Mitral stenosis is the narrowing of the mitral valve opening, which restricts blood flow from the left atrium to the left ventricle. It is most commonly a result of rheumatic heart disease, although congenital and degenerative causes also exist.
Hemodynamic consequences of mitral stenosis include elevated left atrial pressure, pulmonary congestion, and reduced cardiac output. Patients may experience fatigue, palpitations, and progressive shortness of breath, especially during exertion.
Complications such as atrial fibrillation, pulmonary hypertension, and right heart failure frequently develop in advanced stages. These secondary effects significantly increase morbidity and require close medical monitoring.
Treatment approaches range from medical therapy, including diuretics and anticoagulants, to interventional procedures such as balloon valvotomy or surgical valve replacement, depending on disease severity and patient condition.
| Causes | The most common cause is rheumatic fever; rarely congenital defects, mitral annular calcification |
| Risk Factors | History of rheumatic diseases, female gender, low socioeconomic status, previous infections |
| Symptoms | Shortness of breath increasing with exertion, palpitations, weakness, orthopnea, paroxysmal nocturnal dyspnea, hemoptysis |
| Diagnostic Methods | Opening sound and diastolic murmur on physical examination, echocardiography (the most important diagnostic tool), ECG, chest radiography |
| Treatment Options | Medical therapy (diuretics, beta blockers, anticoagulants), minimally invasive mitral valvuloplasty or open valve replacement |
| Complications | Atrial fibrillation, thromboembolism, pulmonary hypertension, right heart failure |
| Protective Measures | Early treatment of rheumatic fever, prevention of infections, regular cardiologic follow-up |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Mitral Valve Stenosis and How Does It Affect the Heart?
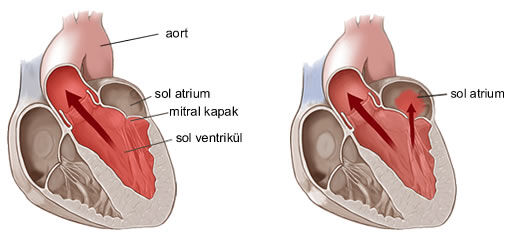
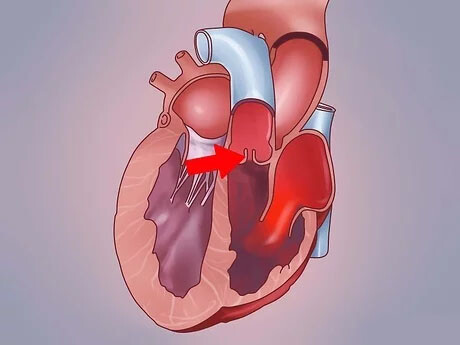
Imagine a door on the left side of our heart between the left atrium, where clean blood from the lungs is collected, and the left ventricle, the main chamber that pumps this blood throughout the body. This door is called the mitral valve. Its job is to ensure that blood flows at the right time and in the right direction, i.e. only from the atrium to the ventricle. A healthy mitral valve opens fully with each heartbeat, allowing blood to pass freely, and then closes tightly so that it does not leak.
So what happens when you have mitral valve stenosis? It can be likened to an old door that has rusted over time and the hinges are stuck. No matter how hard you try, the door will not open and it will not open wide. In mitral stenosis, the valves stiffen, thicken and stick together, leading to a narrowing of the valve opening.
This “stuck door” negatively affects the functioning of the heart in several ways. First, as blood tries to pass through a narrow opening, it pools behind the door, in the left atrium. This build-up increases the pressure inside the chamber, causing its walls to stretch and expand over time. Second, the heart has to work much harder and contract more strongly than usual to push the blood through this narrow doorway. This is like running a marathon, which exhausts the heart. The third, and perhaps the one that causes us to feel the symptoms the most, is that not enough blood can get to the left ventricle. If the left ventricle, the body’s main pump, receives too little blood, the amount of oxygen-rich blood pumped to the body and organs is reduced. This is the basis for complaints such as fatigue, weakness and reduced effort capacity.
The accumulation of blood in the left atrium also causes a backward pressure in the pulmonary vessels. This condition is called “pulmonary congestion” and is the main cause of shortness of breath, especially during exertion or when lying on your back.
What are the Main Causes of Mitral Valve Stenosis?
Understanding the underlying causes of mitral valve stenosis is crucial to determine the right treatment strategy. Some of these causes are very common, while others are more rare.
The most common cause is acute rheumatic fever, which is still important especially in our country. This is an immune system reaction to untreated childhood throat infections caused by the streptococcus bacteria known as “beta germs”. In fighting the germ, the body mistakenly attacks its own tissues, especially the heart valves. The mitral valve is the most affected valve. The damage caused by rheumatic fever does not appear immediately. Over the course of many years, a silent process of thickening, hardening and adhesion of the valves progresses. Symptoms usually become apparent 20-30 years after the first infection, in middle age. For this reason, many patients do not realize that their heart problems in adulthood can be caused by a simple sore throat in childhood.
Another important cause is age-related valve calcification. Just like our blood vessels, calcium, or lime, can build up on our heart valves with age. this condition, called “degenerative mitral stenosis”, is more common in people aged 70 and over and causes the valves to lose their elasticity.
Other more rare causes include:
- Congenital valve structure disorders
- Radiotherapy (radiation therapy) applied to the chest area for cancer treatment
- Some rheumatic and immune system diseases such as lupus
- Previous valve infections (infective endocarditis)
Knowing the cause directly affects the treatment options. For example, flexible valves due to rheumatic fever usually respond very well to balloon dilatation, while surgery may be the only option in age-related stenosis where calcification is at the forefront.
What are the Symptoms of Mitral Valve Stenosis?
Mitral valve stenosis can progress silently for many years without any symptoms. When symptoms do appear, they usually start gradually and become more severe over time. As patients gradually get used to these symptoms, they may take them for granted or accept them as normal, saying “I am old now”.
The most common symptoms are:
- Shortness of breath with exertion
- Fatigue and weakness more quickly than usual
- Palpitations or heart palpitations
- Swelling in the ankles and legs
- Dry cough, especially at night
- Feeling of pressure or discomfort in the chest
- Dizziness or darkening of the eyes
The most typical of these symptoms is shortness of breath. Initially, this only occurs when climbing stairs or hills, but as the disease progresses, it can be felt while walking in a straight line, even at rest. Some patients wake up at night because of shortness of breath when lying on their backs, or they can only get comfortable when lying high with a few pillows. This is a sign of fluid accumulation in the lungs and indicates that the disease has reached an important stage.
Palpitations are usually caused by a rhythm disorder called atrial fibrillation, which is a complication of stenosis. It is felt as an irregular and often rapid beating of the heart. This condition is not only uncomfortable but also increases the risk of stroke and should be taken seriously.
If you experience sudden and severe symptoms such as the following, you should seek medical attention immediately:
- Severe chest pain
- Fainting
- Shortness of breath that starts suddenly and does not go away even when you are sitting
- Symptoms of paralysis such as impaired speech, weakness in the arm or leg
These symptoms may indicate a life-threatening condition.
How is Mitral Valve Stenosis Diagnosed?

If we suspect mitral valve stenosis when we listen to a patient’s complaints, we perform a series of examinations to confirm the diagnosis and determine the severity of the condition. This process is like putting together the pieces of a jigsaw puzzle.
One of the first and most important steps is the physical examination. When we listen to the heart with a stethoscope, we can hear very typical sounds characteristic of this disease. The “opening snap” of the valve as it opens and the murmur of blood passing through a narrow opening are important clues for an experienced physician.
However, the gold standard method that confirms the diagnosis and allows us to plan treatment is Echocardiography (ECHO), an ultrasound of the heart. This painless and harmless test allows us to take a detailed movie of your heart and valves. With ECHO, we can clearly see how thick the valves are, how calcified they are and how far they can open. By measuring the valve area in millimeters, we objectively determine the degree of stenosis (mild, moderate, severe). We also assess the strength of the heart’s contraction, the condition of other valves and pulmonary pressure.
Sometimes when more detailed imaging is needed, especially if we are planning an intervention or surgery, we use the Transesophageal Echocardiography (TEE) test through the esophagus. Because this test shows the valve much more closely, it is particularly vital in determining whether valve repair is possible and to see for certain whether there is a small clot in the left atrium that could cause paralysis.
Other ancillary tests we use in the diagnostic process include
- Electrocardiogram (ECG)
- Chest X-ray
- Stress ECG or Stress Echocardiography
- Cardiac Catheterization (heart angiography)
What Complications Can Mitral Valve Stenosis Lead to If Left Untreated?
Untreated mitral valve stenosis can create a domino effect over time, leading to serious and life-threatening problems. These complications clearly show why the disease should be taken seriously.
The most common complications that can lead to the most dangerous consequences are the following:
- Atrial Fibrillation: This is when the upper chambers of the heart (atria) lose their normal rhythm and vibrate irregularly and rapidly.
- Blood clot and stroke: During atrial fibrillation, blood pooling in the atria creates an ideal environment for clot formation. A clot fragment can travel through the bloodstream to the brain and block a blood vessel, causing a stroke with permanent disability.
- Pulmonary Hypertension: This is an increase in blood pressure in the arteries of the lungs to dangerous levels. This puts excessive strain on the right side of the heart.
- Right Heart Failure: The right side of the heart, which has to constantly work against high pressure, gets tired, weakens and becomes unable to do its job.
- Pulmonary Edema: It is a severe shortness of breath that occurs as a result of excessive fluid accumulation in the lungs and requires urgent intervention.
What are the Treatment Approaches for Mitral Valve Stenosis?
There is no “one-size-fits-all” treatment for mitral valve stenosis. The treatment plan is individually tailored according to many factors such as the severity of the stenosis, the age of the patient, the symptoms and the anatomical structure of the valve. Our aim is to solve the mechanical problem in the door, relieve the heart’s burden and allow the patient to lead a normal life.
Our basic treatment approaches are categorized under three main headings:
Medication Therapy: It is used to control symptoms and prevent complications.
Interventional Methods (Non-Surgical): Balloon valve dilatation (PMBK) is performed in suitable patients.
Surgical Interventions: It includes valve repair or valve replacement surgeries.
Which or which of these options to use is decided jointly by a “Heart Team”, usually consisting of a cardiologist and a cardiac surgeon, in consultation with the patient.
Does Medication Solve Mitral Valve Stenosis?
This is one of the most common questions patients ask and the answer is clear: No. Medication does not correct the mitral valve stenosis itself, that is, the mechanical narrowing of the valve. It does not repair the rusted door. But it plays a vital role in alleviating symptoms and protecting the heart when living with this mechanical problem.
The main goals of drug treatment are:
Controlling Heart Rate: Medications such as beta blockers slow down the heart rate. This both reduces palpitations and allows the heart to fill more efficiently with each beat.
Removing Excess Fluid from the Body: Diuretics (diuretics) relieve shortness of breath and swelling by removing fluid accumulated in the lungs and legs.
Preventing Clot Formation: Especially in patients who develop atrial fibrillation, the use of blood thinners (anticoagulants) is mandatory to prevent the risk of stroke.
Drug therapy is the mainstay of treatment, especially for patients with mild stenosis or who are not suitable for interventional or surgical treatment for any reason. In patients with severe stenosis, it often acts as a bridge to surgery or a balloon procedure.
When to Decide on Surgery for Mitral Valve Stenosis?
The most important factor in deciding on surgery for mitral valve stenosis is the right timing. It is necessary to decide on surgery before irreversible damage to the heart occurs and before pulmonary hypertension occurs:
- In the presence of severe stenosis with severe symptoms (shortness of breath, fatigue, etc.) that limit the patient’s daily life.
- ECHO shows that pulmonary artery pressure has increased to dangerous levels, even if the patient has no symptoms.
- In cases where the structure of the valve (such as severe calcification) is not suitable for balloon dilatation.
- If the balloon procedure has been tried but failed or the valve has narrowed again over time.
- Mitral valve stenosis is accompanied by another heart condition that requires surgery (e.g. coronary bypass or other valve disease).
The decision for surgery is taken together with the patient, taking into account the patient’s individual situation, risk factors and expectations.
Is Valve Repair or Replacement Preferred in Mitral Valve Stenosis Surgery?
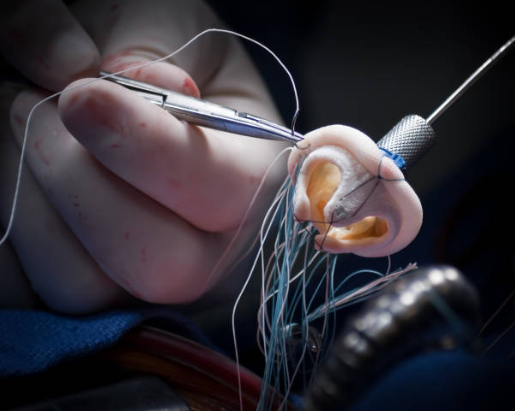
The first question that comes to mind when the decision for surgery is made is: “Will the valve be repaired or replaced?” The basic philosophy of modern heart surgery is to always preserve the patient’s own tissue. Because no artificial valve can replace the patient’s own natural valve. Therefore, if the structure of the valve is suitable, our first and foremost choice is always valve repair.
Valve Repair: This is the art of solving the problem with the precision of a sculptor, using the patient’s own valve tissue. Repair of mitral valve stenosis is a surgical procedure in which the edges of the valve, which are usually adherent, are carefully cut open (open commissurotomy). If necessary, lime deposits are removed from the valves and thickened tissues are thinned. The biggest advantage of repair is that it protects the patient from the need for lifelong blood thinners and the risks associated with prosthetic valves.
Cover Replacement: Sometimes the valve may be damaged beyond repair due to advanced calcification or structural deterioration. In this case, the damaged valve is completely removed and replaced with an artificial (prosthetic) valve. Prosthetic valves can be mechanical or biological (tissue). This decision is based on the patient’s age, lifestyle and medical condition. For patients who have no chance of repair, valve replacement is an excellent option that saves lives and improves quality of life.
What are the Modern Surgical Techniques Used in Mitral Valve Stenosis Surgery?
Today, there are different surgical approaches to perform mitral valve stenosis surgery. While traditional open heart surgery used to be the only option, we can now offer our patients much more comfortable options thanks to minimally invasive and robotic techniques.
The main surgical approaches used are as follows:
- Open Heart Surgery (Sternotomy): The traditional method in which the sternum is cut across the front. It provides the widest field of view to the heart and is still the gold standard, especially in complex cases where multiple procedures (e.g. both valve and bypass) are to be performed.
- Minimally Invasive Heart Surgery: In this technique, the breastbone is not cut. The operation is performed through a small incision of about 5-6 cm, usually on the right side of the chest, at the armpit level. Through this small incision, special instruments and a camera are used to access the heart and repair or replace the valve. The biggest advantages of this method are much less postoperative pain, faster recovery, better cosmetic results and the ability to return to daily life much earlier.
- Robotic Assisted Heart Surgery: It is the most advanced technology of minimally invasive surgery. The surgeon performs the surgery by directing robotic arms from a console. The robotic arms, which are advanced through a few small (1-2 cm) holes in the chest, perform the surgery with much more precise movements than the human hand under 3D and magnified images. It ensures great success and comfort, especially in complex valve repairs.
In eligible patients, minimally invasive or robotic surgery is preferred because of the rapid recovery and comfort it offers.
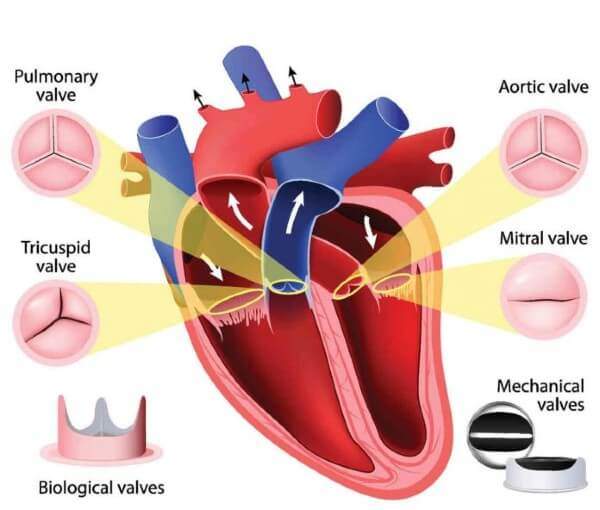
How to Choose a Prosthetic Valve in Mitral Valve Stenosis Surgery?
Once the decision to replace the valve has been made, the next important question we need to answer together with the patient is which type of prosthetic valve to choose. We can liken this choice to choosing a car tire: Performance tires that last a lifetime but require special care (blood thinners) (mechanical valve) or standard tires that are easy to maintain but have a set lifespan and need to be replaced in due time (biological valve)?
Mechanical Covers: They are made of very durable materials such as carbon and theoretically last a lifetime. Their most important feature is that they require lifelong use of blood thinners (Warfarin) to prevent clot formation. They are generally preferred in younger patients (under 60-65 years of age).
Biological (Tissue) Valves: These are tissue valves obtained from bovine or porcine heart membranes by special processes. Their biggest advantage is that they do not require the use of blood thinners. However, they tend to wear out over time and may require re-intervention (a second surgery or valve-in-valve placement by angiography) in an average of 10-20 years. They are generally preferred in elderly patients or in people who cannot use blood thinners.
This decision is made with the patient after discussing the advantages and disadvantages in detail, taking into account the patient’s age, lifestyle (active sports, pregnancy plan, etc.), general health status and personal preferences.
What awaits me during the recovery period after mitral valve stenosis surgery?
Postoperative recovery is as important as a successful surgery. Although this process varies according to the type of surgery performed, it is usually faster and more comfortable than our patients expect.
The first day after surgery is usually spent in the intensive care unit, where your vital functions are closely monitored. You will then be transferred to the ward, where you will be encouraged to move slowly (first sitting, then walking). Breathing exercises accompanied by physiotherapists will help clear your lungs.
The hospital stay after minimally invasive or robotic surgery is usually 3-5 days. After traditional open surgery, this period may be a few days longer.
There are some important points to be aware of after discharge home:
- Keeping the wound clean and dry
- Regular use of prescribed medications (including painkillers)
- Following the activity program determined by your doctor
- Paying attention to a healthy and balanced diet
- Keeping scheduled control appointments
Participating in cardiac rehabilitation programs in the post-operative period will not only help you recover faster physically, but also help you learn how to maintain your heart health in the long term.
Frequently Asked Questions
What is mitral valve stenosis?
Mitral valve stenosis is a condition in which the mitral valve between the left atrium and left ventricle of the heart narrows, making blood flow difficult.
Why does the mitral valve narrow?
The most common cause is valve damage due to rheumatic fever. Rarely, it can also develop as a result of congenital or age-related arthritis.
What are the symptoms?
Shortness of breath, fatigue, palpitations, coughing and rarely fainting are the main symptoms of mitral valve stenosis.
How is mitral valve stenosis diagnosed?
The diagnosis is clarified by cardiac examination, ECG, chest radiography and especially echocardiography.
In which age group does this disease occur?
It is usually diagnosed between the ages of 30-50; however, it may develop due to rheumatic fever in childhood.
Is mitral valve stenosis dangerous?
Yes, if left untreated, it can lead to serious problems such as heart failure, arrhythmias and stroke.
Does mitral valve stenosis cause heart failure?
Yes, valve stenosis can increase the burden on the heart, leading to heart failure over time.
What are the treatment options?
In mild cases, medication is used, and in advanced cases, minimally invasive surgery with valvuloplasty or valve replacement is performed.
What is mitral balloon valvuloplasty?
The stenotic valve is widened with a balloon. It is a non-surgical method applied through a catheter. It is often not successful because the stenotic valve may rupture and cause mitral valve insufficiency.
Is mitral valve replacement a difficult operation?
It is an operation with a high success rate with minimally invasive surgical techniques. If necessary, a mechanical or biological cover is installed.
Do I need lifelong medication after valve replacement?
If a mechanical valve is implanted, lifelong use of blood thinners may be necessary. In the biological valve, this period is limited.
Does mitral valve stenosis prevent sports?
The decision is made according to the degree of stenosis. In severe stenosis, effort restriction may be required.
Is mitral valve stenosis risky during pregnancy?
Yes, pregnancy should be carefully monitored as it increases cardiac load. If necessary, pre-pregnancy intervention should be planned.
Is mitral valve stenosis a progressive disease?
Yes, it usually gets worse over time. Regular follow-up is therefore very important.
Which doctor should you consult?
The cardiologist is the first point of contact for diagnosis and follow-up. Cardiovascular surgery support is obtained if necessary.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.