A thoracic aortic aneurysm is a pathological dilation of the aorta within the chest region. It may remain asymptomatic for years but carries the risk of rupture, which is a life-threatening condition requiring urgent medical intervention.
Symptoms of thoracic aortic aneurysm may include chest pain, back pain, cough, or hoarseness due to pressure on nearby structures. In some cases, sudden severe pain may indicate dissection or impending rupture, necessitating immediate diagnosis.
Causes of thoracic aortic aneurysm include hypertension, atherosclerosis, connective tissue disorders such as Marfan syndrome, and trauma. Genetic predisposition also plays a role, especially in familial cases, warranting screening of relatives.
Treatment of thoracic aortic aneurysm depends on size and growth rate. Small aneurysms are monitored with imaging and risk management, while larger or symptomatic cases may require surgical repair or endovascular stent grafting to prevent rupture.
| Medical Name | Thoracic Aortic Aneurysm |
| Anatomical Location | – Vasodilation (ballooning) of the aorta in the chest (thorax) |
| Common Symptoms | – Usually asymptomatic- Chest pain- Back or lower back pain- Shortness of breath- Difficulty swallowing or hoarseness (in advanced cases) |
| Causes | – Atherosclerosis (arteriosclerosis) – High blood pressure – Connective tissue diseases (Marfan syndrome etc.) – Trauma – Congenital anomalies |
| Risk Factors | – Hypertension- High cholesterol- Smoking- Family history of aneurysm- Advanced age |
| Complications | – Aneurysm rupture (rupture)- Life-threatening- Bleeding- Disruption of blood flow to organs |
| Diagnostic Methods | – CT angiography- MR angiography- Echocardiography- X-ray (indirect findings) |
| Treatment Methods | – Regular follow-up (in small aneurysms)- Blood pressure control- Surgical repair (open or with endovascular graft) |
| Prevention Methods | – Regular blood pressure control – Smoking and alcohol cessation – Healthy diet and exercise – Regular medical follow-up |
What is a Thoracic Aortic Aneurysm?
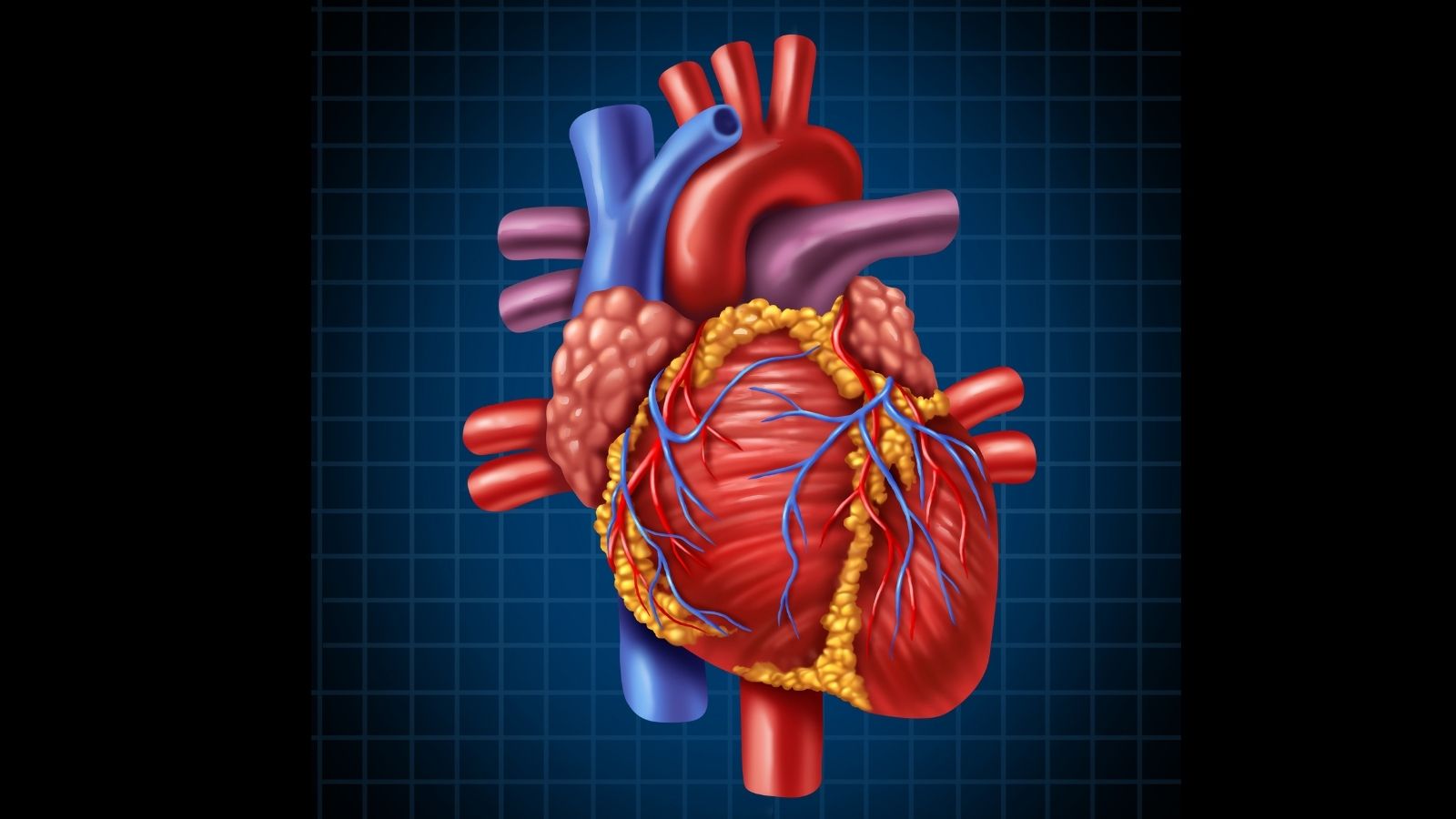
You can think of a thoracic aortic aneurysm as a ballooning of the aorta, the body’s main water pipe, in the chest. When the wall of this vessel, which is subjected to enormous pressure with every beat of the heart, weakens for various reasons, it loses its elasticity and begins to bulge outwards. It’s like an old tire herniating outward from a weak spot. This ballooned and weak area is called an aneurysm in medical language. For a dilatation to be considered an aneurysm, the vessel must be at least P larger than its normal diameter in that area.
The most worrying aspect of this condition is that it often grows silently for years without any symptoms. For this reason, it is often detected by chance when patients go to the doctor with a completely different complaint, for example a chest X-ray or CT scan. The appearance of symptoms can often be a sign that the aneurysm has reached a dangerous size or an emergency, such as a rupture (rupture) or a separation of the wall layers (dissection). This is actually the answer to the question of what a thoracic aortic aneurysm is without rupture; it means that the aneurysm has not ruptured but continues to exist, posing a potential risk. Therefore, regular screening of individuals with risk factors is not a luxury but a life-saving measure.
In which parts of the aorta do aneurysms occur and what are their types?
Aneurysms can occur in different parts of the aorta and have different names depending on their location and shape. This distinction is very important for planning the treatment to be applied.
The structure of the aorta can be likened to the handle of an old walking stick that comes out of the heart, curves upwards and then goes down. Aneurysms can develop at different points along this route of the aorta.
Here are the places where an aortic aneurysm can be seen depending on its location:
Ascending Aorta: It is the part that goes up just after the heart and is the most common site of aneurysms.
Aortic Arch (Aortic Arch): It is the apex where the veins that supply blood to the brain and arms branch off.
Descending Aorta: It is the part of the rib cage that goes downwards.
Thoracoabdominal Aorta: This is when the aneurysm extends to cover both the chest and abdomen.
According to their shape, there are two main types:
Fusiform Aneurysm: It is a symmetrical, spindle-shaped enlargement that surrounds the entire circumference of the vessel. It is the most common type.
Saccular Aneurysm: It is an asymmetrical, sac-like protrusion that forms on only one side of the vessel wall.
What are the Risk Factors Causing Thoracic Aortic Aneurysm?
The formation of an aneurysm is usually not due to a single cause, but rather to a combination of factors over time. Knowing these risk factors helps us understand who needs to be more careful.
We can list the main risk factors as follows.
High Blood Pressure (Hypertension): It is the most important factor that causes the aneurysm to grow by continuously exerting mechanical pressure on the weakened aortic wall.
Atherosclerosis (Hardening of the Arteries): It is the loss of elasticity and weakening of the vessel walls due to the accumulation of fat and cholesterol plaques.
Smoking: It is the most important modifiable risk that directly damages the vessel wall, increasing the risk of aneurysm development, growth and rupture.
Genetic Predisposition: A family history of aortic aneurysm or dissection significantly increases the risk.
Some Genetic Syndromes: Diseases that weaken connective tissue, such as Marfan Syndrome and Loeys-Dietz Syndrome, lead to aneurysm development, especially at a young age.
Bicuspid Aortic Valve: The congenital two-leaflet heart valve, which normally has three leaflets, disrupts blood flow in the aortic root and increases the risk of an aneurysm.
Advanced Age: The risk increases especially after the age of 65.
Gender: It is more common in men than in women.
What Are the Symptoms of Aortic Aneurysm and When Should It Be Taken Seriously?
The majority of aneurysms are completely asymptomatic, especially when they are small. However, as the aneurysm grows and begins to press on neighboring organs in the chest cavity, some signs may appear. Symptoms of a thoracic aortic aneurysm usually vary depending on the organ being compressed.
Possible symptoms of a growing aneurysm could be
- A deep, constant, throbbing pain in the chest or back, especially between the shoulder blades
- An unexplained and persistent dry cough
- Wheezing or shortness of breath
- Hoarseness or hoarseness of voice
- Sticking sensation during swallowing or difficulty swallowing
- Rarely swelling of the face, neck and arms
These symptoms are important signals to consult a doctor. However, there are some symptoms that indicate an emergency situation, i.e. an aneurysm rupture (rupture) or a separation of the wall layers (dissection), and require a call to the 112 emergency hotline without waiting a second.
Signs of a rupture or dissection requiring urgent intervention include
- A sudden, excruciating pain in the chest or back, described as “tearing” or “stabbing”
- Sudden dizziness, blackouts or fainting
- Severe and sudden onset of shortness of breath
- Cold sweats and sticky skin
- Nausea and vomiting
- Stroke-like symptoms such as difficulty speaking, numbness or paralysis on one side of the body
How Is Aortic Aneurysm Diagnosed and What Tests Are Used?
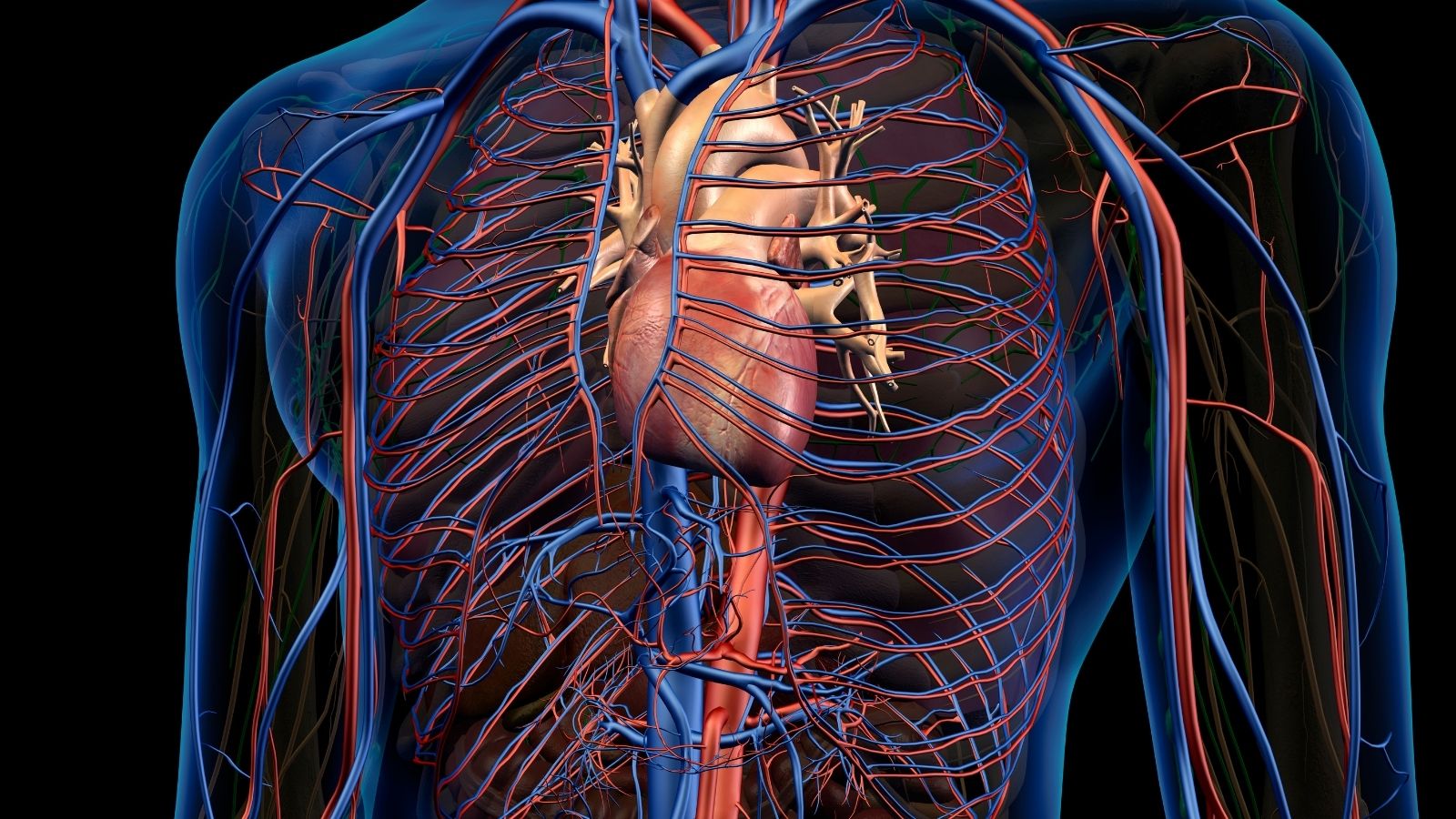
The answer to the question of how an aortic aneurysm is diagnosed lies in modern imaging technologies. When the presence of an aneurysm is suspected, often by chance, or for screening purposes in people at risk, various tests are used to clarify the situation. These tests are critical to confirm the presence of an aneurysm and to determine its location, size and shape.
The main imaging methods used in the diagnostic process are as follows:
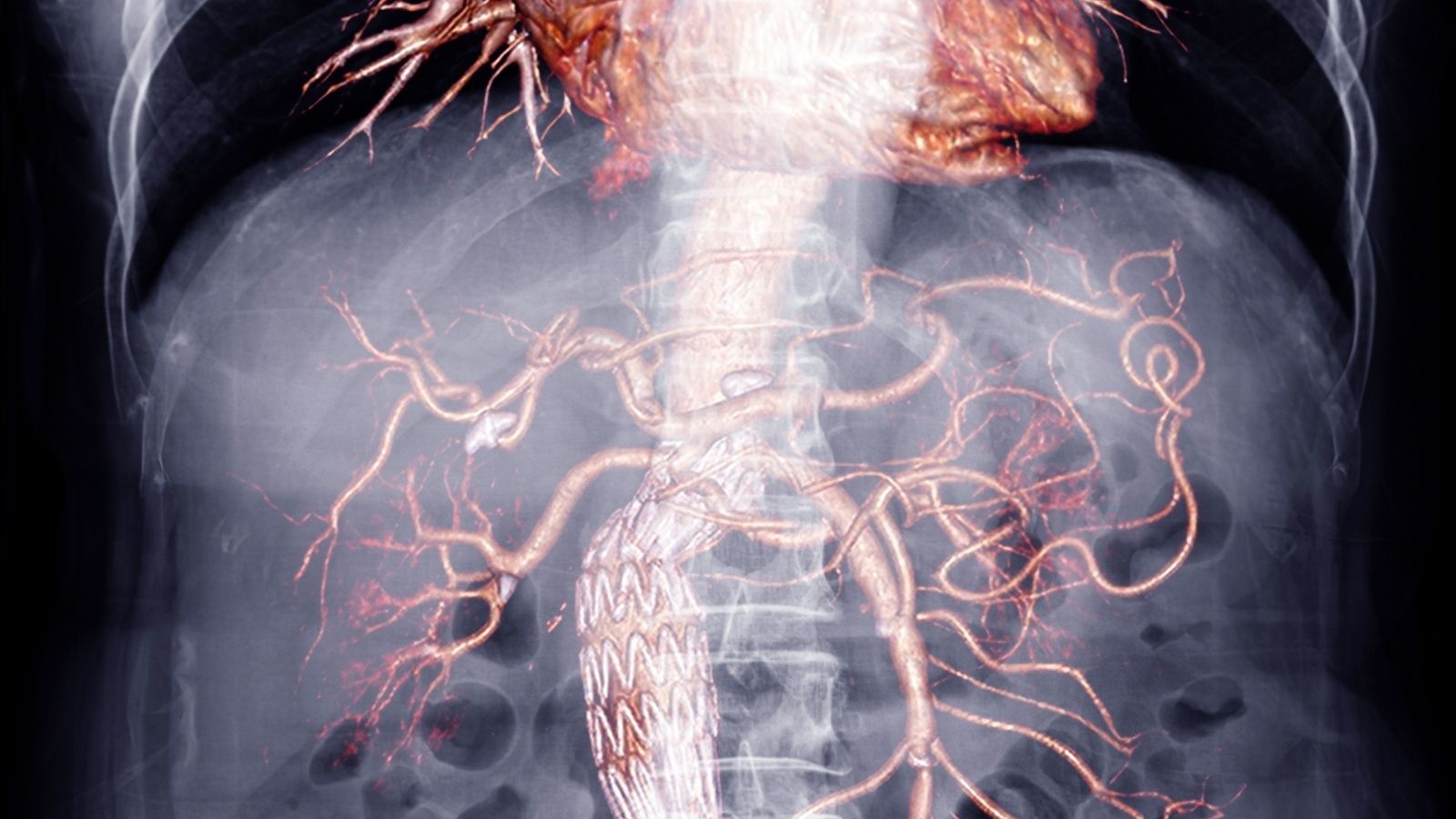
Computed Tomography Angiography (CTA/CTA): Also known as CT of the thoracic aorta, this is considered the “gold standard” for diagnosis and follow-up. It produces a detailed three-dimensional map of the aorta using contrast material. This allows the diameter of the aneurysm to be measured in millimeters and details such as clots in the wall or calcification, which is the answer to the question of what is thoracic aortic wall calcification.
Magnetic Resonance Angiography (MRA): Since it does not involve radiation, it is a method that is preferred especially in young patients or in cases where frequent follow-up is required and provides images with similar detail to BTA.
Echocardiography (Echo): This is an ultrasound of the heart. It is particularly valuable for evaluating the first part of the aorta where it exits the heart, i.e. the aortic root and the aortic valve. Echocardiography is frequently used to screen for aortic aneurysms. Sometimes an esophageal version (TEE) may be needed for a clearer image.
Chest X-ray It is usually the first suspicious test but is not diagnostic on its own.
What is the Treatment Approach when a Small Aneurysm is Detected?
Not every aneurysm diagnosis means that you should immediately go to the operating table. If the aneurysm is small (usually less than 5 cm), growing slowly and asymptomatic, a strategy called “watchful waiting” or “active surveillance” is followed. The basic logic of this approach is simple: The risk of an aneurysm rupturing is currently lower than the risks associated with major surgery.
But this does not mean ignoring the situation. Rather, it is an active management process involving two key steps.
Regular Imaging: Tests such as CTA or MRA are usually repeated every 6 to 12 months to closely monitor the rate at which the aneurysm is growing.
Aggressive Risk Factor Control: This is the most important part of treatment. The aim is to slow the growth of the aneurysm by reducing stress on the aortic wall. In this context, medications that control blood pressure and cholesterol are prescribed. In addition, lifestyle changes are as important as medication. It is highly recommended to quit smoking, eat a healthy diet and avoid activities that cause a sudden increase in pressure, such as heavy lifting.
When Is Surgery Necessary for Thoracic Aortic Aneurysm Treatment?
The timing of surgery for the treatment of thoracic aortic aneurysm is one of the most critical decisions of treatment. The aim is to intervene at the safest time for the patient before the aneurysm causes a life-threatening rupture or dissection. This decision is based on a personal approach where many factors are considered together.
The main factors that trigger the decision for surgery are:
Diameter of the Aneurysm: The most important objective criterion. As a general rule, surgical repair is recommended when thoracic aortic aneurysms reach a diameter of about 5.5 to 6.0 centimeters.
Growth Rate: Even if its size has not yet reached the surgical limit, if the aneurysm is growing rapidly (e.g. more than 1 cm per year), this is considered a sign that the wall is unstable and may require earlier intervention.
Presence of Symptoms: If the aneurysm starts to cause pressure symptoms such as pain or hoarseness, regardless of its size, this usually indicates an increased risk of rupture and makes surgery necessary.
Patient’s Special Condition: People with genetic connective tissue diseases such as Marfan syndrome have a more fragile aortic wall. Therefore, the threshold for surgery is lower in these patients and surgery may be recommended when aneurysms are smaller in diameter (e.g. 4.5-5.0 cm).
What Is Open Aneurysm Surgery?
Open aneurysm repair is the most established and proven surgical technique in this field. In this method, the chest cavity is accessed by cutting vertically through the breastbone (sternotomy) or by making an incision between the ribs (thoracotomy). During the operation, the blood circulation is connected to a heart-lung machine to provide blood supply to the other organs of the body. The heart is temporarily stopped and the surgeon carefully removes the diseased, ballooned part of the aorta. In its place, he sews a tubular artificial vessel (graft) made of a highly durable synthetic material such as Dacron.
What you need to know about this method:
- It is a major and extensive surgery.
- Proven long-term results and durability are very high.
- The recovery period is longer and the hospital stay is longer.
- It is usually an ideal option for younger patients in good general health.
- It may be the only treatment option for complex aneurysms such as aortic root and ascending aorta.
What is the TEVAR (Endovascular Repair) Method and How is it Applied?
TEVAR is a minimally invasive technique (with fewer incisions) developed over the last two decades that offers an alternative to open surgery. The main aim of this method is to repair the aneurysm from the inside, avoiding major breast surgery.
In this procedure, instead of opening the chest, the surgeon makes a small incision in the artery in the patient’s groin area. Through this incision, a thin system called a catheter, a compressed fabric-covered metal stent (stent-graft) is advanced into the vessel. Under the guidance of angiography, this stent-graft is delivered to the site of the aneurysm, opened in a controlled manner and placed in the inner wall of the aorta. This procedure prevents blood from entering the aneurysm sac and creates a new pathway. This relieves the pressure inside the sac and prevents the risk of rupture.
What you need to know about the TEVAR method:
- It is a minimally invasive procedure.
- The incisions are in the groin and are much smaller.
- The hospital stay and return to normal life is much faster.
- It is generally preferred for older patients or patients with additional health problems who are at high risk of open surgery.
- It requires regular lifelong follow-up due to risks such as “endoleak” (leakage) in the long term.
How Does Life Span After Aortic Aneurysm Surgery Affect?
One of the most frequently asked questions by patients is the duration and quality of life after aortic aneurysm surgery. The answer to this question depends on when and how the surgery is performed. Long-term results after a successful surgery performed in a planned manner without rupture of the aneurysm are extremely satisfactory. Scientific studies show that the life expectancy of patients who survive the first critical period after surgery is almost the same as that of healthy individuals of their own age. This means that successful treatment eliminates the life threat posed by the aneurysm and gives the patient the chance to live a normal life. However, in emergency conditions, i.e. after a rupture or dissection, the risks are higher and this can have a negative impact on long-term survival. This difference once again demonstrates the vital importance of early diagnosis and planned treatment.
How Should Postoperative Recovery and Long-Term Follow-Up Be?
Having aneurysm surgery is not the end of treatment but the first step towards a healthy future. The postoperative period is a lifelong journey that involves both physical recovery and managing future risks.
Things to consider during recovery and follow-up.
Recovery in Hospital and at Home: Recovery time varies depending on the type of surgery. While full recovery after open surgery may take 2-3 months, this period is usually 1-4 weeks after TEVAR. Fatigue, loss of appetite and pain are normal during this period. Heavy lifting, strenuous exercise and driving should be avoided for the period prescribed by your doctor.
Lifelong Follow-up: Aneurysm repair does not completely cure the underlying weakness in the vessel wall. Therefore, other unrepaired parts of the aorta may have new enlargements in the future. To check this, it is essential that all patients are followed up regularly with imaging tests (CTA or MRA) for life.
Lifestyle Management: Maintaining aortic health in the long term depends on controlling the risk factors that lead to an aneurysm.
Here’s what you need to do to protect your long-term health:
- Keeping your blood pressure at targeted levels
- Adopting a heart-friendly diet low in salt and saturated fat
- Doing regular exercises (such as walking) approved by your doctor
- Absolutely and permanently abstain from smoking and all tobacco products
- To inform all health professionals about the implanted artificial vessel (graft).

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.