Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic method that uses strong magnetic fields and radio waves to obtain detailed images of organs and tissues. It helps physicians evaluate structural abnormalities, detect diseases early, and plan treatment strategies effectively.
MRI indications include neurological conditions, musculoskeletal problems, cardiovascular diseases, and oncological assessments. It provides high-resolution images without radiation, making it safer than many imaging techniques, particularly in recurrent examinations.
Functional MRI and contrast-enhanced MRI are advanced methods that allow evaluation of brain activity, blood flow, and tissue viability. These techniques are widely used in neurology, cardiology, and oncology to support accurate diagnoses.
MRI safety is generally high; however, patients with pacemakers, cochlear implants, or metal fragments in the body may face contraindications. Prior consultation with a physician is essential to ensure safe and effective imaging.
| Medical Name | Magnetic Resonance Imaging (MR, MRI) |
| Frequent Use Areas | – Brain, spine, joints, heart and vessels, abdominal organs – Diagnosis of tumors, masses, infections and vascular diseases |
| Causes | – The need for detailed soft tissue and organ evaluation- Insufficient information can be obtained with other imaging modalities |
| Risk Factors | – Metallic implants in the heart or body (pacemaker, stent, prosthesis, etc.) – Fear of enclosed spaces (claustrophobia) – Pregnancy (attention in the first 3 months) |
| Complications | – Allergic reaction to contrast media (rare)- Risks associated with metallic implants- Discomfort due to prolonged immobilization |
| Diagnostic Methods | – Preliminary evaluation with clinical examination and other imaging methods |
| Treatment Methods | – MRI is a diagnostic method, not a treatment |
| Prevention Methods | – Removal of metal objects- Evaluation of renal function if contrast media is to be used- Precautions for claustrophobia |
What is MRI and how does it work?
To answer the question of what is Magnetic Resonance (MRI) in the most understandable way, we can liken this technology to creating a map by asking questions to the water molecules in our body and getting answers from them. Contrary to popular belief, the principle of MRI does not use radiation or X-rays; it is based on a giant magnet, radio waves and the water in our bodies.
A very large part of the human body is made up of water. Inside each water molecule are hydrogen atoms. You can think of the nuclei of these hydrogen atoms as billions of tiny spinning tops. This spinning gives them a property called “magnetic moment”, meaning that each one acts like a tiny magnet. Under normal conditions, these tiny magnets are completely scattered throughout our body, like marbles in a bag, facing in random directions.
When you wonder how an MRI is performed, the process starts with aligning these scattered balls. When the patient lies down inside the tunnel-shaped MRI machine, its extremely powerful magnet is activated. This magnetic field is so strong that it aligns a significant number of the billions of tiny magnets (hydrogen nuclei) in our bodies and makes them all face in the same direction. Just like a commander’s command to “turn right” makes all soldiers turn in the same direction. But this alignment is not static; the atoms continue to make a vibrating wobble around this main axis. The atoms of each tissue make this movement at a frequency unique to them.
The next step is to give these regular “soldiers” a new command. The device sends a radio wave at the same frequency as the frequency at which atoms vibrate. the word “resonance” refers to the perfect match of these frequencies. The hydrogen atoms that receive this radio wave absorb the energy and temporarily “tip” sideways from their aligned main axis.
The magic moment that creates the image is when this radio wave is turned off. The energized and distracted atoms quickly try to return to their original regular position. During this “relaxation” process, they emit their excess energy as a weak signal, like a whisper. Highly sensitive receivers (antennas) placed around the device hear these whispers. A powerful computer system analyzes the millions of whispers and calculates where in the body and what kind of tissue they come from. It combines this data to create incredibly detailed, black-and-white cross-sectional images of your organs, muscles and blood vessels. In short, MRI is a technology that draws a picture by listening to the behavior of water inside the body.
Why is an MRI performed?
The answer to the question of why an MRI is performed lies in the unique information provided by this technology. It is far superior to other methods, especially in visualizing soft tissues. For a cardiovascular surgeon, MRI provides valuable information to make critical decisions before, during and after surgery. The main reasons for requesting an MRI scan are as follows:
- Assessing the health of the heart muscle
- Measuring the damage caused by a heart attack
- Finding the underlying cause of heart failure
- Precisely measuring leaks in heart valves
- Detailed examination of congenital heart diseases
- Detecting problems in large vessels such as the main artery (aorta)
- Mapping vascular structure before procedures such as bypass or stenting
- To investigate tumors or masses in or around the heart
- Monitoring the success of the treatment and the healing process of the heart
What Do T1 and T2 Images Used in MRI Mean?
The terms T1 and T2, often seen in MRI reports, are actually similar to different camera settings. Each setting highlights a different detail. The process of hydrogen atoms returning to their former calm state (relaxation) after being stimulated by radio waves occurs at different speeds in different tissues. The T1 and T2 sequences use these speed differences to create contrast.
T1-weighted images are often used to clearly see the details of anatomy, i.e. the normal structure and boundaries of organs. In this sequence, fat-containing tissues appear bright (white) because they rapidly radiate energy to their surroundings. Tissues and fluids with a high water content appear darker (black). T1 images are ideal for understanding the shape and size of an organ and its relationship to neighboring structures. T1-weighted images, especially after intravenous administration of contrast material (medication), illuminate blood supply tissues or abnormal structures, making them more prominent.
T2-weighted images are our number one aid in detecting pathology, the diseased state. In this sequence, the opposite is true; tissues containing water and fluid appear bright (white). When there is inflammation, infection or tissue damage in the body, there is fluid accumulation in that area called edema. This fluid build-up shines like a light bulb on T2 images and immediately identifies the location of the problem. For example, when we suspect inflammation of the heart muscle (myocarditis), the bright areas we see in the heart muscle on T2 images show us the edema there, strengthening the diagnosis.
Why is it important that an MRI is radiation-free?
One of the most fundamental and invaluable advantages of MRI is that it does not use ionizing radiation. Computed tomography (CT), angiography and nuclear medicine methods (such as SPECT, PET) use X-rays or gamma rays to create images, the uncontrolled use of which can carry long-term risks. MRI, on the other hand, only works with magnetic fields and radio waves, which have no known permanent damage to the human body. This safety feature makes MRI an alternative for some patient groups. There are situations where it is particularly important that the MRI is radiation-free:
Pediatric patients: Children’s developing tissues are more sensitive than adults to the potential long-term adverse effects of radiation.
Those with congenital heart disease: These patients usually require lifelong follow-up and MRI can be performed repeatedly without worrying about radiation accumulation.
Chronic patients requiring frequent follow-up: It protects the patient from radiation during serial photography to monitor the progression of conditions such as aortic dilatation (aneurysm) or heart muscle disease.
Young adults: It keeps the lifetime radiation dose to zero in young patients with valve or heart muscle conditions that may require decades of follow-up.
Certain periods of pregnancy: It can be considered as a radiation-free option, especially after the first trimester, when another imaging method is risky for the mother or baby.
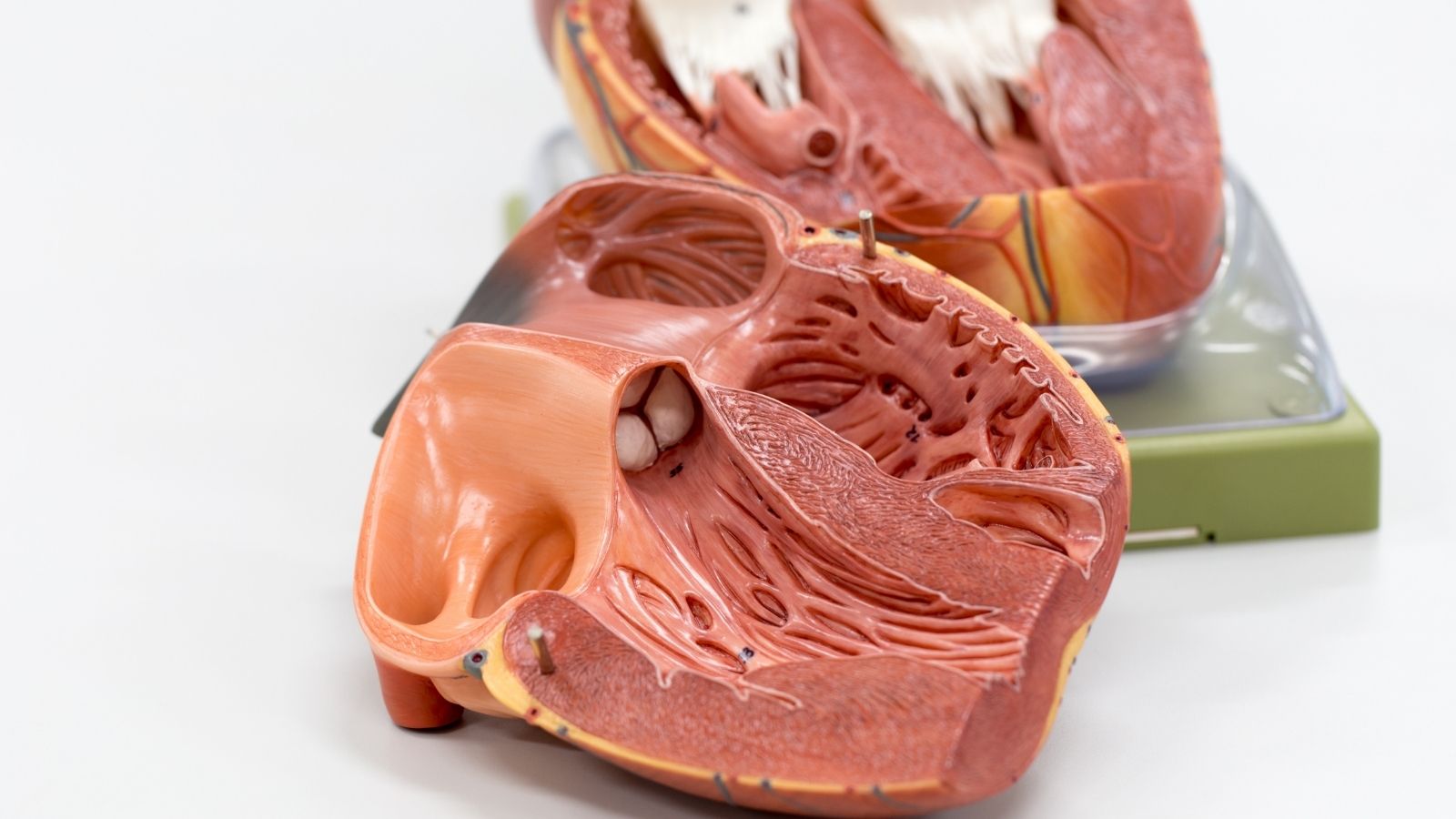
What is Cardiac MRI and Why is it Considered the Gold Standard?
Cardiac MRI (CMR) is an application of MR technology specifically optimized for imaging the moving and complex structure of the heart and the large vessels connected to it. Today, it is the most accurate and reliable method for measuring the volumes of the chambers of the heart (ventricles and atria), the mass of the heart muscle and, most importantly, the pumping power of the heart (ejection fraction). It is therefore considered the “gold standard” in scientific circles.
The reason for this superiority is the measurement technique. Echocardiography, an ultrasound of the heart, uses geometric formulas to estimate volume from two-dimensional images taken from certain angles. However, these estimates can be misleading in a heart that has suffered a heart attack or is deformed for some other reason. Cardiac MRI, on the other hand, scans the entire heart from its base to its apex in successive, very thin slices, like slicing a loaf of bread. By summing the volumes of these slices one by one, it directly measures the true, three-dimensional volume of the heart. This hypothesis-free and direct measurement makes the results much more precise and reproducible. This sensitivity is invaluable in showing whether a treatment is working or not, or whether a disease is progressing, by detecting even the smallest changes.
Some of the key and critical measurements obtained with cardiac MRI are:
- The volume of the heart when it fills with blood (end-diastolic volume)
- The volume remaining in the blood after pumping (end-systolic volume)
- The amount of blood pumped in each beat (Stroke volume)
- Percent pumping power of the heart (Ejection fraction – EF)
- Total weight and thickness of the heart muscle (Myocardial mass)
Cardiac MRI is also the method that most accurately measures the right ventricle, which is very difficult to evaluate with other methods, especially due to its complex half-moon-shaped structure.
Why an MRI after a Heart Attack or in Heart Failure?
The most revolutionary feature of cardiac MRI is that it shows not only how well the heart is pumping, but also why the heart muscle tissue is working well or poorly. It is like performing a bloodless biopsy without touching the heart. The most basic and powerful technique used for this purpose is “Late Gadolinium Enhancement” (LGE).
The principle of this method is based on the different behavior of an intravenously administered contrast agent (drug) called “gadolinium” in healthy and damaged heart muscle tissue. Healthy heart muscle cells are tightly packed together and their cell membranes are intact. Therefore, the contrast medium cannot penetrate these cells and is quickly washed out of the tissue. In the area that has been damaged by a heart attack or other cause, the cell membranes have broken down and the intercellular space has widened. The contrast medium fills this enlarged area and cannot be easily washed out due to damaged capillaries.
During the scan, 10-15 minutes after the contrast medium is administered, a special imaging technique is applied. With this technique, the signal from healthy heart muscle is erased by the computer and these areas appear completely black. Damaged, i.e. dead or scar tissue, in which a large amount of contrast material has accumulated, glows bright white. The resulting image offers a striking contrast between intact heart muscle (black) and dead tissue (white).
This information is vital for a cardiovascular surgeon. In a patient who is scheduled for bypass surgery, it allows us to understand whether the area of heart muscle supplied by the blocked vessel is alive or completely dead. If the muscle is completely dead, it will be useless to open that vessel. By making this “viability” analysis in the most accurate way, KMR guides us in determining which patient will benefit from surgery.
The distribution of the LGE pattern in cardiac muscle also provides valuable information about the origin of the disease.
Ischemic Pattern (Due to Vascular Occlusion): The damage starts from the inner surface of the heart muscle and is limited to the irrigation area of a specific coronary artery.
Non-ischemic Pattern (Due to Muscle Specific Diseases): The damage is distributed in the center of the muscle, on its outer surface or in a patchy distribution that does not correspond to a vascular area.
This distinction can reveal the cause of the heart failure (e.g. myocarditis, sarcoidosis, amyloidosis), which can lead to a completely different direction of treatment.
What is MRI Angiography (MR Angiography) and What is the Difference Between MR and MRI?
MR Angiography (MRA) is a specialized MR technique designed to image blood vessels. Unlike conventional angiography, where a catheter (a thin tube) is inserted through the groin vein, this is a completely external and non-invasive procedure. MRA can be performed in two main ways: Sometimes no medication is administered and the vessels are imaged using only the signal difference between the flowing blood and the fixed tissue. For higher resolution and detail, a gadolinium-based contrast agent is usually administered intravenously.
the question “the difference between MRI and MRI” also often comes to mind. In fact, there is no difference between the two. MRI stands for “Magnetic Resonance Imaging” and is the full scientific name of the method. MR or MRI is the more common and shorter name of this method used in everyday language. Angiography is a specialized sub-application of this technology used to visualize blood vessels.
MRA is especially used to evaluate large vessels such as the main artery (aorta) and leg arteries. For vascular surgeons, MRA provides a road map. In a patient with a blockage in the leg arteries, MRA allows us to see in three dimensions where the stenosis is located, how long a segment it is blocking and the condition of the vessels beyond the blockage. This information is critical for planning where and how to suture the vascular graft in the bypass surgery.
Why is MRI Important in Aortic Vessel Diseases?
The aorta is the main artery that comes from the heart and distributes clean blood throughout the body. Aneurysms (ballooning) and dissections (tears in the inner wall) in this vital artery are urgent and serious conditions. MR Angiography (MRA) plays a critical role in the diagnosis, follow-up and surgical planning of these diseases. Although tomography is usually the first choice in emergencies due to its speed, MRA is an invaluable alternative in stable patients, especially in lifelong follow-up, because it is radiation-free.
The main information that MRA provides for surgical planning in a patient with aortic dissection (rupture) is as follows
- Precise points where the tear starts and ends
- Two blood vessel pathways (true and false lumen) formed as a result of a tear
- Whether the tear affects the vessels of the brain, arms or legs
- Whether there is clot formation along the tear line
This information is essential to determine the type, urgency and strategy of surgery. In aortic aneurysms, MRA helps us decide which of the open or closed (endovascular) surgery methods is appropriate by mapping the largest diameter of the aneurysm, its length and its relationship with the kidney or intestinal vessels in three dimensions.
How long does an MRI scan take?
there is no single answer to the question “How long does an MRI take?” that is valid for everyone. The duration depends entirely on the area of the body being imaged, the complexity of the disease being investigated and the specific imaging techniques to be used.
To give a general time frame, most MRI scans are completed between 30 and 90 minutes. For example, the answer to the question “how long does a brain MRI take?” is usually 30-45 minutes. However, a more detailed brain MRI that investigates special conditions such as migraine, tumors or epilepsy and requires the use of contrast agents or additional sequences can take up to an hour or more. An MRI of a joint such as a knee or shoulder is usually finished in 30-40 minutes, while an MRI of the heart is one of the longest. A comprehensive cardiac MRI can take 60 to 90 minutes, as the heart is constantly moving and many different measurements are taken, including both function and tissue structure. It is vital for image quality that the patient remains as still as possible during these periods.
What happens during an MRI and why is the MRI taken at night?
For patients, the MRI experience can sometimes be worrying. Knowing in advance how the process works greatly reduces this anxiety. On the day of the scan, you will be asked to remove all metal objects (jewelry, watches, glasses, hearing aids, clothes with metal buttons) and you will be given a metal-free hospital gown. If a contrast medium is to be used, an IV will be started in your arm.
During shooting, you lie down on a motorized table, which slowly slides into the tunnel-shaped part of the device. When the scanning starts, the device makes a very loud and rhythmic beating, clattering and buzzing noise. These noises are caused by the rapid opening and closing of the magnetic fields to create the image and are normal. To reduce these noises, you will be given earplugs or headphones with music playing on them. For shots of the heart or abdomen, the technician will give you regular commands over the intercom, such as “breathe in, breathe out, hold your breath”. These breath-holding moments, usually 15-20 seconds, freeze the movement of the organs, allowing clear images to be taken.
So “why is MRI done at night?” The answer to this question is not purely medical but logistical. MRI devices are very expensive investments and the number of patients that can be seen during the day is limited due to the long duration of a scan. In order to maximize the efficiency of these valuable devices and meet the high demand for appointments, hospitals usually operate them on a 24/7 basis. For this reason, some non-urgent patients may be scheduled for appointments during the quieter hours of the night or early morning.
There are some important points to consider during the shoot:
- Remain as still as possible throughout the shoot
- Carefully follow the technician’s breathing commands
- If you have a fear of confined spaces (claustrophobia), mention this when making an appointment
- Using the emergency button that is handed to you in case of any inconvenience
Can an MRI be Performed in the Presence of Metal in the Body?
In the past, the presence of any metal implant in the body was seen as an absolute barrier to MRI. There was concern that the strong magnet could attract the metal and cause damage. However, thanks to revolutionary developments in both implant technology and security protocols, this situation has changed radically. MRI can now be performed safely with many metal implants.
The MR safety status of implants available in the body today is as follows.
Coronary Stents All modern stents (with or without medication) implanted in the heart vessels are MR compatible. They are made of materials such as titanium and cobalt-chromium, which are not affected by magnetic fields, so there is no risk of displacement or heating. An MRI can be safely performed even immediately after stent implantation.
Prosthetic Heart Valves: All surgically implanted mechanical or biological prosthetic heart valves and valve repair rings (annuloplasty rings) are MR compatible. The structure of these implants is robust enough to withstand the force of a magnetic field compared to the force of the heart’s own contraction.
Pacemakers and Shock Devices (ICDs): This is the group to be most careful with. Older generation pacemakers are still an obstacle for MR. However, the vast majority of pacemakers and ICDs manufactured today are designed to be “MR-Conditional”. This means that under certain conditions (such as setting the device to a specific MR mode, shooting at a specific magnetic field strength), the patient can safely undergo MRI. This procedure must be performed with a strict protocol in which the cardiology and radiology departments work together, the device is reprogrammed before and after the procedure, and the patient is closely monitored throughout the procedure.
Is the drug (contrast agent) used in MRI safe?
In some MRI scans, “gadolinium-based contrast agents” (GBCA) are injected intravenously to improve image quality and sharpen the distinction between tissues. These agents are generally quite safe and have a much lower risk of allergic reactions than the iodinated contrast agents used in tomography. However, as with any medical practice, it is useful to be aware of some potential, albeit rare, risks:
Here is what you need to know about these substances:
Allergic Reactions: The risk of serious allergic reactions is extremely low. Usually mild and temporary side effects such as nausea, headache or a short-lived feeling of coldness at the injection site may occur.
Effect on the Kidneys: In the past, some older types of gadolinium agents, especially those used in patients with severe renal insufficiency, have been shown to cause a serious side effect called “Nephrogenic Systemic Fibrosis”. However, with the new generation of more stable contrast agents used today, this risk has almost completely disappeared. However, you should always inform your doctor if you have a known kidney disease.
Gadolinium Accumulation: In recent years, it has been discovered that a very small amount of these contrast agents can accumulate in tissues such as brain and bone after repeated use. However, extensive research to date has not proven that this accumulation causes any clinical disease or symptoms in patients with normal kidney function.
What is the Evaluation 44 written on the result of an MRI?
questions such as “What does brain MRI assessment 44 mean?” or “What does MRI result assessment 44 mean?” arise from a natural curiosity about the technical phrases patients see in their reports. However, there is no universal and single answer to this question that can be learned from the internet or anyone else, and it is not right to investigate it in this way.
In radiology reporting, internationally standardized classification systems are used for some conditions (such as the BI-RADS system for mammography). However, a specific code or phrase such as “evaluation 44” can often be an internal coding, a billing code or a short name for a technical detail that is unique to that hospital or the laboratory writing the report. This alone may not make sense even for an external physician.
Therefore, the best and only reliable thing to do about any statement, finding or coding in your MRI report is to talk to your doctor who ordered this test. Your doctor will be able to explain the meaning of this statement in the most accurate way by evaluating the entire report, the images themselves and, most importantly, your complaints and examination findings as a whole. Trying to find the meaning of such specific codes on the internet or other sources may cause you unnecessary worry or misinformation.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.