A heart attack, or myocardial infarction, occurs when blood flow to the heart muscle is blocked. The most common symptom is chest pain or pressure, often radiating to the arm, neck, or jaw. Shortness of breath, sweating, and nausea may accompany these signs.
Silent heart attacks may present without obvious chest pain. Fatigue, dizziness, or mild discomfort are often overlooked, especially in women and elderly patients. Early recognition of atypical symptoms is critical for timely treatment.
Risk factors for heart attack include high blood pressure, high cholesterol, diabetes, smoking, obesity, and family history of heart disease. Preventive measures such as lifestyle modification and medical therapy significantly reduce the likelihood of myocardial infarction.
Emergency treatment involves restoring blood flow to the affected coronary artery. Methods include thrombolytic drugs, angioplasty, or stent placement. Rapid intervention minimizes heart muscle damage and improves survival rates.
|
Definition |
The condition in which the heart muscle does not receive enough oxygen as a result of sudden blockage of the coronary vessels and the tissue is damaged |
|
Causes |
Coronary artery occlusion (atherosclerosis and clot), rarely vessel spasm, coronary embolism, vessel rupture |
|
Risk Factors |
Advanced age, male gender, family history of heart attack, smoking, hypertension, diabetes, high cholesterol, obesity, sedentary lifestyle, stress |
|
Symptoms |
Chest pain (squeezing, pressing, longer than 20 minutes), pain radiating to the left arm, jaw, back, sweating, nausea, vomiting, shortness of breath, dizziness, fainting, sudden death |
|
Diagnostic Methods |
ECG, cardiac enzymes (troponin, CK-MB), echocardiography, coronary angiography |
|
Treatment Methods |
Oxygen, aspirin, antiplatelet drugs, heparin, thrombolytic therapy, balloon angioplasty, stents, coronary bypass surgery, lifestyle changes |
|
Complications |
Heart failure, arrhythmia, cardiogenic shock, heart wall rupture, aneurysm, death |
|
Prevention Methods |
Smoking cessation, healthy nutrition, regular exercise, stress management, blood pressure and cholesterol control, diabetes management, regular use of medications |
Why and how does a heart attack develop?
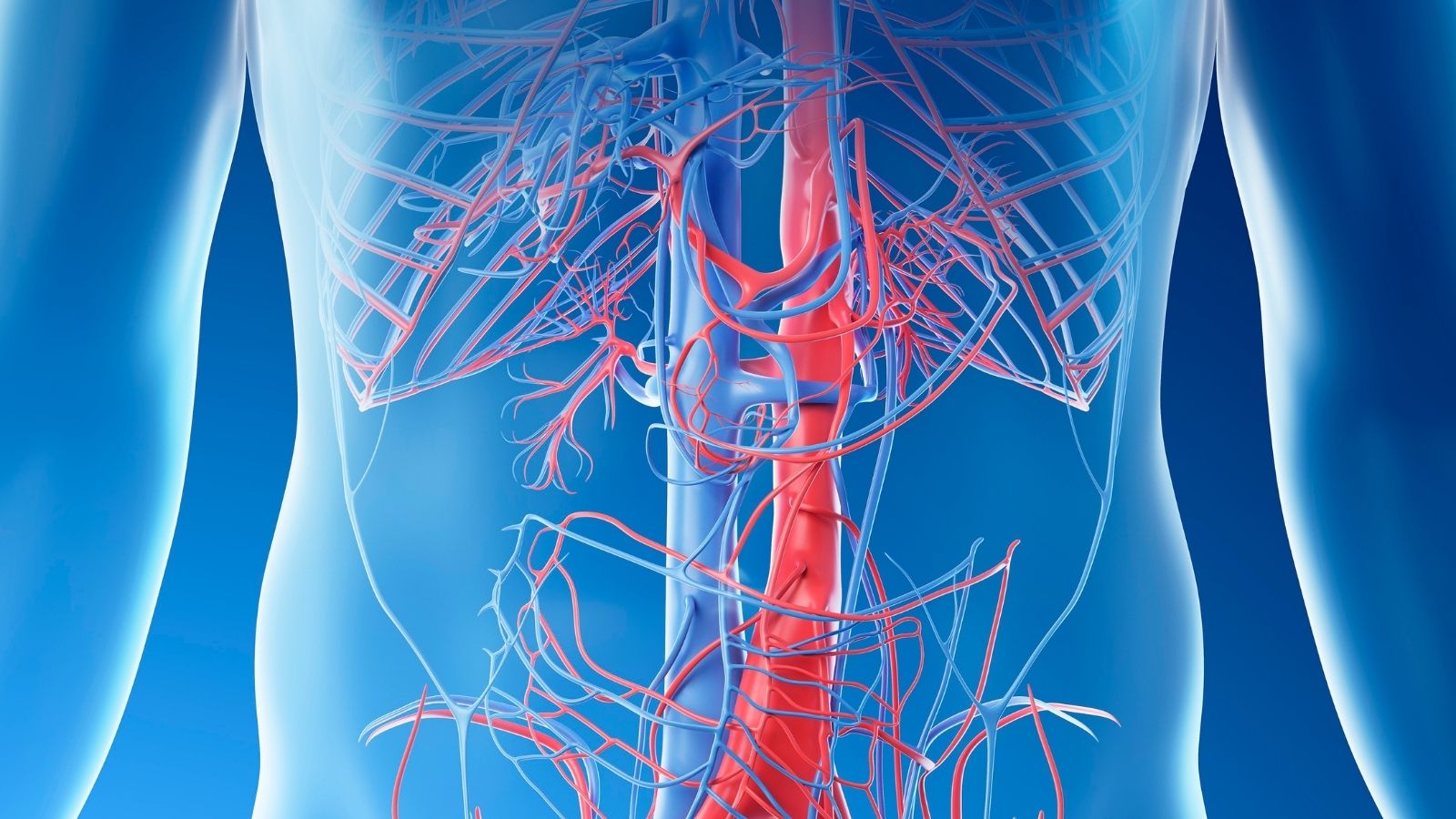
Understanding the process behind a heart attack is the first step to preventing it. It all starts with fatty deposits called “atherosclerotic plaques”, which can be likened to rust and limescale lining the inner walls of arteries like the inside of a plumbing pipe. These plaques grow slowly over the years as cholesterol, fat and other cellular waste build up, silently narrowing the arteries. We call this process arteriosclerosis, or atherosclerosis in medical terms.
For many years, these plaques can remain on the vessel wall without causing any symptoms. One day, however, the surface of one of these plaques becomes sensitive for various reasons (high blood pressure, stress, etc.) and cracks or tears. Our body recognizes this cracking as a wound and immediately goes into “repair” mode. Platelets, the cells responsible for blood clotting, flock to this cracked area and form a blood clot (thrombus). It is this “well-intentioned” repair mechanism that starts the disaster. The clot can become so large that it can completely block the already narrowed vessel in an instant.
When this happens, the area of the heart muscle supplied by that vessel is instantly deprived of oxygen. Within minutes, this oxygen starvation begins to cause irreversible damage. Deprived of oxygen, heart muscle cells begin to die and are replaced by scar tissue that is incapable of contracting. The extent of the damage depends on how long the blockage lasts and how large an area of the heart it affects. This damage can permanently reduce the heart’s pumping power and set the stage for serious problems such as heart failure and arrhythmias.
The road to a heart attack is often paved years in advance. The stones on this road are our risk factors. Some of them we cannot change, but many of them are under our control.
What are the modifiable risk factors that lead to heart attacks?
These are factors that directly affect the risk of heart attack, which we can control through lifestyle changes and medical treatment. It is important to remember that when these factors combine, the risk does not simply add up, it increases exponentially.
The main risk factors you can control are:
- Smoking and use of tobacco products
- High blood pressure (Hypertension)
- High blood cholesterol (especially LDL – bad cholesterol)
- Diabetes (Diabetes)
- Overweight and obesity (especially fat around the waist)
- Physical inactivity
- Unhealthy and unbalanced diet
- Intense and unmanaged chronic stress
- Excessive alcohol consumption
Each of these factors accelerates the process of atherosclerosis by damaging the vessel wall or increasing the workload of the heart. For example, smoking poisons the delicate lining of the inner surface of blood vessels (the endothelium), setting the stage for plaque formation and increasing the tendency of blood to clot. Diabetes, on the other hand, makes the blood more “sticky” and reduces the elasticity of the vessel walls. Intervening in one of these factors therefore often creates a domino effect that positively affects the others.
Are there unchangeable risk factors that predispose to heart attacks?
Yes, unfortunately some risk factors are beyond our control. Even if we cannot change them, knowing about them is a warning to be even more diligent about other controllable factors.
We can list the main risk factors that we cannot change as follows:
- Advanced age: The risk increases after the age of 45 for men and 55 for women.
- Gender: Men are at higher risk than women until menopause. This difference decreases after menopause.
- Family history: A family history (mother, father, siblings) of heart disease or heart attack at an early age indicates that you may also be genetically predisposed. This is particularly important for male relatives under 55 and female relatives under 65.
What are the less common causes of heart attacks?
Although the vast majority of heart attacks are due to atherosclerosis, other causes can also play a role, especially in young people or in people whose underlying coronary artery disease is not obvious.
More rare causes of heart attack include
- Coronary artery spasm
- Spontaneous coronary artery dissection (SCAD)
- Blood clot (embolism)
- Some infectious diseases
- Congenital heart vessel anomalies
In particular, SCAD is caused by a spontaneous rupture of the inner layer of the vessel wall and should be considered more frequently in women who show signs of a heart attack at a young age, especially those who have given birth.
In a heart attack, time is literally life. Recognizing the body’s warning signals and taking them seriously is key to preventing permanent damage and saving lives. Symptoms are not always as dramatic as in the movies.
What are the most common heart attack symptoms?
Although chest pain is the first symptom that comes to mind when you think of a heart attack, it may not always be the only or most obvious sign. You may experience one or more of these symptoms at the same time.
The most common heart attack symptoms are:
- Pressure, tightness, heaviness or burning sensation in the chest
- Pain radiating to the left arm, shoulders, neck, jaw or back
- Shortness of breath that starts suddenly and does not go away with rest
- Unexplained cold sweating
- Nausea or vomiting
- Feeling dizzy or lightheaded
- Sudden and extreme fatigue, weakness
Chest discomfort is a feeling of pressure, often described as “like someone is sitting on my chest” or “like they are squeezing my chest with a belt”, rather than pain. This sensation can last for more than a few minutes, pass and then start again.
Are the symptoms of a heart attack different in women than in men?
Yes, this is a very important point. Although chest pain is the most common symptom in women, the symptoms of a heart attack in women can be more varied and sometimes more “atypical” than in men. Unfortunately, this can cause women to downplay or misinterpret their complaints.
Here are the signs of a heart attack in women to look out for in particular:
- Back, shoulder or jaw pain (without chest pain)
- Unusual and extreme fatigue (sometimes starting days before the crisis)
- Indigestion or upper abdominal pain similar to heartburn
- Shortness of breath
- Sudden onset of anxiety or panic
Because of these symptom differences, the symptoms of a heart attack experienced by women can sometimes be mistaken for flu, stomach upset or anxiety. This is why women, especially those with risk factors, need to be extra vigilant about unusual changes in their bodies.
What is a silent heart attack and who should be more vigilant?
A silent heart attack, as the name suggests, is a real heart attack that is either asymptomatic or the symptoms are so mild that the person does not notice them. A person may experience mild indigestion, muscle pain or fatigue and attribute it to something else. In the meantime, however, the heart muscle is being damaged.
A silent heart attack is often diagnosed by chance months or years later, during an ECG (electrocardiogram) or echocardiogram performed for another reason.
There are groups at higher risk of silent heart attacks:
- Diabetes (sugar) patients
- Older individuals
- Women
Especially in diabetics, the pain sensation may be dulled due to damage to nerve endings caused by high blood sugar (neuropathy). These patients may therefore have a heart attack without feeling severe chest pain. In people in these groups, symptoms such as sudden and unexplained shortness of breath, weakness or confusion may indicate a heart attack and should be taken seriously. Sometimes patients may perceive this as a false heart attack, but the danger is real.
If a heart attack is suspected, even a second counts. the thought “Let me wait a little, maybe it will pass” leads to the loss of heart muscle tissue, which is the most valuable thing to lose.
What is the first thing to do in case of a suspected heart attack?
There is only one right thing to do when you suspect a heart attack: Call 112 Emergency Service immediately.
Never try to drive yourself to the hospital. An ambulance is both faster and the medical team in it has the opportunity to start life-saving first interventions (such as giving oxygen, opening an IV, monitoring the rhythm) on the way. They will also direct you directly to the nearest center equipped to treat a heart attack.
after dialing 112, you can chew an aspirin to dilute the blood, as directed by the operator, if there are no other obstacles. However, never delay calling 112 to seek aspirin.
How is the diagnosis of a heart attack confirmed in hospital?
When you arrive at the emergency room, a series of tests and evaluations will be carried out immediately. This process is critical to confirm the diagnosis and determine the direction of treatment.
The main methods used in the diagnostic process are the following:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and provides results within seconds. Certain changes in the ECG (e.g. ST elevation) indicate a complete blockage of a major blood vessel and the need for urgent intervention. Sometimes, especially in the early stages of a crisis or partial blockage, the ECG may be normal. Therefore, a normal ECG does not rule out a heart attack.
- Blood Tests (Cardiac Enzymes): When the heart muscle is damaged, a protein called “Troponin” leaks into the blood. Measuring the level of this protein in the blood is the “gold standard” method to confirm the diagnosis of a heart attack. Because it takes time for the troponin level to rise, the test is usually repeated upon admission to the hospital and a few hours later.
- Echocardiography (ECHO): This is an ultrasound of the heart. It shows whether part of the heart wall is contractile due to a heart attack, the pumping power of the heart (ejection fraction) and the condition of the valves.
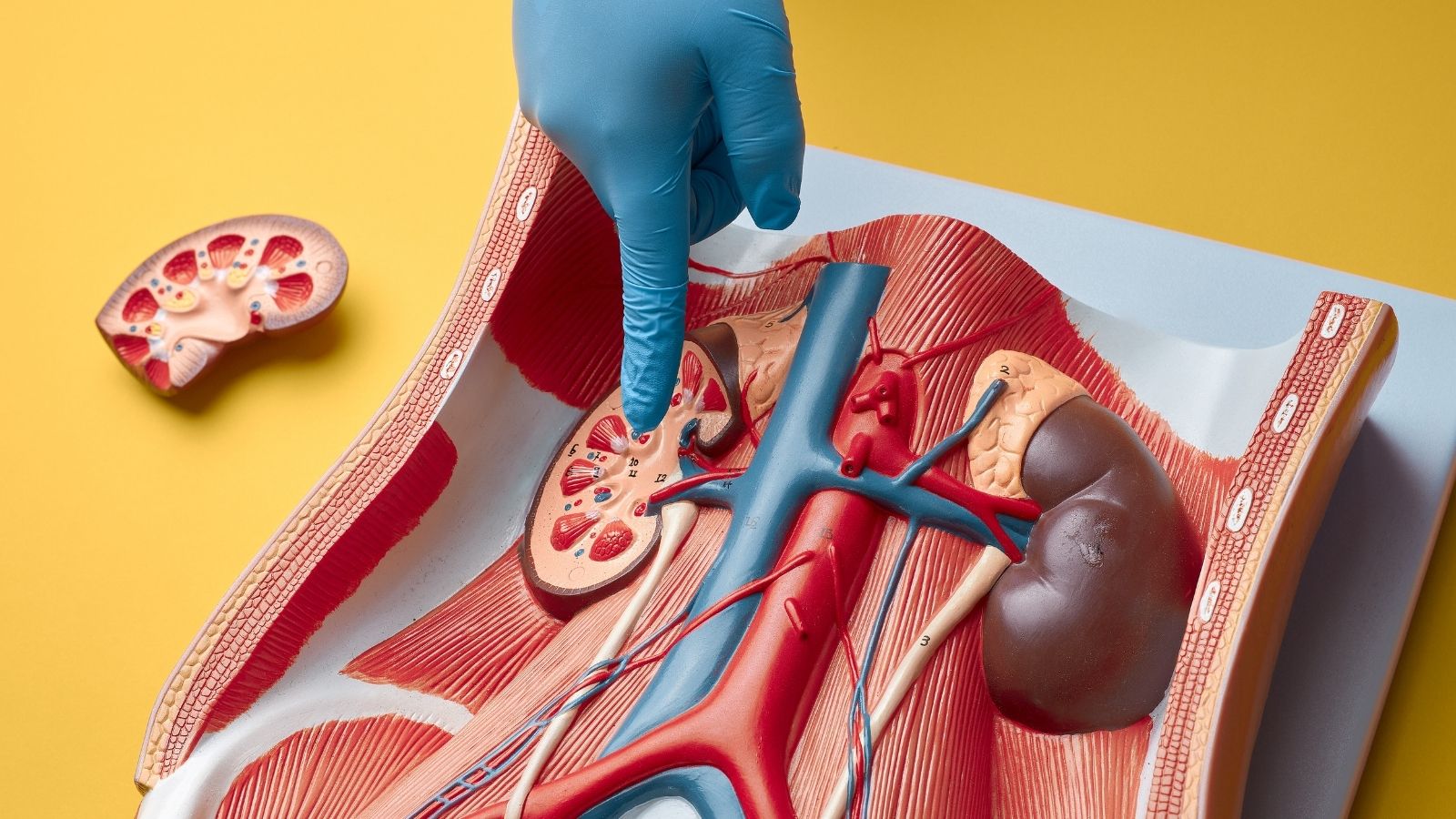
- Coronary Angiography: The most accurate method used for both diagnosis and treatment. A thin tube (catheter) is inserted through the groin or wrist to access the heart vessels. A dye that visualizes the inside of the vessels is injected and films are taken. In this way, it is clearly seen which vessel is blocked, where and to what extent.
The main goal of treatment in a heart attack is one: To open the blocked blood vessel as quickly as possible and restore blood flow. Medication and interventional/surgical methods are used for this purpose.
Which drug therapies are used in heart attacks?
In the treatment of a heart attack, medications are used both to solve the immediate problem and to protect the heart in the long term.
The drug groups that form the cornerstone of treatment are as follows:
- Anticoagulants (Antiplatelets: Aspirin, Clopidogrel, etc.)
- Blood thinners (Anticoagulants: Heparin etc.)
- Clot dissolving drugs (Thrombolytics – when angiography cannot be performed)
- Drugs that reduce the workload of the heart (beta-blockers)
- Cholesterol-lowering and plaque-stabilizing drugs (Statins)
- Blood pressure regulators and heart-protective drugs (ACE inhibitors)
- Vasodilators to relieve chest pain (Nitroglycerin)
What is angiography (PCI) and stenting in a heart attack?
Percutaneous Coronary Intervention (PCI), commonly known as angioplasty, balloon and stenting, is a non-surgical procedure to open a blocked heart vessel. Especially in major heart attacks (STEMI), this is the first-choice and life-saving “gold standard” treatment to open the blocked vessel.
In this procedure, when a blocked vessel is detected during coronary angiography, the blockage is bypassed with a wire with a tiny balloon at the end, which is advanced through the same catheter. The balloon is inflated at the site of the blockage, crushing the plaque against the vessel wall and opening the vessel. A tube made of wire mesh, often called a “stent”, is then placed in the same area to prevent the vessel from closing again. Most modern stents have a special coating that slowly releases medicine to prevent re-narrowing.
When and why is bypass (CABG) surgery necessary for a heart attack?
Coronary Artery Bypass Grafting (CABG), or bypass surgery, is an open heart operation. The logic of this surgery is that instead of trying to open the blocked artery, a new artery pathway is created to “bypass” the blocked artery, that is, to go around it. For this new pathway (graft), the patient’s own intrathoracic artery, an arm artery or a vein from the leg is usually used.
Angioplasty and stenting can be compared to a plumber unblocking a blocked water pipe: Fast, effective and targeted to the problem. Bypass surgery, on the other hand, is the approach of an urban planner or architect who reorganizes the entire traffic flow in an area. Instead of fixing the old clogged road, it is building a new highway next to it that will carry traffic smoothly for many years to come.
Bypass surgery usually offers a more permanent and superior solution in the following cases
- If there are widespread and severe blockages in several arteries of the heart.
- The main artery of the heart (left main coronary artery) is critically narrow.
- Patients with diabetes have multivessel disease.
- In cases where stent implantation is not technically feasible or previously implanted stents are blocked again.
- If an additional surgical problem such as valvular disease or an aneurysm has developed in the heart after a heart attack.
Bypass surgery may be more advantageous than a stent in preventing future heart attacks and improving long-term survival rates, especially in these complex patient groups. Based on your angiography results, the “Heart Team” of cardiologists and cardiac surgeons will decide which treatment is best for you.
Having a heart attack is not the end but the beginning of a new life in which you will prioritize your heart health. This process involves not only a physical but also a spiritual recovery.
Why is cardiac rehabilitation after a heart attack so important?
Cardiac rehabilitation is the most important and unfortunately the most neglected part of recovery after a heart attack. It is much more than just “take a walk” advice. This medically supervised program has been proven to reduce the risk of future heart attacks and mortality by up to 5%.
A cardiac rehabilitation program consists of three pillars.
- Individualized exercise planning: Exercises to safely strengthen your heart under the supervision of a doctor and physiotherapist, monitoring your heart rate and blood pressure.
- Patient education: Detailed information on topics such as heart-friendly nutrition, the importance of medications and combating risk factors.
- Psychological support: Counseling services to deal with fear, anxiety and depression, which are common after a heart attack.
What should I pay attention to in my diet after a heart attack?
Nutrition is the foundation of heart health. The aim is to keep blood pressure, cholesterol and weight under control. Think of your table as a medicine.
Here’s what you should include more of to protect your heart:
- Fresh vegetables (spinach, broccoli, tomatoes, etc.)
- Fruits (especially fibrous and colorful ones)
- Whole grains (oats, brown rice, whole wheat bread)
- Oily fish (Omega-3 sources such as salmon, sardines)
- Legumes (lentils, chickpeas, beans)
- Nuts (such as walnuts, almonds – unsalted)
- Olive Oil
Here’s what you should avoid or severely limit
- Processed meat products (salami, sausage, pepperoni)
- Fried foods and foods containing trans fats
- Sugary drinks and sweets
- Refined carbohydrates such as white bread, rice
- Packaged foods and pickles containing excess salt
- Full-fat dairy products and fatty cuts of red meat
When can I return to my normal life after a heart attack?
This depends on the size of the attack, the treatment and your general state of health. However, the main goal is to get you safely back to your normal life as soon as possible:
- Within a few weeks if you have a desk job, or 1-3 months if you have a job that requires physical strength.
- You can usually start driving after a few weeks, with your doctor’s approval.
- This is a subject that patients hesitate to ask but are very curious about. The general rule is that if you can climb two flights of stairs without difficulty, it is safe to return to sexual activity. This is usually a few weeks after the crisis.
- The cardiac rehabilitation program will give you the best guidance on when and how to start exercising.
Remember that one heart attack is proof that you have vascular disease. Treatments (stents or bypass) can put out the immediate fire, but it is up to you to protect the rest of the forest. By taking your medication regularly, adopting a healthy lifestyle and keeping up with your medical check-ups, you can turn this “second chance” into a long and healthy life.
Frequently Asked Questions
What is a heart attack?
A heart attack is when the blood supply to the heart muscle suddenly stops and the heart tissue is damaged. The medical name is “myocardial infarction”.
What causes a heart attack?
The most common cause is a blockage in one of the heart arteries. This usually occurs when a cholesterol plaque ruptures and a clot forms.
What are the symptoms of a heart attack?
Symptoms include chest pain, tightness, pain radiating to the left arm and jaw, shortness of breath, sweating, nausea and dizziness.
Do women have different heart attack symptoms?
Yes. Atypical symptoms such as nausea, weakness, back and neck pain are more common in women.
How to distinguish a heart attack from a panic attack?
In a panic attack, the pain is usually sharp and does not increase with movement. In a heart attack, the pain is more pressing and intensifies with physical activity. A definitive diagnosis is made with ECG and troponin test.
What to do in case of a heart attack?
112 should be called immediately, the patient should be seated and an aspirin should be chewed if he/she is not allergic to aspirin.
How is a heart attack diagnosed?
It is diagnosed with ECG, blood tests (especially troponin), echocardiography and angiography.
How is a heart attack treated?
The most common treatment is to open the blocked blood vessel. This is usually done with angioplasty and stenting. If necessary, bypass surgery may be performed.
How is life affected after a heart attack?
Recovery is possible in people with early intervention. However, lifestyle changes, medication and regular check-ups are essential.
Is a heart attack fatal?
It can be fatal without intervention. The chances of survival increase significantly with prompt diagnosis and treatment.
How to reduce the risk of heart attack?
Not smoking, eating a healthy diet, exercising regularly, and keeping blood pressure and cholesterol under control are effective measures.
Can a person have another heart attack?
Yes. A previous heart attack is a serious risk factor for subsequent attacks. Regular treatment and follow-up are necessary.
Can a heart attack happen at a young age?
Yes. Factors such as genetic predisposition, smoking, poor diet, stress and drug use increase the risk in young people.
Is there a difference between heart attack and stroke?
Yes. A heart attack affects the heart muscle, while a stroke affects brain tissue. Both are due to impaired blood flow but involve different organs.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.