A Left Ventricular Assist Device (LVAD) is a mechanical pump implanted to support patients with advanced heart failure. It assists the left ventricle in pumping blood to the body, providing life-saving support while awaiting heart transplantation or as a long-term therapy.
Indications for LVAD include patients with end-stage heart failure who no longer respond to medical treatment. The device can be used as a bridge to transplantation or as destination therapy for those ineligible for transplant. It significantly improves survival rates and quality of life.
The implantation procedure requires open-heart surgery and specialized intensive care. Postoperative management includes anticoagulation therapy to prevent blood clots, strict infection control, and careful monitoring of device function. Education of both patient and caregivers is critical.
Living with an LVAD involves adjustments to daily life, including external power supply management and routine follow-ups. With proper care and compliance, patients can return to many normal activities. Technological advances continue to improve LVAD safety, durability, and comfort.
| Medical Name | Left Ventricular Assist Device (LVAD) |
| Type | Mechanical circulatory support system |
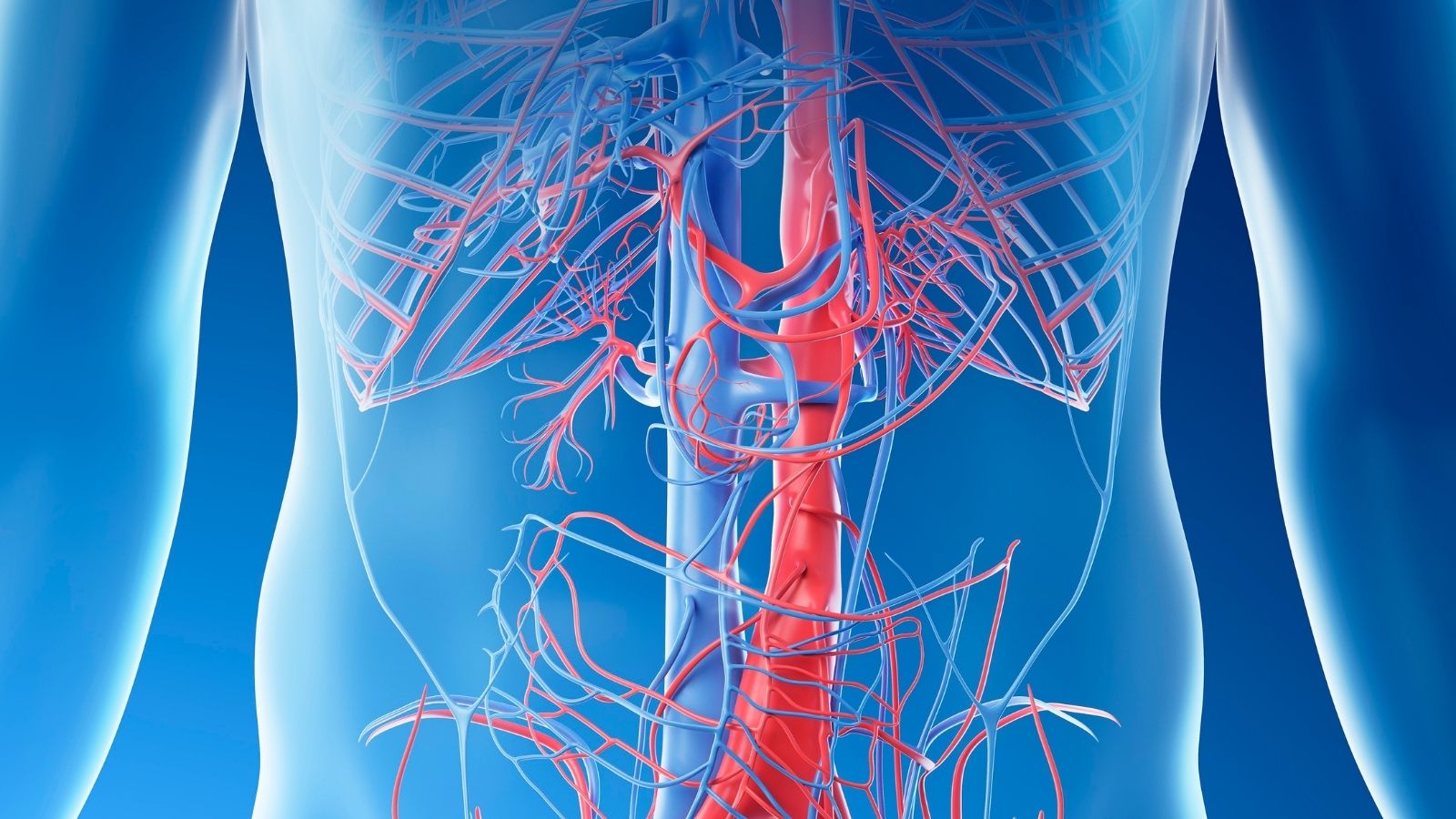
| Affected System | Cardiovascular system |
| Indications | Severe heart failure (NYHA class III-IV); for bridge to heart transplantation or long-term support |
| But | Ensure organ perfusion by supporting the pumping function of the left ventricle |
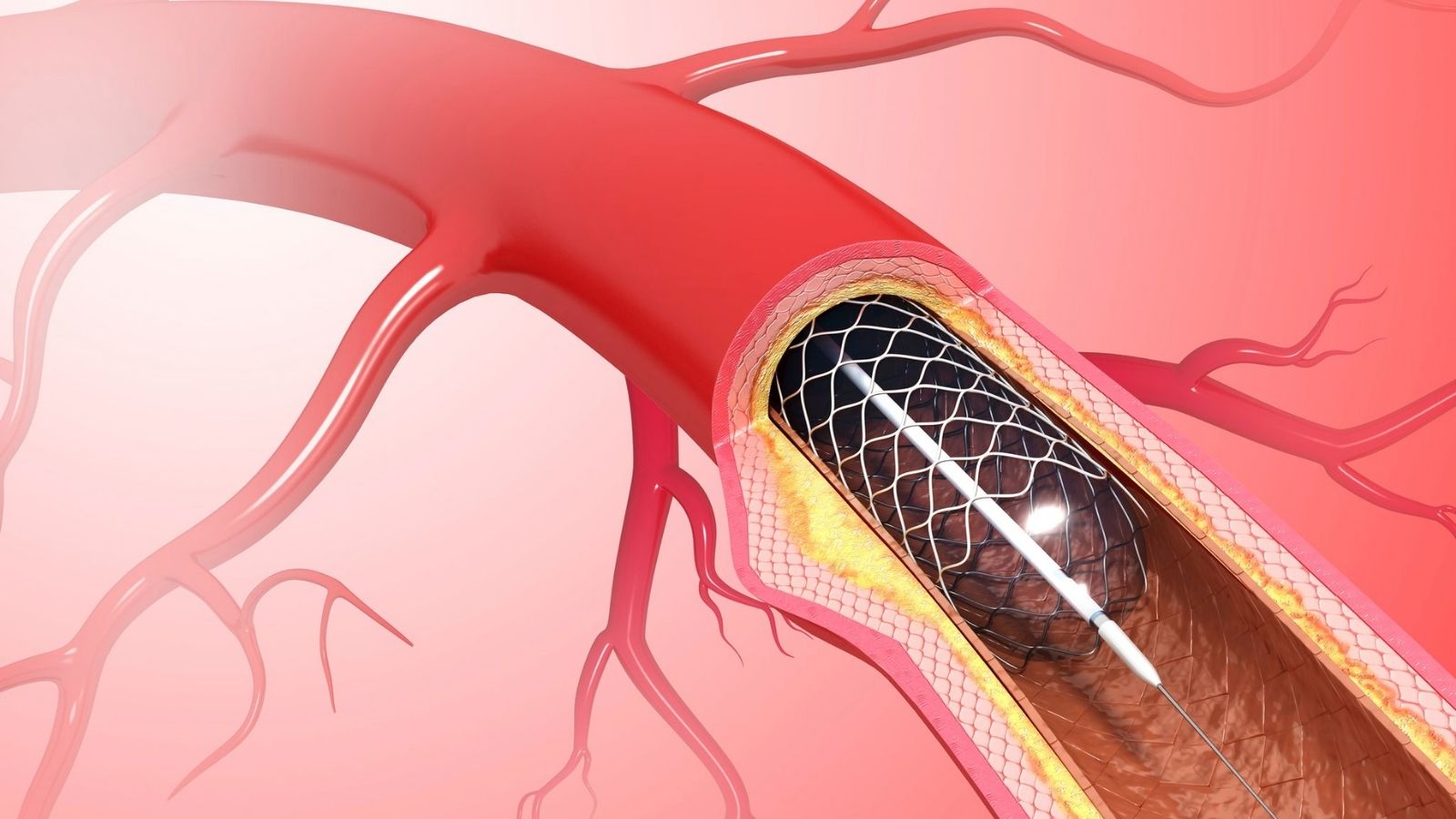
| Application Method | The device is surgically implanted in the heart: contains a pump system that takes blood from the left ventricle and delivers it to the aorta |
| Alternative Methods | Heart transplant, medical therapy (limited effect); other assistive devices (BiVAD, TAH) |
| Complications | Infection, bleeding, thrombosis, stroke, device failure, hemolysis |
| Observation | Lifelong anticoagulation, infection monitoring, device management training, frequent clinical and laboratory controls |
What is a Left Ventricular Assist Device (LVAD) and how does it help the heart to function?
You can think of the Left Ventricular Assist Device as a miniature “helper motor” that supports your heart when it is tired and no longer able to pump enough blood throughout the body. This device is not a heart transplant; rather, it works alongside your own heart, taking over its most important task: pumping clean blood throughout the body. It takes blood from the left ventricle (left ventricle), the hardest working and most tired chamber of your heart, and directs it to the aorta, the main artery of your body.
This means that all your vital organs, from your brain to your kidneys, get the oxygen and nutrient-filled blood they need. The LVAD relieves the heavy burden on your heart, allowing it to rest while you breathe again, regain your energy and participate more actively in life.
This intelligent system consists of several parts that work in perfect harmony with each other. The main pump of the device is surgically implanted inside your chest cage, close to your heart. This pump is connected to a power source outside the body via a thin cable (driveline) that is removed through your abdominal wall. This cable allows the device to receive energy and operate. A small control unit, which you will carry outside your body, is like the brain of the device; it monitors the operation of the pump and provides you with the necessary information. It draws its power from rechargeable batteries that you can carry with you or directly from a power outlet at home.
One of the most interesting features of modern LVADs is that they pump blood like a continuous river flow, rather than in a “beating” rhythm like the natural rhythm of the heart. A practical consequence of this is that most patients do not feel a pulse as we know it in the wrist or neck. This is certainly nothing to worry about; on the contrary, it is a sign that the device is doing its job successfully. Blood pressure measurements are therefore made with a specialized Doppler device.
In which cases is a Left Ventricular Assist Device (LVAD) treatment recommended and what are the different purposes of this treatment?
LVAD therapy is considered for patients whose heart failure is now end-stage, when the best available drug therapies and other methods have failed to control symptoms. The introduction of this treatment for a patient usually coincides with a period of severely reduced quality of life, with persistent shortness of breath, fatigue and frequent hospitalizations.
Because each patient’s condition and future prospects are different, the goal of LVAD treatment is also individualized. We can think of these goals as different “roadmaps” drawn for our patient. The main ones are these roadmaps:
- Bridge-to-Transplant Therapy: This is the most well-known use of the LVAD. It establishes a “bridge to life” for patients who need a heart transplant but have to wait until a suitable heart is found. The LVAD keeps the patient alive and their organs healthy during the waiting period, so that they are in the best condition for transplantation.
- Permanent Support Therapy (Destination Therapy): Some patients may not be suitable candidates for heart transplantation due to advanced age or additional health problems (such as diabetes, kidney failure). In this case, the LVAD becomes not a bridge but the treatment itself – a permanent solution. The goal is to ensure that the patient lives the rest of his or her life with the device in the highest possible quality and comfort. Thanks to advances in technology, LVADs can now operate for years without problems, offering these patients an invaluable quality and duration of life.
- Bridge-to-Recovery: In rare cases, the condition causing heart failure may be temporary (e.g. heart muscle weakness during pregnancy or due to a severe infection). In such cases, the LVAD takes over the burden of the heart for a while, giving it the opportunity to take a “healing vacation”. Once the heart is sufficiently strengthened, the device can be surgically removed and the patient can resume life with their own heart. This is one of the most gratifying outcomes of treatment.
- Bridge-to-Candidacy: Sometimes patients are initially deemed unsuitable for transplantation because of the damage heart failure causes to other organs (for example, very high lung pressure). An LVAD can help these organs recover by improving blood circulation. Once organ function returns to normal, the patient may now be a suitable candidate for a heart transplant.
How is it decided whether a patient is a candidate for a Left Ventricular Assist Device (LVAD) and what do INTERMACS profiles mean in this process?
Deciding whether a patient is a candidate for LVAD is a highly detailed evaluation process that is not carried out by a single physician, but by a large team of cardiologists, cardiac surgeons, LVAD coordinators, psychologists and dietitians. This process takes into account not only the condition of the heart, but also the patient’s general health, psychological state and how prepared he or she is for this major change.
In general, a patient is expected to meet some basic medical criteria to be a candidate for LVAD. Some of these criteria are:
- Symptoms of advanced heart failure (NYHA Class III-IV) that persist despite all powerful medications and make daily life impossible.
- The heart’s pumping power (Ejection Fraction – EF) is at a critical level, usually below %.
- The function of other vital organs such as the kidneys or liver begins to deteriorate due to heart failure.
- Becoming dependent on intravenous heart-boosting drugs (inotropes) to stay alive.
- Frequent hospitalizations for heart failure in the last year.
In addition to these criteria, the right timing is as vital as the right patient selection. This is where a classification system called INTERMACS comes into play. INTERMACS is a “timing scale” that rates the urgency of a patient’s clinical condition on a scale of 1 to 7.
- INTERMACS 1: The patient is in critical condition, connected to life support machines in intensive care. Surgery at this stage is very risky.
- INTERMACS 2-3: The patient is in hospital and depends on continuous intravenous drug support. His/her condition is fragile and prone to deterioration.
- INTERMACS 4: The patient is at home but experiences severe shortness of breath with even the slightest exertion (such as getting dressed).
The “golden window” of best outcomes from surgery is usually when patients are in INTERMACS profiles 3 and 4. This means that the patient has the best chance of success if they are operated on before they are in critical shock, but when their quality of life at home has become unsustainable. Achieving this delicate balance is one of the most important keys to treatment success.
Finally, it is important to recognize that this treatment is not suitable for every patient. Additional serious illnesses, such as untreatable cancer, or the lack of adequate social and psychological support for the patient and their family to cope with this difficult process, can be a barrier to treatment.
What awaits me in the hospital before, during and after a Left Ventricular Assist Device (LVAD) surgery?
LVAD surgery is not a one-day event, but a carefully planned journey that takes weeks. This journey is a team effort in which the patient and family are informed and actively involved at every step.
Preoperative Preparation Period
You will be admitted to the hospital a few days before your surgery. This period includes a series of tests and assessments to prepare you for surgery in the safest way possible. The team will take a close interest in you and your family and explain the whole process in detail. Here are some steps in this preparation period:
Comprehensive blood tests
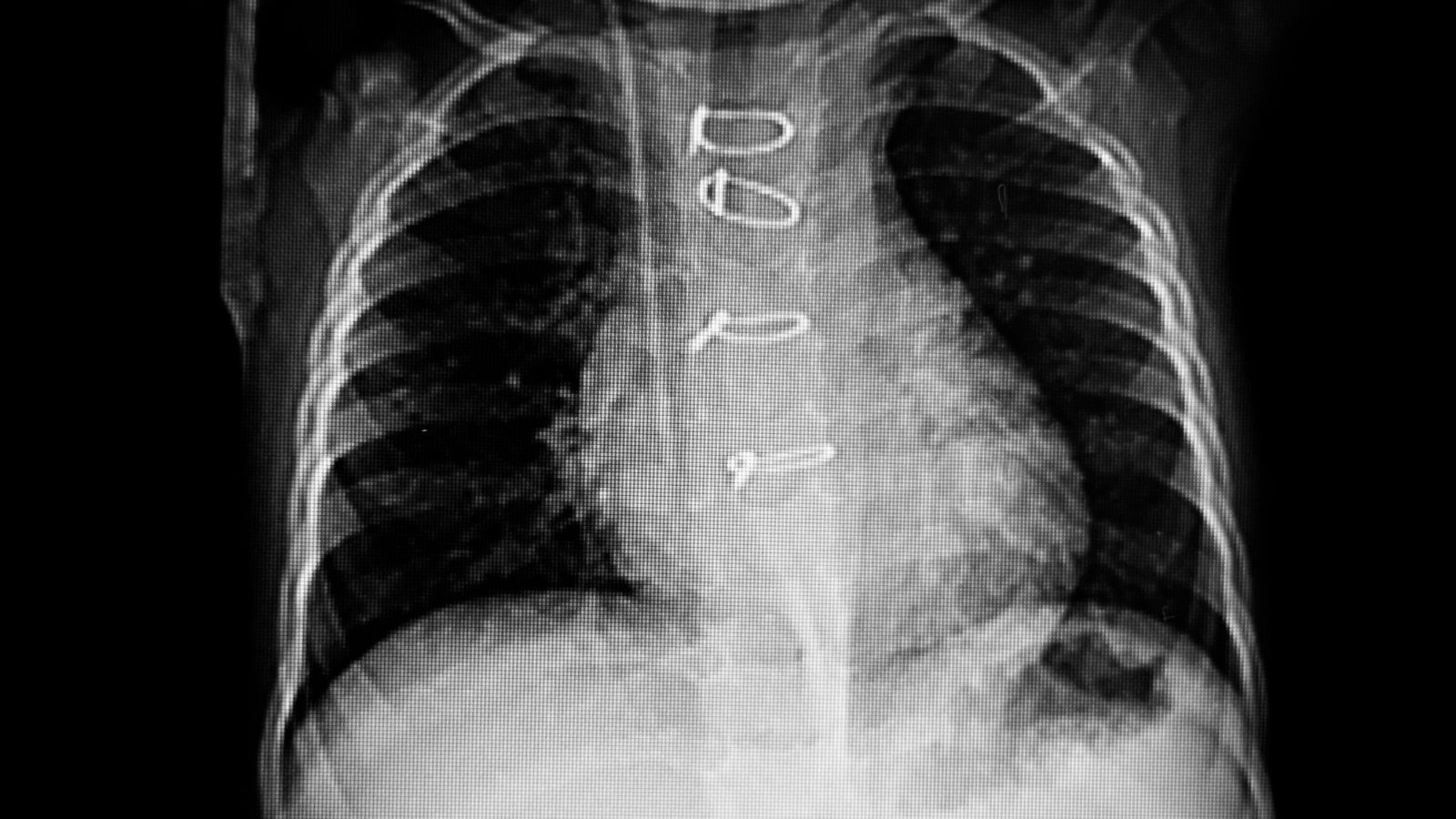
- Echocardiography (ECHO), which shows the structure and function of your heart in detail
- Lung X-ray and computed tomography (CT) if necessary
- Cardiac catheterization to measure right heart function
At the same time, you and your relative (caregiver) will receive initial training on how to use the device, how to change batteries and how to make dressings.
Surgery Day
LVAD implantation is a major open heart surgery that takes about 4 to 6 hours. The surgery is performed under general anesthesia, meaning you are fully asleep. The surgeon reaches your heart by opening your breastbone. During the operation, your heart is temporarily stopped and your blood circulation is maintained by a heart-lung machine. The surgeon carefully inserts the pump into the left ventricle of your heart and into your aorta. He or she removes the power cable (driveline) through your abdominal wall. Once all connections have been completed and the device has been checked to be working, you leave the heart-lung machine and the LVAD starts pumping blood.
Postoperative Recovery Process
You will spend the first few days after surgery in the intensive care unit. Here you may be on a ventilator and will be monitored very closely. Once your condition stabilizes, you will be transferred to the cardiology ward, where the recovery process will continue. Your hospital stay varies from 2 to 4 weeks on average, depending on the speed of your recovery. During this period, under the supervision of physiotherapists, you begin to stand up slowly, walk and regain your strength.
The most important part of this process is the training. You and your caregiver learn hands-on all the details of living with the LVAD. Once you are fully competent in recognizing alarms, managing batteries, dressing the driveline in a sterile manner and are medically fit, you will be discharged to start your new life.
What positive effects does Left Ventricular Assist Device (LVAD) treatment have on survival, quality of life and physical capacity?
The benefits of LVAD treatment go far beyond statistics and numbers – they are like a new lease on life. The most tangible and valuable effects of this treatment are that it both prolongs life and makes it “worth living”.
LVAD is a turning point for patients who have become bed- or chair-dependent in the pre-operative period, struggling to meet even their simplest needs. The positive effects of treatment can be summarized under several headings.
Meaningful Increase in Life Expectancy:
This is the most fundamental success of the LVAD. Major scientific studies have shown that the survival rates of patients with LVADs are many times higher than those with drug therapy alone. With modern devices, success rates have improved so much that one-year survival has reached -85. For patients whose life expectancy used to be limited to months, this means gaining years of valuable time.
Revolutionary Improvement in Quality of Life:
Perhaps the most magical touch of LVAD is felt here. But the goal is not just to survive, but to come back to life. The vast majority of patients, almost 8 out of 10, feel as if they have been reborn after surgery. Here are some of the features that this improvement has brought:
- Elimination of shortness of breath experienced at night and in the daytime.
- The feeling of constant fatigue and exhaustion is replaced by energy.
- Being able to return to ordinary but long-awaited activities such as walking and shopping.
- Spending quality, enjoyable time with family and friends.
- To move from a life dependent on the hospital to the comfort and independence of one’s own home.
- Visible Increase in Physical Capacity:
This improvement is not just a “feeling”, it is tangibly measurable. In standardized measurements, such as the 6-minute walk test, the distance patients walk can double after surgery. Whereas they used to have difficulty walking from room to room, they can now comfortably walk hundreds of meters. This means that the patient regains independence and self-confidence.
What are the main risks and complications of Left Ventricular Assist Device (LVAD) surgery and life afterwards and how are they managed?
LVAD therapy is a complex, life-saving technology that brings with it serious risks and responsibilities to manage. Discussing these risks openly is the most important step in making an informed decision about treatment and managing the process successfully. It is important to remember that your LVAD team is always there to anticipate and manage these potential issues.
The main potential complications that may be encountered in this process are:
- Bleeding: Bleeding, especially in the gastrointestinal tract, may occur due to the blood thinners used to prevent clotting. This is the most common complication in LVAD patients and is usually controlled by adjusting drug doses or endoscopic interventions.
- Infection: The point where the power cable (driveline) exits the skin is a gateway for infection. Meticulous and sterile dressing of this area every day is the most basic rule to prevent infection. If infection develops, long-term antibiotic treatment may be required.
- Clot Formation Inside the Pump (Thrombosis): In rare cases, a blood clot may form inside the pump. This can affect the operation of the device or, more dangerously, the clot can travel to the brain and cause a stroke. Inadequate use of blood thinners or infections can increase this risk. If diagnosed early, it can be managed with drug treatments, but sometimes the pump may need to be replaced.
- Stroke (Paralysis): LVAD patients are at risk of both clot-related (ischemic) and brain bleeding (hemorrhagic) stroke. Strict control of blood pressure and careful adjustment of blood thinners play a critical role in reducing this risk.
- Right Heart Failure: While the LVAD helps the left heart, the right side of the heart may struggle to manage the increased blood flow. This condition is usually managed with medication, but sometimes additional interventions are required to temporarily support the right heart.
These risks may seem frightening, but modern devices and experienced teams have reduced the incidence of these complications and made their management much more successful. The success of the treatment depends on strong cooperation between the patient, their family and the LVAD team, and strict adherence to the rules.
How does today’s modern Left Ventricular Assist Device (LVAD) technology differ from older generation devices and what are the advantages of these advances for patients?
The progress of LVAD technology over the last three decades is a success story that has gone from science fiction movies to reality. This evolution from early devices to today’s modern systems has focused on improving patient comfort and safety at every step.
We can analyze this technological development in three main generations:
- Generation Devices: These were large and mechanically cumbersome pumps that tried to mimic the natural beating of the heart. Because they had so many moving parts, they often failed, worked noisily and had a very short lifespan. These devices, which were a “first attempt”, are no longer in use today.
- Generation Devices: This generation was much smaller, quieter and more durable, pushing the blood in a continuous flow like a propeller. This made the LVAD a “permanent treatment” option for the first time. However, the major disadvantage of these devices was that they were a bit harsh on blood cells, increasing the risk of clots forming inside the pump (thrombosis).
- Generation Devices (Today’s Gold Standard): Devices such as the HeartMate 3, which we currently use and are considered the “gold standard”, represent the pinnacle of technology. These devices have solved almost all the problems of previous generations. The greatest innovation is the “Full Magnetic Levitation” technology. In this system, the impeller (rotor), the only moving part of the pump, rotates suspended in the air on a completely magnetic cushion, without sliding anywhere.
The revolutionary benefits to patients of this frictionless design include the following:
- The risk of clots forming inside the pump (thrombosis) is reduced to almost zero.
- The mechanical life of the device is much longer.
- Because it is much more “gentle” on blood cells, blood-related complications are significantly reduced.
In addition, these modern devices create an “artificial pulse” by periodically changing their speed instantaneously to prevent blood from stagnating in the pump. This helps the system to function more safely and physiologically. Thanks to these technological marvels, LVAD treatment is safer and more effective than ever before.
What changes will happen to my daily life, diet, activities and psychological state after my Left Ventricular Assist Device (LVAD) implantation?
Starting life with an LVAD is both an exciting and responsible process that requires adapting to a new “normal”. This new life involves caring for this device as it becomes part of your body and adopting some lifestyle changes. Remember that you are not alone on this journey; it is a journey of partnership between you and the caregiver closest to you.
Daily Routines and Device Maintenance:
In your new life you will have some daily routines. Over time, these will become a habit and a natural part of your life.
- Changing the driveline dressing every day in a sterile manner.
- Charge the batteries of the device regularly.
- Always carry spare batteries and a spare control unit with you when going outside.
- Recognize the alarms of the device and know what they mean.
Personal Hygiene and Prohibitions:
The most important rule is that the external parts of the device should never get wet. There are therefore some activities that you should cut out of your life.
- Swim (pool, sea)
- Washing by filling the bath tub
- Entering a jacuzzi or sauna
These are strictly forbidden. However, this does not mean that you cannot be cleaned. After your surgical wounds have healed, you can safely take a shower using special waterproof shower kits that protect the external parts of the device.
Nutrition Scheme:
A heart-healthy, salt-restricted diet is usually recommended. This helps to prevent fluid retention in the body and keep blood pressure under control. If you are taking Coumadin (Warfarin), a blood thinner, the amount of vitamin K in your diet becomes important. This vitamin can change the effect of the medicine. The important thing is not to cut out vitamin K-rich foods (leafy greens such as spinach, cabbage, broccoli) completely, but to eat them consistently, in about the same amount every day.
Physical Activity and Sport:
Once your recovery is complete, you can return to many physical activities with your doctor’s approval.
- Walking
- Gardening
- Light housework
- Sports that do not require contact, such as golf
However, you should avoid contact sports such as soccer, basketball and heavy lifting where there is a risk of falling and hitting the device.
Psychological Adjustment and Support:
The idea of living with a device attached to your body can be disconcerting at first. It is normal to experience emotional difficulties such as worries about your body image, anxiety or depression. Likewise, your caregiver may experience stress and fatigue because he or she is taking on a great deal of responsibility. Do not hesitate to seek professional psychological support during this time and join LVAD support groups to talk to people who are going through the same experiences as you. Supporting each other is the most important part of this new life.
Frequently Asked Questions
What is LVAD?
An LVAD (Left Ventricular Assist Device) is a mechanical pump that supports the pumping function of the left ventricle of the heart.
Who is it suitable for?
It is suitable for patients with severe heart failure who are awaiting a heart transplant or who are not transplant candidates.
Does LVAD replace the heart?
No, it does not completely replace the heart; it only supports the pumping function of the left ventricle.
Is LVAD placement an operation?
Yes, open heart surgery involves opening the chest cage and inserting the device.
Is LVAD temporary or permanent?
It depends on the situation. It can be used as a bridge to transplant or as destination therapy.
Can LVAD patients return to their normal lives?
Yes, it is possible to live with the device. Daily life activities can be maintained with careful planning.
Can the device be seen from the outside?
Yes, there is an externally mounted control unit and battery system.
Can I take a shower with an LVAD?
Direct water contact is prohibited; dry bathing or cleaning with special protective systems is recommended.
How long does the battery last?
Portable batteries usually last 8-12 hours and spare batteries should be kept on hand at all times.
Is there a risk of infection?
There is a risk of infection where the cables of the device come out; hygiene is very important.
Does LVAD device prevent heart transplant?
No, on the contrary, it ensures survival until transplantation and acts as a bridge that prepares the body.
How often are patients with LVADs checked?
Frequent check-ups are done at the beginning; once the condition stabilizes, follow-up by a doctor continues at intervals.
Which specialists deal with LVAD?
Cardiovascular surgeons, cardiologists and LVAD nurses form a multidisciplinary team.
When is the LVAD removed?
The device can be removed in the event of a heart transplant or, in rare cases, if heart function improves.
Can you live with LVAD for a long time?
Yes, with proper care and follow-up, the device can work for years and significantly extend its lifespan.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.