Cardiac arrest symptoms occur suddenly and require immediate medical attention. The most typical signs are sudden collapse, loss of consciousness, and absence of pulse. Without rapid intervention such as CPR and defibrillation, cardiac arrest is fatal within minutes.
Early warning signs of possible cardiac arrest may include chest pain, dizziness, palpitations, and shortness of breath. These symptoms often precede cardiac arrest in individuals with underlying heart disease. Recognizing them increases the chance of survival with timely medical help.
Risk factors for cardiac arrest include coronary artery disease, arrhythmias, heart failure, and genetic syndromes. Lifestyle-related factors such as smoking, obesity, and lack of exercise further increase susceptibility. Regular cardiac evaluations help identify at-risk patients early.
Emergency management of cardiac arrest involves immediate CPR, use of an automated external defibrillator, and advanced hospital care. Public awareness and widespread availability of defibrillators significantly improve survival rates. Rapid response remains the key determinant of patient outcome.
What Does Cardiac Arrest Mean?
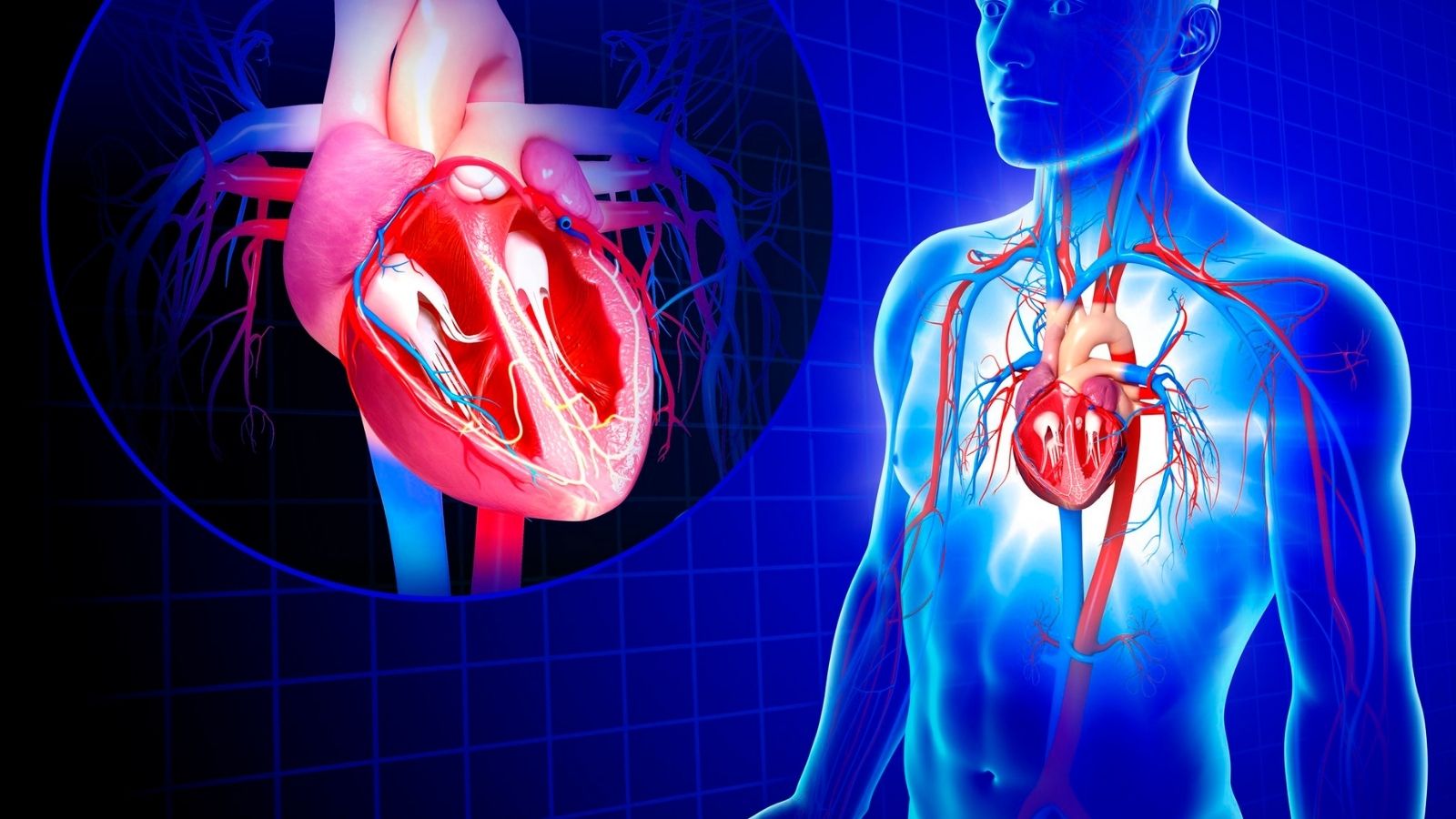
The easiest way to understand cardiac arrest is to think of it as an electrical malfunction. Our heart has a complex electrical system that regulates its every beat. Just like the wiring in a house, this system allows the heart muscle to contract rhythmically and pump blood throughout the body. At the moment of cardiac arrest, there is a major “short circuit” or “blown fuse” in this electrical system.
As a result of this electrical storm, the heart begins to tremble senselessly so that it cannot pump blood (this is called ventricular fibrillation) or stops its electrical activity altogether (asystole). As a result, blood circulation is suddenly cut off. As there is no blood supply to any organ, especially the brain, the person loses consciousness within seconds, normal breathing stops and the pulse becomes imperceptible. The colloquial expression “the patient is in arrest” describes this dramatic situation. It is literally a race against time.
What is the Difference Between a Heart Attack and Cardiac Arrest?
Although these two concepts are often used interchangeably, there is a fundamental difference between them. Knowing this difference is vital for correct first aid and treatment.
You can think of a heart attack as a blockage in the plumbing in your home. It is a “circulatory” problem. One of the blood vessels (coronary arteries) that supply the heart is blocked by a clot. The area of the heart muscle supplied by that blood vessel is deprived of oxygen and begins to be damaged. At this time, the person is usually conscious, experiencing symptoms such as severe chest pain and shortness of breath, but their heart is still beating.
Cardiac arrest is like the entire electrical network of the house going down, like the main fuse blowing. It is an “electrical” problem. The pumping function of the heart has completely and suddenly stopped.
So how are these two related? A heart attack is one of the most common triggers of cardiac arrest. During a heart attack, damaged and deprived of oxygen, the heart muscle becomes electrically very sensitive and unstable. This imbalance can trigger a fatal arrhythmia – cardiac arrest. In short, a plumbing problem (heart attack) can lead to a major electrical failure (cardiac arrest). However, it should be remembered that not every cardiac arrest is the result of a heart attack.
How to recognize when a person is in cardiac arrest
The diagnosis of cardiac arrest does not require complex tests; the symptoms are very clear and must be recognized quickly. This is because the brain can only withstand oxygen deprivation for a few minutes. There are three main signs that allow rapid recognition of cardiac arrest:
Lack of Response: The person does not react even if you call out or gently shake their shoulder.
Abnormal Breathing The patient does not breathe normally. Either his/her breathing has stopped completely or he/she makes irregular and ineffective breathing sounds called “agonal breathing”, as if he/she is dying, sighing. These sounds are not normal breathing and are an important sign of arrest.
No Pulse No pulse can be felt in the carotid artery on the side of the neck. Instead of wasting time looking for a pulse, non-health professionals are advised to act immediately if the first two symptoms are present.
What Causes Cardiac Arrest?
The underlying causes of cardiac arrest are diverse. Knowing these causes not only determines the direction of emergency intervention but also provides a roadmap to prevent recurrence in the long term. The most common causes are the following:
Coronary Artery Disease: Responsible for the vast majority of all cases. The most common scenario is that plaque that has accumulated in the heart vessels over the years ruptures, forms a clot and triggers a heart attack.
Structural Disorders of the Heart: Sometimes the problem is not in the blood vessels but in the heart muscle or valves themselves. Some conditions that disrupt the structure of the heart and increase the risk are:
- Cardiomyopathies (heart muscle diseases)
- Advanced valvular heart disease
- Congenital heart defects
- Heart failure
Hereditary (Genetic) Causes: Sometimes the heart looks completely normal structurally. The problem is a defect in the genes that govern the electrical activity of the heart cells. This condition is called “channelopathy”. Such genetic diseases are often behind sudden deaths, especially in young people and athletes.
- Long QT Syndrome
- Brugada Syndrome
- Short QT Syndrome
- Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
- Other Causes: Some non-cardiac conditions can also cause cardiac arrest.
- A large clot in the lung (Pulmonary Embolism)
- Serious trauma and bleeding
- Side effects of certain medications or drug use
- Serious disturbance of electrolyte (such as potassium, magnesium) balance in the body
- Electric shock
Are There Causes of Cardiac Arrest That Can Be Corrected by Emergency Intervention?
Yes, it does, and this is one of the most promising parts of resuscitation efforts. Especially in rhythms that do not respond to electroshock, finding and treating an underlying cause that can be quickly corrected directly increases the patient’s chances of survival. These causes, which we keep in mind as “Hs and Ts” in medicine, are like a checklist for emergency intervention:
These are the situations that we call ‘H’s’ in medicine and can be intervened quickly:
- Hypovolemia (excessive fluid loss)
- Hypoxia (lack of oxygen)
- Hydrogen ion (increased acidity in the blood)
- Hypo/Hyperkalemia (potassium imbalance)
- Hypothermia (low body temperature)
- Then there are the so-called ‘T’s’, which often require immediate intervention. Especially for a cardiovascular surgeon, this list indicates conditions that may require immediate surgical intervention.
- Tension Pneumothorax (lung deflation and pressure on the heart)
- Tamponade (accumulation of fluid in the heart membrane)
- Toxins (drugs or poisonous substances)
- Thrombosis (a clot in a lung or heart vessel)
For example, if the ultrasound performed during arrest case management shows that blood has accumulated around the heart (tamponade), the only solution to this situation is to drain that blood urgently with a needle or surgically. It is in these moments that the response to an arrest patient ceases to be just CPR and medication and becomes dependent on the immediate skill of a surgical team.
What Does Chain of Life Mean for Cardiac Arrest Management?
Saving someone from cardiac arrest is not possible by a miraculous act of one person, but by the timely execution of a series of correct and coordinated actions. We call this set of actions the “Chain of Life”. If even one link in the chain is missing or weak, the chances of success are unfortunately reduced.
The links of the Chain of Life are:
- Recognizing the situation quickly and calling 112
- Immediate and quality CPR
- Rapid electroshock application (Defibrillation)
- Intervention by advanced life support teams
- Professional care after arrest
- Recovery and rehabilitation process
What is a Quality Cardiopulmonary Arrest Intervention?
perhaps the most important link in the “Chain of Life” is high-quality CPR until professional help arrives. Because CPR means manually pumping blood to the brain and other vital organs to replace the stopped heart. This saves precious minutes to prevent brain damage. The essentials of a high-quality CPR are the following:
Correct Speed: It should be done at a speed between 100 and 120 per minute (the rhythm of the Bee Gees’ “Stayin’ Alive” is a good reference for this speed)
Adequate Depth: In an adult human, the sternum should be collapsed by at least 5 cm and no more than 6 cm.
Complete Relaxation of the Thorax: After each compression, the rib cage should be allowed to fully recover. This is critical for the heart to fill with blood again.
Minimum Possible Interruptions: Interruptions to CPR (e.g. for artificial respiration) should be as short as possible. The goal is to massage without interruption for a large part of the time.
Remember that not intervening at all is the worst option. Even if you have no training, just performing CPR under the guidance of a 112 operator can save someone’s life.
How does the Arrest Case Intervention Process in the Hospital Work?
When a patient arrests in hospital, a “code blue” announcement is made within seconds and a specially trained resuscitation team arrives on the scene. From this moment on, everything proceeds according to a predetermined plan of action – an algorithm. This organized teamwork avoids confusion and ensures that every step is taken at the right time.
The electrical rhythm of the heart is monitored by electrodes attached to the patient’s chest. The intervention in an arrest case is completely shaped according to this rhythm. If the rhythm is one that can be corrected with a shock, such as “ventricular fibrillation”, the priority is to immediately use the defibrillator. Once the shock has been delivered, CPR is immediately continued for 2 minutes, regardless of the outcome. During these 2-minute cycles, the IV is opened, the necessary drugs (adrenaline, antiarrhythmics) are administered, and at the end of each cycle the rhythm is checked again and a new shock is administered if necessary.
If the monitor shows a flat line (asystole) or a regular rhythm without a pulse (pulseless electrical activity), there is no point in shocking. In this situation, the focus is on continuous and very high quality CPR, administering adrenaline as soon as possible, while quickly looking for reversible causes (list of Hs and Ts) that may have led to this situation.
What Advanced Therapies Are Available for Resistant Cardiac Arrest Case Management?
Sometimes, despite all standard resuscitation efforts, the heart cannot be started, or even if it is started, it stops again. It is in these “resistant” cases that more advanced and technological treatments come into play. This is a process that usually involves a cardiovascular surgeon and interventional cardiologist.
Emergency Coronary Angiography and Surgery: If the cause of the arrest is thought to be a blocked heart vessel, the patient can be quickly taken to the angiography laboratory. The blocked vessel can be opened with a balloon or stent. Sometimes the vessel structure is not suitable for a stent or a mechanical problem develops, such as a tear in the heart due to a heart attack. In this case, the only option is to rush the patient to the operating room for emergency bypass surgery (CABG) or surgery to repair the tear. This is a critical surgical intervention against the clock.
ECMO resuscitation (ECPR): This is one of the most advanced life support methods in modern medicine. ECPR is a “bridge” treatment for selected patients who do not respond to standard resuscitation. In this method, while CPR continues, a surgical team quickly inserts cannulas into the patient’s inguinal veins and transfers the patient’s blood to a machine (ECMO device) outside the body. This machine oxygenates the blood, removes carbon dioxide and pumps it back into the body. In short, the ECMO machine temporarily takes over the function of both the heart and the lungs. This gives us, the physicians, golden time to solve the real cause behind the stopped heart, such as dissolving a large clot in the lung, treating poisoning or preparing the patient for an angioplasty/surgery. ECPR is a glimmer of hope that can significantly improve survival rates, especially in young and diagnosed arrest patients.
How Does the Arrest Patient’s Intervention Continue After the Heart is Restarted?
Restarting the heart is only the first half of the battle. The real battle continues with a complex process called “post-arrest care”, which is carried out in intensive care units. This is because during the arrest the whole body, especially the brain, has been exposed to severe oxygen deprivation. The aim of this period is to minimize this damage.
Targeted Temperature Management (TTM): This is the most basic method to limit brain damage in unconscious patients after arrest. The aim is to actively prevent fever and maintain body temperature at a constant level (usually 36-37.5°C) for several days. This controlled mild coolness slows down brain metabolism, reduces brain edema and suppresses the chemical reactions that cause damage. It is like giving the wounded brain a chance to recover:
Assessment of Brain Functions: What the neurologic status of the patient will be is the most worrying question for both the family and the physicians. It is very important not to make a hasty decision on this issue. Because brain functions in the first hours after resuscitation may be misleading due to the drugs used and metabolic status. For this reason, we usually wait at least 72 hours and then evaluate more than one method together to get an idea of the patient’s condition.
- Detailed neurological examination (such as pupil reflexes)
- Brain electroencephalogram (EEG)
- Evoked potential tests (SSEP)
- Brain tomography and MRI imaging
- Blood markers of brain damage (such as NSE)
What are Secondary Prevention and Long-Term Treatment Methods After Cardiac Arrest?
Surviving a cardiac arrest is like starting life anew. However, this does not mean that the risk of a similar event happening in the future is eliminated. Long-term treatment therefore focuses on minimizing this risk.
Implantable Cardioverter-Defibrillator (ICD): This device is the main pillar of secondary prevention. Similar to a pacemaker but much smarter, it is implanted under the skin and one or more wires (electrodes) extend into the heart. The ICD’s job is to analyze the heart’s rhythm within seconds. If it detects a dangerous life-threatening arrhythmia, it automatically delivers an electroshock within seconds to correct it. In other words, the ICD works like a “guardian angel” or “emergency response team” placed inside the body to prevent sudden death.
Catheter Ablation The ICD treats the arrhythmia but does not prevent it from occurring. If a patient has frequent episodes of arrhythmia and the ICD shocks frequently, this can significantly reduce quality of life. This is where catheter ablation comes in. In this procedure, special catheters are inserted into the heart through the groin. Using three-dimensional mapping systems, the abnormal electrical signal foci or short circuit pathways causing the arrhythmia are identified one by one and destroyed with radio frequency energy (a kind of burning). Successful ablation can significantly reduce or even completely eliminate ICD shocks.
Medication and Lifestyle: Of course, it is essential that the underlying heart disease (heart failure, coronary artery disease, etc.) is treated effectively with the latest medications. In addition, some key lifestyle changes are of great importance.
- Quit smoking completely
- Maintaining a healthy weight
- Regular physical activity as recommended by the doctor
- Eating a diet low in salt and saturated fats and rich in vegetables and fruits
- Learning stress management techniques
- Keeping blood pressure and cholesterol levels under control

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.