 3 years.
- Shortness of breath (heart failure): The most serious symptom of the triad. It occurs when the weakened heart is unable to pump blood forward and it pools in the lungs. Once symptoms of heart failure begin, the average life expectancy drops to just 2 years, or even less.
How is Aortic Valve Stenosis Diagnosed?
Aortic valve stenosis is diagnosed by listening to the patient’s complaints, performing a detailed physical examination and then using modern imaging methods. The first suspicion is usually aroused by the typical “murmur” heard when listening to the heart with a stethoscope during a medical examination for another reason. This murmur is the sound of the turbulent flow of blood through the narrowed valve. However, hearing the murmur is only a suspicion and additional tests are needed to confirm the diagnosis. Echocardiography (ECHO) is the most important of these tests. Echocardiography, an ultrasound of the heart, is the gold standard for diagnosing aortic stenosis. This painless and radiation-free test uses sound waves to provide a clear picture of the structure and function of the heart and valves, the severity of the stenosis and how the heart adapts to this condition. ECHO provides the following critical information:- Details of the cover structure (number of leaflets, thickness, degree of calcification)
- Hemodynamic measurements that determine the severity of the stenosis (blood flow velocity, pressure difference)
- Area of the valve opening (Aortic valve area)
- The pumping power of the heart (ejection fraction) and the thickness of the muscle wall
Can Aortic Valve Stenosis be Treated with Medication?
This is one of the most common questions patients ask. Unfortunately, there is no proven drug treatment that can correct, reverse or stop the progression of aortic valve stenosis. The basis of the problem is mechanical, i.e. the physical constriction and calcification of the valves. Therefore, no pill can solve this calcification or widen the narrowed doorway. However, this does not mean that medicines are not used at all. Drug treatment focuses on managing the problems caused by the disease, rather than solving the main problem with the valve. The aim is to relax the patient, reduce the workload on the heart and prepare the patient for the final treatment – valve replacement – in a better condition. Medicines used for this purpose are:- Diuretics (diuretics), which relieve shortness of breath by removing excess fluid from the body.
- Medicines that control high blood pressure and can reduce chest pain by slowing the heart rate.
- Other supportive medicines that reduce the burden on the heart when heart failure develops.
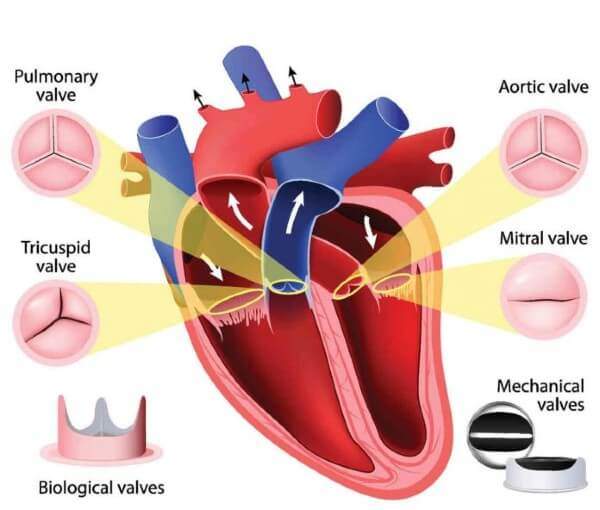
Which Treatment Methods Are Used in Severe Aortic Valve Stenosis?
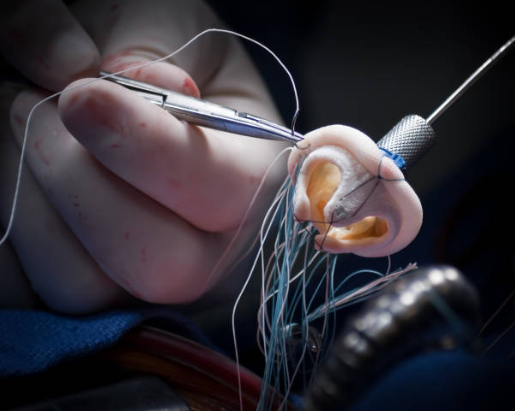
The only effective treatment for symptomatic severe aortic stenosis is to remove the diseased valve and replace it with a new prosthetic valve. Today, there are two main modern methods for this procedure: Surgical Aortic Valve Replacement (SAVR) and Transcatheter Aortic Valve Replacement (TAVR). Which method to choose is jointly decided by a “Heart Team” consisting of an interventional cardiologist and a cardiac surgeon, based on the patient’s age, general health status, surgical risk and anatomical features.- Surgical Aortic Valve Replacement (SAVR):
- Transcatheter Aortic Valve Replacement (TAVR):
What is the Importance of Lifestyle Changes in the Treatment of Aortic Valve Stenosis?
Although there is no lifestyle change that will directly stop the progression of aortic valve stenosis, it is extremely important to take certain steps to maintain overall cardiovascular health, reduce the workload on the heart and minimize the risk of complications. Recommendations to Support Heart Health:- Reduce Salt Consumption: It keeps fluid accumulation in the body and blood pressure under control.
- Avoid Saturated and Trans Fats: Protects vascular health by regulating cholesterol levels.
- Limit Processed Foods: Opt for fresh and natural foods.
- Quit Smoking: It is one of the most harmful habits for the heart and blood vessels.
- Maintain Ideal Weight: Being overweight directly increases the burden the heart has to carry.
- Check Your Activity Level with Your Doctor: Those with mild stenosis can do most activities, while those with severe stenosis may need to avoid heavy and competitive sports.
- Pay Attention to Oral and Dental Hygiene: Gum infections can lead to a serious valve infection called “infective endocarditis”, where bacteria can enter the bloodstream and settle on damaged heart valves. Regular dental check-ups are therefore a must.
What kind of a healing process awaits patients after aortic valve replacement?
Recovery after aortic valve replacement varies significantly depending on the method used (SAVR or TAVR). Recovery after SAVR (Open Heart Surgery): This process is longer and more gradual. Patients are usually admitted to the ward after 1-2 days in intensive care and stay in hospital for about 1 week in total. The most critical period after returning home is the 6-8 weeks needed for the sternum to fuse. During this period, patients are asked to- lifting no more than 5 kilograms
- Avoiding movements that strain the chest muscles such as pushing and pulling
- Not driving for about 6 weeks
- Regularly performing breathing and walking exercises recommended by physiotherapists
Is Long-Term Care and Follow-up Necessary After Aortic Valve Replacement?
Yes, it is absolutely necessary. Aortic valve replacement is not the end of the treatment process but the new beginning of a healthy life. Regular lifelong follow-up is essential to ensure that the new valve works smoothly for many years and to maintain the patient’s overall heart health. The follow-up protocol is determined by the physician according to the patient’s condition but usually includes- First month control after the procedure
- First year check
- Followed by regular annual medical examinations and echocardiography (ECHO) checks
Frequently Asked Questions
What is aortic valve stenosis?
Who has this disease?
What are the symptoms?
How is it diagnosed?
Is aortic valve stenosis life threatening?
How is the degree of stenosis determined?
Is medication enough?
What are the surgical treatment methods?
Who is TAVI suitable for?
Which type of caps are used for cap replacement?
How is life affected after a cover change?
Is this disease genetic?
Is exercise harmful?
Is aortic stenosis progressive?

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.