Anticoagulants are medications that prevent abnormal blood clot formation by inhibiting specific steps in the coagulation cascade. They are essential in treating and preventing conditions such as atrial fibrillation, deep vein thrombosis, pulmonary embolism, and stroke.
Traditional anticoagulants like warfarin require frequent monitoring of INR values to maintain therapeutic efficacy and avoid bleeding risks. Newer direct oral anticoagulants (DOACs) provide more predictable effects without routine monitoring, improving patient convenience.
The choice of anticoagulant depends on underlying disease, renal function, comorbidities, and drug interactions. Individualized therapy ensures both effective thromboprophylaxis and minimal risk of hemorrhagic complications.
Patients on anticoagulant therapy should be closely monitored for signs of bleeding, drug interactions, and compliance. Education regarding medication adherence and regular follow-up visits play a critical role in ensuring safe and effective treatment outcomes.
| Medical Name | Anticoagulant Drugs (Blood Thinners) |
| Frequent Use Areas | – Treatment of deep vein thrombosis (DVT) and pulmonary embolism- Atrial fibrillation- Heart valve diseases- Stent applications |
| Causes | – Prevent or treat blood clots |
| Risk Factors | – Coagulation disorders- Long-term immobility- Heart rhythm disorders- Presence of stent or prosthetic valve |
| Complications | – Risk of bleeding (internal and external bleeding)- Bruises on the skin- Rarely impaired liver or kidney function |
| Diagnostic Methods | – Blood tests (INR, aPTT, anti-Xa level, kidney and liver functions)- Clinical evaluation |
| Treatment Methods | – Warfarin, heparin, low molecular weight heparin, new generation oral anticoagulants (NOAC/DOAC) |
| Prevention Methods | – Regular blood tests and follow-up- Not changing the dose without doctor’s recommendation- Protection from falls and traumas |
What is an anticoagulant and why is it incorrectly called a ‘blood thinner’?
It is quite common for people to call these medicines “blood thinners”, but this term does not actually describe what the medicine does. Think of it this way: these drugs do not physically thin your blood like water or increase its fluidity. If they were, your blood cells would not be able to do their job.
The truth is that these drugs interfere with the complex chain of chemical reactions that make blood clot. This wonderful clotting mechanism, which stops bleeding when we are cut, can sometimes be triggered unintentionally inside the blood vessels. Anticoagulant drugs prevent dangerous clot formation by “slowing down” this internal mechanism. It does not stop clotting completely, it only controls it.
At this point it is necessary to distinguish between two different groups of anticoagulants that are often confused. These drugs act on different links in the coagulation chain.
It is important to know whether the medicine used in your treatment is an anticoagulant or an antiaggregant. For example, the answer to the common question “Is Coraspin an anticoagulant?” is no. Coraspin (aspirin) is an antiaggregant and acts through platelets. The main differences between these two groups are as follows:
Anticoagulants (eg: Warfarin, Eliquis, Xarelto, Pradaxa)
- Targets proteins called clotting factors.
- It slows down the clotting chain (cascade) itself.
- It is often used in conditions such as atrial fibrillation or deep vein thrombosis.
Antiaggregants (e.g. Aspirin/Coraspin, Clopidogrel/Plavix)
- It targets blood platelets called platelets.
- It prevents platelets from sticking together and forming a plug.
- It is usually used for protection after a heart attack or stent.
How Does Our Body Form a Blood Clot?
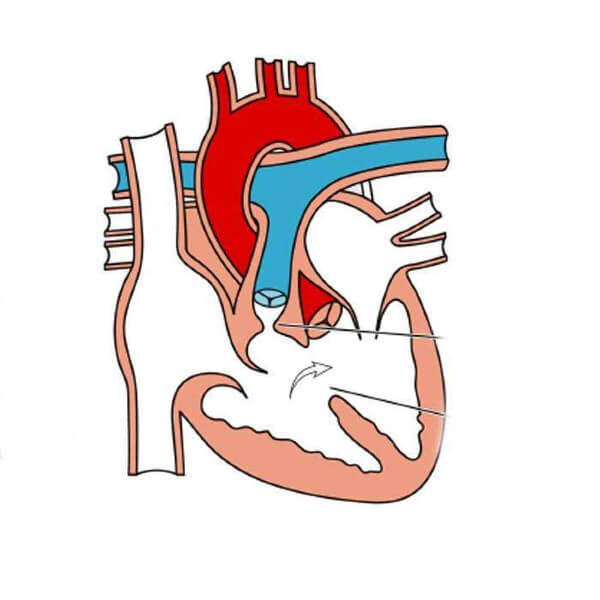
Our body’s ability to form clots is actually a survival mechanism. When a blood vessel is damaged, an emergency team steps in to prevent blood loss. We call this process “hemostasis” and liken it to a domino effect.
The first domino falls with damage to the vessel wall. Platelets (blood platelets), the tiny “first aid workers” circulating in the blood, immediately stick to the damaged area. They come together and form a temporary plug in that area. But this plug is still weak.
This is where the second and more powerful mechanism, the clotting cascade, comes into play. A series of proteins circulating in the blood in an inactive state, called “clotting factors”, are activated one after the other, knocking over the dominoes. The ultimate goal of this chain reaction is to produce a very powerful enzyme called “thrombin”. Thrombin takes the final step and converts the soluble substance “fibrinogen” in the blood into insoluble “fibrin” strands. These fibrin strands weave a web around the temporary platelet plug, reinforcing it like concrete. This stops the bleeding. The substances that enable this natural process are generally called coagulants.
How do the anticoagulant medicines I take work?
Anticoagulants break the chain by intervening at a specific point in this ingenious domino effect we have just described. Each class of anticoagulant targets a different domino. Some block the production of these factors in the liver, others block a key factor or enzyme circulating directly in the blood.
There is a very important point to underline here. These medications do not “dissolve” an existing, i.e. pre-existing, clot or remove it like a cleanser. This is a very common misconception. Instead of extinguishing the fire, the task of these drugs is to turn off the faucet that pours gasoline on the fire. In other words, they prevent the existing clot from growing further and, most importantly, they prevent new clots from forming. This gives the body’s own repair mechanisms the opportunity to remove the existing clot over time. Therefore, knowing that you are “preventing” a dangerous future event is the greatest motivation for adherence to treatment, rather than expecting to see immediate benefits when taking these medicines.
What Types of Anticoagulant Drugs Are There?
Today, there are different anticoagulant drugs with different mechanisms of action. The management of your treatment depends on which medication you are taking.
Vitamin K Antagonists (Warfarin / Coumadin)
This is one of the oldest and best known anticoagulants. It works by blocking vitamin K, which the liver uses to make clotting factors. It has a slow onset of action and is slowly eliminated from the body. The most important feature of warfarin treatment is that its effect can vary from person to person and from day to day. Therefore, close monitoring with regular blood tests (INR) is essential in order to adjust the dose of the drug correctly.
Here are some important features of warfarin treatment:
- Requirement for regular INR blood testing
- Interaction with foods containing vitamin K, such as green leafy vegetables
- Potential for interaction with many different drugs (antibiotics, painkillers)
- It takes days to start and days to end
- Low cost
Heparins (injections such as Clexane)
Heparins are usually used in hospital settings or for short-term home treatments. They work very quickly by increasing the strength of a protein called “antithrombin”, the body’s own natural anticoagulant, by thousands of times. They are usually administered as an injection under the skin to prevent the risk of clots after major surgery or as a “bridge” when starting warfarin therapy. They usually do not require routine blood monitoring as their effects are predictable.
Direct Oral Anticoagulants (DOACs)
These are a new generation of anticoagulants that directly target key factors in the coagulation chain (Thrombin or Factor Xa). These drugs have revolutionized anticoagulant therapy.
The advantages of DOAK (Eliquis, Xarelto, Pradaxa, Lixiana) treatment are
- Does not require routine blood monitoring
- Fast onset of action (within a few hours)
- Virtually no interaction with food
- Fewer drug interactions
- Faster elimination of the effect from the body
Who May Need Anticoagulant Therapy?
In which cases are anticoagulant medicines used? This treatment is needed for people with certain health conditions where the risk of blood clotting is higher than normal. What these conditions have in common is that blood flow slows down, the vessel wall is damaged or the blood itself becomes more prone to clotting.
The main conditions requiring anticoagulant therapy are as follows:
- Atrial Fibrillation (AFib)
- Deep Vein Thrombosis (DVT)
- Pulmonary Embolism (PE)
- Presence of a mechanical (artificial) heart valve
- After Major Orthopedic or Cardiac Surgery
- Inherited Coagulation Disorders (Thrombophilia)
- Some Types of Cancer
In particular, atrial fibrillation, a rhythm disorder in the heart, is one of the most common causes. When the atria of the heart beat irregularly, blood pools there and can easily clot. This clot can travel to the brain, which is one of the most important causes of stroke. Anticoagulant therapy can reduce this risk by up to p
Why Anticoagulant Therapy After Heart Valve Surgery Is So Critical
As a cardiovascular surgeon, one of the issues we focus on most is anticoagulant management after heart valve replacement. This treatment is as vital as the surgery itself and differs fundamentally depending on the type of valve that is fitted.
Mechanical (Artificial) Lids: These lids are made of durable and long-lasting materials such as carbon. However, the body perceives this surface as “foreign” and constantly tries to form clots on it. For this reason, it is absolutely mandatory for a patient with a mechanical valve to take warfarin (Coumadin) for life in order for the valve to work properly and to prevent the risk of stroke. This is a non-negotiable rule. DOACs, which are new generation drugs, are definitely not used in this patient group as they have failed in studies.
Bioprosthetic (Tissue) Valves: Since these valves are made from animal (usually bovine or porcine) tissue, they have a much lower risk of clot formation. The biggest advantage for patients is that they usually do not have to take warfarin for life. However, in the first 3-6 months after surgery, the risk of clots increases slightly until the tissue heals. The treatment to be applied in this early period may vary from patient to patient and according to the surgeon’s preference.
Possible treatment options for bioprosthetic valves in the early postoperative period are
- Aspirin (antiaggregant) use only
- 3 months of warfarin (anticoagulant) use
- Use of DOAC (new generation anticoagulant) whose efficacy has been investigated by new studies
How and Why Should My Anticoagulant Therapy Be Monitored?
Your treatment will be monitored according to the type of medication you are taking and this will determine your responsibilities during treatment.
If You Are Taking Warfarin INR Test
An integral part of warfarin treatment is regular blood tests. The INR (International Normalized Ratio) is a value that measures the rate at which your blood clots. In a healthy individual, this value is around 1. The goal of our treatment is to bring this value down, usually to between 2.0 and 3.0, depending on your disease. This range is called the “therapeutic window” – effective enough to prevent clots, but safe enough not to cause dangerous bleeding. To maintain this delicate balance, INR tests are performed frequently, especially at the beginning of treatment, and then usually once a month.
If You Are Taking DOAK Responsibility for Regular Medication Use
The great convenience of the new generation of medicines (DOACs) is that they do not require these routine blood tests. However, this does not mean that you should be complacent. On the contrary, it takes the responsibility away from the test and puts it entirely on you. It is vital to take your medication every day, at the prescribed time, without fail.
Here are the golden rules for DOAK users:
- Taking the medicine at the same time every day
- Never skip a dose
- Never take a double dose to compensate for a forgotten dose (without consulting a doctor)
- Obtaining a new box before the medicine runs out
Are there any risks with this treatment and which side effects should I watch out for?
As with any effective treatment, anticoagulants have potential risks. The most important and most common risk is the inherent bleeding tendency of the drug itself. Remember, this is not a “side effect” but an extension of the desired effect of the drug. Our goal is to find that sweet spot that minimizes the risk of bleeding while preventing clotting.
You should be careful if you notice any unusual bleeding in your body. If you experience any of the following symptoms, you should contact your doctor or go to the nearest emergency room immediately:
- Bruises that form or enlarge abnormally easily
- more than 10 minutes of unstoppable nosebleeds
- Excessive or prolonged bleeding gums after tooth brushing
- Stool is bright red or tarry black
- Pink, red or cola-colored urine
- Coughing up blood
- Vomit like coffee grounds or with blood
- Abnormally heavy or prolonged menstrual bleeding in women
- Severe and sudden onset of headache, dizziness or loss of balance
- A serious fall or blow to the head (even without external bleeding)
What should I pay attention to in my daily life while taking anticoagulants?
Safe treatment depends as much on your care in everyday life as on the medicine. It is a team game.
Nutrition (especially for warfarin users)
If you are taking warfarin, you do not need to eliminate vitamin K-rich foods from your diet. The important thing is to maintain a balance by consuming about the same amount of these nutrients each week.
The main foods rich in vitamin K are:
- Spinach
- Cabbage (white, black, Brussels)
- Chard
- Broccoli
- Parsley
- Lettuce
- Turnip
Other Medicines, Herbal Products and Supplements
Many over-the-counter products may interact with your treatment. Always consult your doctor or pharmacist before starting any new medication, vitamin or herbal supplement.
Things to pay particular attention to:
- Painkillers (especially the NSAID group: ibuprofen, naproxen, etc.)
- Some antibiotics and fungicides
- St. John’s Wort
- Ginkgo biloba
- Garlic, ginger and ginseng supplements (high doses)
Daily Life and Safety Precautions:
You can take simple but effective measures to reduce the risk of bleeding.
Some precautions that can be taken:
- Using a soft-bristled toothbrush
- Using dental floss gently
- Choosing an electric machine for shaving instead of a razor
- Wearing gloves when gardening or working with cutting tools
- Avoiding contact sports or activities where there is a risk of falls
- Limiting alcohol consumption
What to do if there is unexpected serious bleeding during treatment?
This is what patients worry about most, but you should know that the medical world is prepared for this situation. In case of an emergency or life-threatening bleeding, there are special “antidotes” that can quickly reverse the effect of the anticoagulant you are taking. This is one of the most important safeguards of treatment.
Each group of drugs has its own specific reversal agent:
Warfarin In emergencies, special blood products (PCC) containing vitamin K and clotting factors are given intravenously.
For heparin: A drug called protamine sulfate quickly neutralizes its effect.
For DOACs: For each new generation of drugs there are specific antidotes (such as Idarucizumab, Andexanet alfa). These agents directly bind or inactivate the drug, allowing the clotting system to return to normal within minutes.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.