Non-surgical solutions are also offered to the patient in leg vein occlusion, which manifests itself with arterial occlusion. If this vascular occlusion affects a small section, results can be obtained with procedures such as balloon or stent. If it affects a long area, such as the area from the groin to the knee, vascular occlusion can be intervened with by-pass surgery. It is important to intervene in the loss and damage to the leg due to vascular occlusion. During by-pass surgery, depending on the doctor’s preference, the patient is usually awake and local anesthesia is preferred. The patient who is awake during the operation can be informed about the procedures performed.
| Types | Atherosclerotic peripheral arterial disease, embolic occlusion, thrombotic occlusion |
| Causes | Atherosclerosis (arteriosclerosis), clot formation, inflammation or trauma to the artery walls |
| Risk Factors | Smoking, diabetes, hypertension, hypercholesterolemia, advanced age, obesity |
| Symptoms | Pain in the legs when walking (claudication), coldness, discoloration, non-healing wounds on the feet |
| Diagnostic Methods | Ankle arm index (ABI), Doppler ultrasound, CT angiography, MR angiography, conventional angiography |
| Treatment Options | Lifestyle change, antiplatelet drugs, stenting in single vessel, short segment and single small stenosis, bypass surgery in diffuse stenosis |
| Complications | Tissue death (gangrene), amputation, infection, loss of function, chronic pain |
| Protective Measures | Smoking cessation, regular exercise, blood sugar and blood pressure control, healthy nutrition |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Leg Vascular Occlusion?
To visualize a blocked leg artery more easily, think of the network of arteries in your body as a complex system of pipelines that carries water to every corner of a city. The heart is the main pump of this system and the arteries are the main pipes that deliver clean blood full of oxygen and nutrients – the water of life – to the most remote parts of the body. Leg arteriosclerosis is a condition in which rust, dirt and limescale build up over time in the main pipes of this system leading to the legs. In medical language, we call this build-up “plaque” and the process itself “atherosclerosis” or “arteriosclerosis”.
As these plaques build up on the inner walls of the arteries, they narrow the space for blood to flow. Just as less water flows through a water pipe that calcifies over time, less blood reaches the leg muscles through a narrowed artery. Especially when we walk, climb stairs or run, our muscles need more energy and demand more blood. However, narrowed arteries cannot meet this increased demand. It is at this point that the symptoms of leg vascular diseases begin to appear, that is, when the supply cannot meet the demand.
The most important point to remember is this: This “rusting” process that clogs the pipes in the legs is most likely to be gradually continuing in other pipelines of the body, such as the coronary arteries supplying the heart or the carotid arteries supplying the brain. This is why leg vascular occlusion is not just a matter of leg pain, but an alarm bell for the whole body.
What Causes This Silent Danger in Our Veins, Leg Vascular Occlusion?
What causes leg vascular occlusion? The answer to this question is hidden in one word: Atherosclerosis. In other words, hardening of the arteries. This is a very slow and insidious process that usually begins in middle age and beyond, but actually starts in youth and even in childhood. The inner surface of a healthy artery is smooth and slippery, like a Teflon pan. This allows blood cells to flow freely without sticking to this surface. However, some bad habits and health problems can cause tiny scratches and damage to this delicate inner surface over time.
The prime suspects for this damage are the toxins in cigarette smoke, the constant pressure on the vessel wall from uncontrolled high blood pressure and high blood sugar levels. Our body recognizes this damage as a wound and immediately sends in a repair team. However, this well-intentioned repair process can get out of control due to excess “bad” cholesterol (LDL) and other fatty substances circulating in the blood. Cholesterol, calcium and other cellular waste adhering to the damaged area solidifies over time to form deposits called “plaque”.
While these plaques are soft at first, they harden and grow over time, narrowing the blood flow path inside the vessel like a hillock. Symptoms of leg arteriosclerosis begin when this narrowing reaches a critical level. The process usually proceeds in two ways. Either the plaque grows slowly, narrowing the blood vessel more and more over the years and causing chronic symptoms, or a much more dangerous scenario occurs. Sometimes the surface of the plaque can suddenly crack like a volcano. The body again recognizes this crack as bleeding and activates the clotting mechanism. A blood clot (thrombus) rapidly forms in the area and this clot can suddenly and completely block the already narrow vessel, cutting off the blood flow completely. This can lead to sudden cooling of the leg, severe pain and, without immediate intervention, a very serious condition that can lead to tissue death (gangrene). The main steps in the development of atherosclerosis:
- Damage to the inner surface of the vessel
- Fat and cholesterol accumulation in the damaged area
- Formation and growth of a structure called plaque
- Narrowing of the passageway within the vessel (stenosis)
- The plaque becomes unstable and ruptures suddenly
- Formation of a blood clot on the tear (thrombus)
- Sudden and complete blockage of a blood vessel by a clot.
Which Early Symptoms of Leg Vascular Occlusion Reduces Quality of Life?
Leg vascular occlusion usually first becomes apparent when you are on the move. The most typical and common early symptom is intermittent claudication, popularly known as “window disease”. The reason it is called window disease is that people with this pain often feel the need to rest and pretend to look at shop windows in order not to show it to others. This is pain, cramping, tightness or fatigue in the leg muscles, especially in the calves, after walking a certain distance or exerting effort, such as stairs.
The most important feature of this pain is that it disappears completely within a few minutes when you rest. When you start walking, it reappears at the same distance. The reason for this is that the narrowed blood vessels cannot meet the increased oxygen demand of the muscles in motion. The muscles scream “I’m out of oxygen, help!” and we feel this signal as pain. When we rest, the oxygen demand of the muscles returns to normal and the pain goes away. This pain is definitely not a natural consequence of aging or a simple muscle pain. A healthy individual is not expected to have leg pain that recurs regularly with walking, depending on age.
The area where the pain is felt can also provide valuable information about the location of the blockage. For example, if the pain is most often felt in the calf, the problem is usually in the femoral or popliteal arteries. If the pain is in the buttocks, buttocks or thighs, this indicates that there may be signs of blockage in the veins further up, even in the groin, or a narrowing of the main veins in the abdomen (iliac arteries). Sometimes the symptoms of vascular occlusion in the left groin may be different or more pronounced than on the right side, because the disease does not always affect both legs symmetrically. These are the main features of classic walking pain:
- Occurs only during exertion (walking, running)
- Completely passes in 1-2 minutes with rest
- May feel more like cramping, tightness or fatigue than pain
- Most common in the calf muscles
- It can also be in the thigh or buttock muscles
- It usually starts after a similar walking distance each time.
What Serious Warnings Does Advanced Leg Vascular Occlusion Cause?
If the early symptoms are not taken seriously and the underlying atherosclerotic process continues, leg vein occlusion can progress to a more serious and dangerous stage. At this stage, problems begin to occur not only during movement but also at rest. This is a sign that blood flow is so reduced that the muscles and tissues are unable to meet even their minimal oxygen needs at rest. This condition is called “Critical Limb Ischemia” and is an emergency with the risk of limb loss.
The most important symptom of this stage is “rest pain”. This is a constant, severe and burning pain, usually in the feet and toes, that occurs especially at night when you lie in bed. Patients often describe this pain as “my feet are on fire” or “like pins and needles”. The pain is so severe that it can wake you up from sleep. Many people instinctively feel the need to dangle their legs off the bed to relieve the pain. This is because gravity helps to get a little more blood to the feet, providing temporary relief. The presence of pain at rest is the clearest sign that leg vein occlusion is no longer just a problem that impairs quality of life, but a danger that threatens the future of the limb.
Another very important and dangerous symptom of advanced disease is non-healing wounds, which are one of the symptoms of foot and leg vascular occlusion. Normally, a simple injury such as a small scratch, a knock from a shoe or an ingrown toenail heals in a few days, whereas this is not possible in a leg with severely impaired blood circulation. For the wound to heal, the blood needs to carry plenty of oxygen, nutrients and immune cells to fight infection. Due to poor blood flow, this “support team” cannot reach the wound site. As a result, even the simplest wound can remain open for months, easily become infected and develop into open wounds called “arterial ulcers”, which are often very painful and difficult to treat. These wounds usually occur in areas that are subjected to pressure, such as the toes, heel or sides of the feet. The alarming symptoms of advanced disease are:
- Foot pain that occurs at night and wakes you up from sleep
- Persistent numbness or numbness in the feet and fingers
- Even simple wounds, such as a shoe stub, do not heal for weeks
- Spontaneous painful wounds (ulcers) on the foot or leg
- Blackening or discoloration of the toes or heel (onset of gangrene)
- Sudden onset of very severe pain in the leg and inability to move the leg.
What Modifiable Habits Increase the Risk of Leg Vascular Occlusion?
Leg vascular occlusion is not fate. Many of the factors that play a role in its occurrence and progression are directly related to our lifestyle choices and habits. This is also good news. Because by controlling these risks, we can prevent the disease, slow its progression and even reverse it. This means that we are in control.
The number one enemy of blood vessels is smoking and tobacco products. If we had to pick a single culprit for leg vein blockage, it would definitely be smoking. The thousands of toxic chemicals in cigarettes directly attack and damage the smooth inner surface of blood vessels, increasing the risk of blood clots, lowering “good” cholesterol and making it easier for “bad” cholesterol to stick to the vessel wall. The risk of developing leg vascular occlusion in a smoker is many times higher than in a non-smoker, and the disease progresses much faster.
The second major culprit is uncontrolled diabetes. High blood sugar levels “sugar-coat” the blood vessels from the inside, destroying their structure and accelerating the process of atherosclerosis enormously. In patients with diabetes, problems affecting small vessels, such as symptoms of capillary blockage, especially in the legs, are also common. In addition, the sensation of pain in the foot may be reduced due to damage to nerve endings (neuropathy) caused by diabetes. This prevents the patient from recognizing a wound on their foot, setting the stage for very dangerous infections and non-healing wounds.
High blood pressure (hypertension) and high cholesterol are important parts of this dangerous equation. High blood pressure is like a constant hammering on the walls of blood vessels, fatiguing them and making them vulnerable to damage. High cholesterol is the main ingredient in the mortar used to plaster these damaged walls, which over time clogs the arteries. Overweight and obesity, caused by a sedentary lifestyle and unhealthy diet, is a condition that combines or triggers all of these risk factors.
Which Factors We Cannot Change Set the Stage for Leg Vascular Occlusion?
While our lifestyle choices can have a huge impact on our vascular health, unfortunately there are some risk factors that we cannot control. We cannot change these factors, but being aware of them helps us understand why we need to be even more careful and rigorous about the factors we can change.
The most important of these is advancing age. Time causes some wear and tear in our arteries, as it does in every organ. As we age, our arteries lose some of their natural flexibility and become more prone to plaque build-up. The risk of leg vascular occlusion usually starts to become apparent after the age of 50, and the incidence increases considerably in the 70s.
Another important factor is our genetic heritage, i.e. family history. If a first-degree relative (mother, father or siblings) has a history of early leg artery blockage, heart attack or stroke, you may have a higher than average risk of developing these diseases. This could mean that your vasculature or the way your body processes cholesterol is genetically predisposed to this condition.
Male gender is also considered a risk factor, as leg vein occlusion tends to occur earlier in men than in women. However, in the post-menopausal period, with the decrease in the protective hormone estrogen, the risk increases rapidly in women and becomes equal to that of men. In addition, some systemic conditions such as chronic kidney disease also accelerate the process of atherosclerosis and pose a significant risk for leg arteriosclerosis.
How to recognize leg vein occlusion when you go to the doctor?
You may be worried about how to recognize a blocked blood vessel in the foot or how to find out if this is the problem with your legs. The diagnostic process is actually quite simple and usually involves nothing to be afraid of. It starts with listening to your story. As a physician, the most valuable information for us is what you tell us. Details such as when your complaints started, what triggers them, what reduces them, exactly where and how the pain feels are the first and most important steps on the way to diagnosis.
This is followed by a simple physical examination. One of the most important parts of this examination is to check the pulses in your legs and feet. We check the arterial pulses at certain points, such as the back of the foot, the inside of the ankle and the back of the knee. The pulses beyond a blocked artery are either very weak or absent. This is a very strong physical sign of a blockage. The legs are also carefully examined for color, temperature, skin condition and possible wounds.
After these initial assessments, a very simple, painless and quick test called the “Ankle-Belly Index” (ABI) is usually performed to confirm the diagnosis. This test uses a sphygmomanometer and a small ultrasound device (Doppler) to measure and compare the blood pressure in your arm with the blood pressure in your ankle. In a healthy person, the ankle pressure is expected to be equal to or slightly higher than the arm pressure (a ratio of 1.0 or higher). If there is a narrowing of the blood vessels, the pressure in the ankle drops and the ratio falls below 0.9. The lower the ratio, the more serious the obstruction. In most cases, the patient’s history, physical examination and ABI test are sufficient for diagnosis. If a more detailed examination or intervention is planned, then advanced imaging methods such as Color Doppler Ultrasonography or Angiography may be used to map the vessels. Here is important information to share when you contact your doctor:
- Exact location of the pain you feel (calf, thigh, buttock)
- When the pain started (e.g. after walking 100 meters)
- Character of the pain (cramping, burning, squeezing)
- Whether the pain goes away at rest
- A change in color or temperature that you notice in your legs or feet
- Whether you have any wounds that do not heal
- Any other medical conditions you have (diabetes, blood pressure, cholesterol)
- List of all medicines you take on a regular basis
- Smoking status (if you smoke, how much, if you quit, when).
What is the treatment?
Smoking cessation, diet, lowering the levels of cholesterol and other fats in the blood and helping to keep blood pressure under control,
Exercise not only helps the muscles to use oxygen more efficiently, but also accelerates the development of collateral circulation (a new vascular network of small arterial branches that develop beyond the occlusion).
Blood thinners (e.g. aspirin and clopidogrel), Cholesterol-lowering drugs (statins)
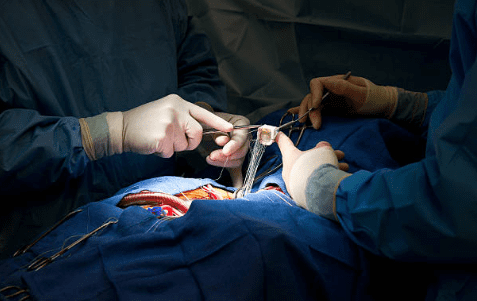
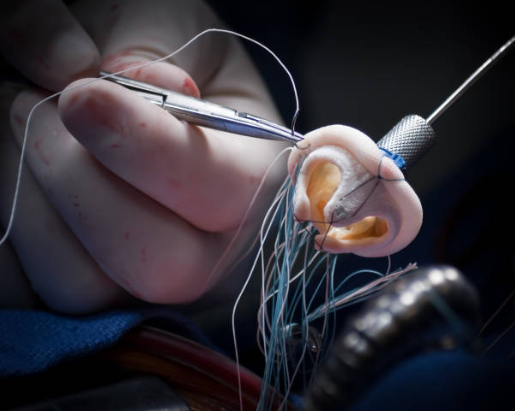
Surgical treatment (Peripheral Bypass)
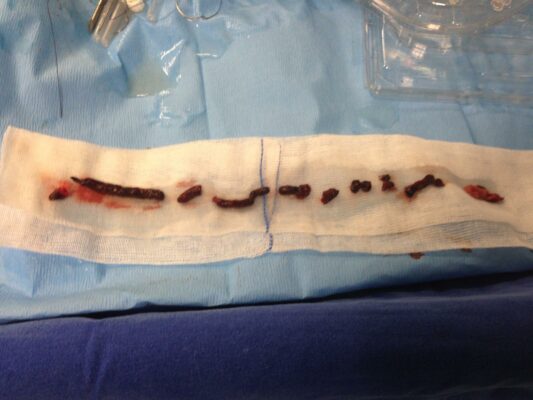
Surgical treatment for peripheral vascular disease includes peripheral bypass procedures and endarterectomy. Nowadays, minimally invasive procedures are performed even at the ankle level. Lesions causing obstruction within the vessel, vessels with multiple stenoses or severe stenoses with long segments are conditions that require surgical treatment. Bypass surgery is the use of a vein or synthetic vessel (known as a graft) taken from your body to provide blood flow through a side path from before to after the blocked area. An endarterectomy is the removal of the plaque layer that causes the blockage in the artery leading to the arms or legs.
Frequently Asked Questions
What is leg vascular occlusion?
Leg vascular occlusion is a narrowing or blockage of the arteries that prevents sufficient blood from reaching the legs.
What are the symptoms of leg vein occlusion?
Pain, numbness, coldness, discoloration and open sores in the legs when walking are the most common symptoms.
At what age does atherosclerosis occur?
Although it is usually seen in people over the age of 50, it can also be seen at younger ages due to smoking, diabetes and genetic factors.
Which blood vessels are most affected by blockage?
Blockage of the arteries in the groin and knee area is most common.
What causes leg vein occlusion?
The most common cause is atherosclerosis, the build-up of cholesterol in the vessel walls.
How is leg vein occlusion diagnosed?
After physical examination, imaging methods such as Doppler ultrasound, CT angiography or MR angiography are used.
What happens if the blockage is not treated?
In advanced stages, it can lead to tissue loss, gangrene and even leg amputation.
Can leg vein occlusion be treated?
Yes, surgical treatment with small incisions is possible.
Does congestion cause symptoms other than pain?
Yes, there may be symptoms such as pale skin, brittle nails, delayed healing of wounds.
Does smoking affect leg vein occlusion?
Yes, smoking narrows the blood vessels and significantly increases the risk of blockages.
Is walking recommended for leg artery occlusion?
No, because with walking, the blood supply is insufficient and muscle cramps and necrosis of the toes increase, accompanied by severe pain.
Does blocked arteries also increase the risk of heart attack?
Yes, people with blockages in their leg veins may also have blockages in their heart and brain veins.
Does it recur after treatment?
With appropriate lifestyle and medication, the risk of recurrence can be reduced but not completely eliminated.
How long does the treatment process take?
Although it depends on the level of obstruction and the treatment method applied, the follow-up process is usually long-term.
Which doctor to consult?
Cardiovascular surgery is the only department specialized in vascular diseases.
Blog Yazıları
Heart Disease: Types, Causes, and Symptoms
Prof. Dr. Yavuz Beşoğul » General » Heart Disease: Types, Causes, and SymptomsHeart diseases are [...]
Aug
How the Heart Works
Prof. Dr. Yavuz Beşoğul » General » How the Heart WorksThe heart functions as a [...]
Aug
How Many Hours Does Heart Valve Surgery Take?
Prof. Dr. Yavuz Beşoğul » General » How Many Hours Does Heart Valve Surgery Take?Heart [...]
Aug
How long does coronary artery bypass (CABG) surgery take?
Prof. Dr. Yavuz Beşoğul » Coronary Artery Bypass » How long does coronary artery bypass [...]
Aug
Kalp Kapak Değişimi Ameliyatı Nedir? Kalp Kapak Değişimi Nasıl Yapılır?
Prof. Dr. Yavuz Beşoğul » Kalp Kapak Hastalıkları » Kalp Kapak Değişimi Ameliyatı Nedir? Kalp [...]
Aug
Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki Fark
Prof. Dr. Yavuz Beşoğul » General » Kalp Kapakçığı Tamiri ve Kalp Kapakçığı Değişimi Arasındaki [...]
Aug
Life After Heart Valve Surgery
Prof. Dr. Yavuz Beşoğul » General » Life After Heart Valve SurgeryLife after heart valve [...]
Aug
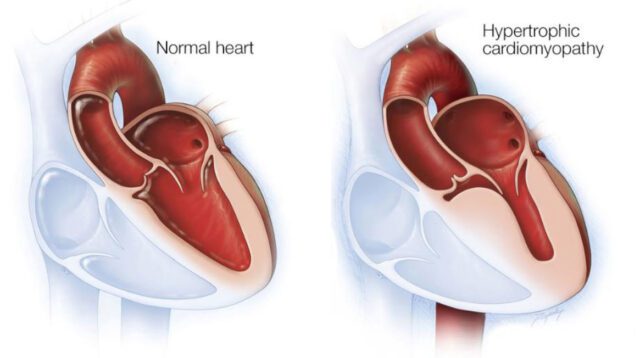
Hypertrophic Cardiomyopathy: Symptoms & Treatment
Prof. Dr. Yavuz Beşoğul » General » Hypertrophic Cardiomyopathy: Symptoms & TreatmentHypertrophic cardiomyopathy is a [...]
Aug