EVAR and TEVAR are minimally invasive procedures used to treat abdominal and thoracic aortic aneurysms. They involve inserting stent grafts to reinforce weakened aortic walls and prevent rupture.
Symptoms of aortic aneurysms include abdominal or back pain, pulsating sensations, and in severe cases, sudden rupture with life-threatening bleeding. Early detection is crucial for timely treatment and survival.
The EVAR procedure addresses abdominal aortic aneurysms, while TEVAR is applied to thoracic aneurysms. Both involve endovascular stent placement through small groin incisions, reducing recovery time compared to open surgery.
Risks include endoleaks, graft migration, or vessel injury. Lifelong follow-up with imaging is required to monitor stent stability and prevent late complications, ensuring long-term treatment success.
| Category | EVAR (Endovascular Aneurysm Repair) | TEVAR (Thoracic Endovascular Aneurysm Repair) |
| Application Area | Abdominal aortic aneurysms | Thoracic aortic aneurysms |
| Type of Surgery | Minimally invasive endovascular intervention | Minimally invasive endovascular intervention |
| Input Path Used | Usually groin (femoral artery) | Usually groin (femoral artery) |
| Imaging Guide | Fluoroscopy and angiography | Fluoroscopy and angiography |
| Type of Anesthesia | General or local anesthesia | Usually general anesthesia |
| The Progression of Renewal | Shorter compared to open surgery | Shorter compared to open surgery |
| Complication Risk | Endoleak, graft displacement, decreased renal function | Endoleak, paraplegia, graft migration |
| Need for Control | Regular CT angiography controls | Regular CT angiography controls |
| Contraindications | Inappropriate aortic anatomy, narrow vascular pathways | Inappropriate thoracic aortic morphology |
| Advantages | Less blood loss, shorter hospital stay | Lower mortality compared to open surgery |
Which Diseases Do Modern EVAR and TEVAR Methods Treat?
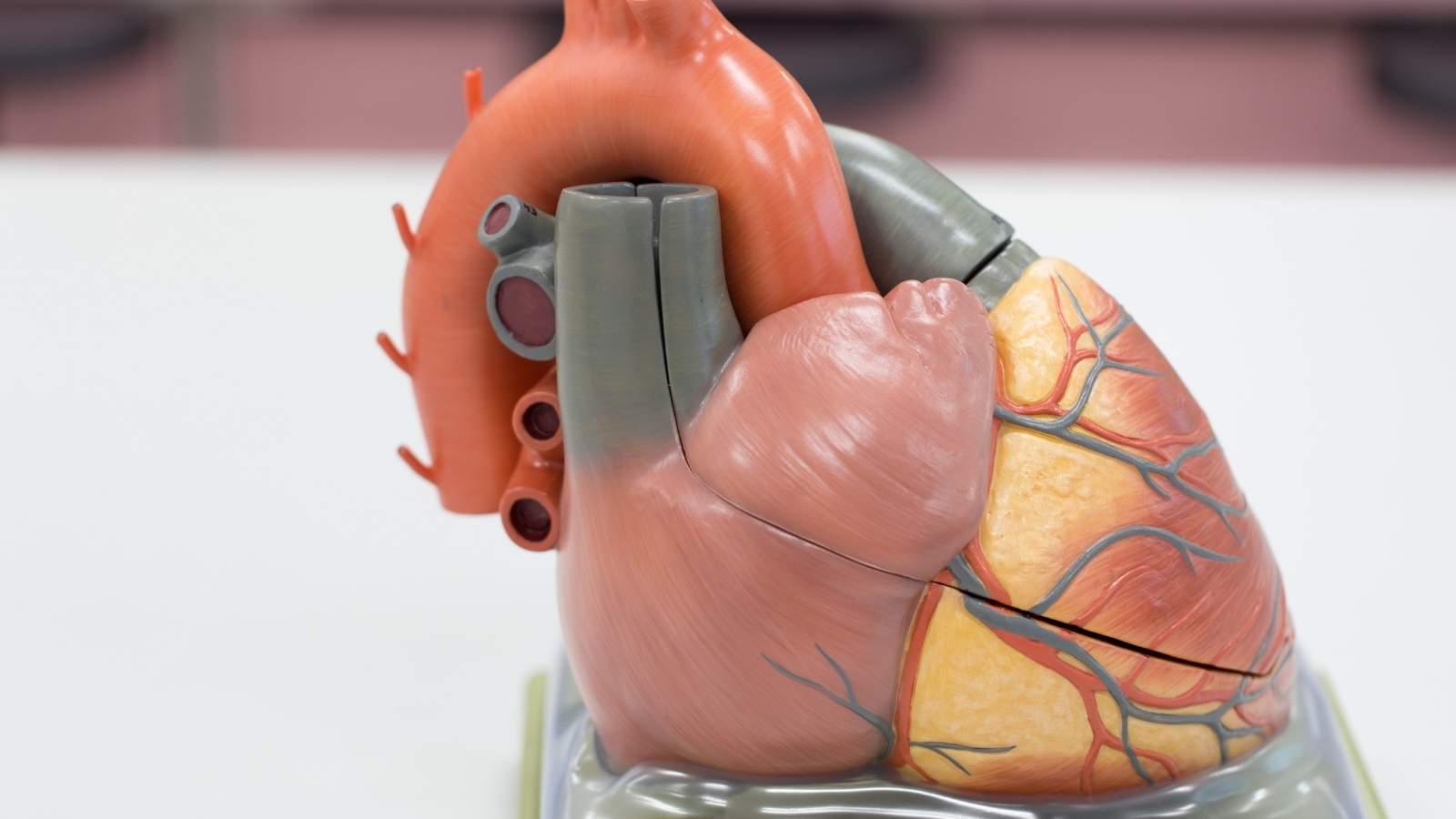
The target of the EVAR and TEVAR methods is the aortic aneurysm. Imagine the aorta as a layered, solid tube through which high-pressure blood flows. Over time, when the fibers that provide the flexibility and strength in the wall of this tube weaken, the vessel wall cannot withstand the pressure of the blood and begins to leak outward. Medically, an aneurysm is when a vessel expands more than one and a half times its normal diameter or, in practical terms, when the aorta in the abdominal region reaches a diameter of 3 centimeters.
The most frightening scenario is when the ballooned vessel wall cannot withstand any more tension and suddenly ruptures (rupture). This is an extremely urgent and life-threatening situation that leads to internal bleeding into the body that is very difficult to stop. Unfortunately, more than half of all rupture cases end in death. This is why aneurysms are referred to as the “silent killer”. Most of the time they cause no pain or discomfort. They are usually detected incidentally during an ultrasound or CT scan for another condition. Therefore, instead of waiting for symptoms to appear, proactively screening those at risk is the smartest way to prevent a potential disaster.
What are the Reasons Why a Person Needs EVAR and TEVAR Treatment?
Rather than a single cause, an aneurysm is caused by a combination of factors that over time disrupt the structural integrity of the vessel wall. It’s like a chain reaction; one factor triggers another and the process accelerates. There are major risk factors that initiated and accelerated this devastating process.
The most important of these factors are:
- Atherosclerosis (Hardening of the Arteries)
- High Blood Pressure (Hypertension)
- Smoking and Tobacco Products Use
- Genetic and Familial Predisposition
- Advanced Age (especially over 65 years)
- Gender (more common in men)
- Congenital Bifurcation of the Aortic Valve (Bicuspid Aorta)
- Connective Tissue Diseases such as Marfan Syndrome
The most powerful modifiable of these factors is undoubtedly smoking. Cigarettes directly damage the vascular wall with their toxic chemicals, accelerate the process of atherosclerosis to an incredible degree, and multiply the risk of aneurysm formation and rupture of an existing aneurysm many times over. High blood pressure, on the other hand, exerts constant pressure on the already weakened vascular wall, which actually encourages ballooning. Therefore, the most basic ways to reduce the risk of an aneurysm or slow its progression are to quit smoking and keep blood pressure at ideal levels. A family history of aneurysms also significantly increases the risk, so these people need to be more careful and aware.
How Does the Location of the Aneurysm Shape the Treatment Decision Between EVAR and TEVAR?
The aorta passes through both our chest and abdominal cavities. At which stop of this journey the aneurysm occurs can radically change both the symptoms and the method of treatment. This is where the fundamental difference between the EVAR and TEVAR procedures comes into play.
- Abdominal Aortic Aneurysm (AAA): These are aneurysms that develop in the abdominal (abdomen) section of the aorta below the diaphragm. This is the most common type among all aneurysms. The procedure used for the closed treatment of aneurysms in this region is called EVAR (Endovascular Aneurysm Repair).
- Thoracic Aortic Aneurysm (TAA): These are aneurysms that develop in the part of the aorta within the chest (thoracic) cavity. Closed treatment of these aneurysms is called TEVAR (Thoracic Endovascular Aortic Repair).
This distinction is not just a geographical nomenclature. AAAs are overwhelmingly associated with atherosclerosis, whereas in TAAs the role of genetic factors and connective tissue diseases is more prominent. Therefore, the choice between EVAR and TEVAR in a patient depends on the exact location of the aneurysm as determined by tomography. The stent-grafts (artificial vessels) and surgical approach used are designed specifically for the anatomical structure of the abdominal and thoracic aorta.
Which Complaints Suspect an Aneurysm That May Require EVAR and TEVAR Treatment?
It must be emphasized again that most aneurysms do not give any symptoms until they enlarge. However, when they grow and start to put pressure on the surrounding tissues, they may give some clues depending on their location. When these symptoms are noticed, a doctor should be consulted.
Possible symptoms of an abdominal aneurysm (AAA) can be the following:
- A deep and persistent pain in the abdomen or back.
- Pulsing or throbbing around the belly button, as if a second heart is beating inside.
The possible symptoms of an aneurysm in the thoracic region (TAA) are different:
- Pain and tenderness in the chest or upper back.
- Persistent coughing or wheezing due to pressure on the windpipe.
- Coarsening, constriction or cracking of the voice due to pressure on the nerve to the vocal cords.
- Difficulty swallowing due to pressure on the esophagus.
Another potential problem is the formation of a blood clot inside the aneurysm sac. A small clot fragment (embolus) can travel with the blood flow to more distant tissues, such as the legs or internal organs, and block the blood vessels in that area. This can lead to sudden and severe pain and loss of function in the affected organ.
What are the Alarm Bells of an Aortic Rupture Requiring an Emergency EVAR and TEVAR Intervention?
Aneurysm rupture (rupture) or separation of the wall layers (dissection) are among the most urgent conditions in medicine and survival is measured in seconds. These symptoms should prompt you to call 112 without a moment’s hesitation.
Aortic rupture (rupture) is a complete perforation of the wall of the aneurysm and the flow of blood into the body cavity. Symptoms are very sudden and severe:
- A pain that radiates to the back or abdomen, described as “tearing” or “stabbing”, never experienced before.
- Sudden drop in blood pressure due to bleeding inside the body.
- Dizziness and darkening of the eyes.
- Cold sweats and a feeling of fainting (shock picture).
- Excessive acceleration of the pulse.
Aortic dissection is slightly different, where a tear in the lining of the vessel wall occurs and blood enters through the tear, separating the layers of the vessel. This can mimic a heart attack:
- Very severe chest pain in the back, wandering and tearing.
- Sudden onset of shortness of breath.
- Stroke-like symptoms such as weakness on one side of the body, speech impairment.
- Significant difference in pulse or blood pressure between the two arms.
What is the Diagnosis and Planning Process for a Successful EVAR and TEVAR Surgery?
Accurate diagnosis and meticulous surgical planning are the foundation for the success of delicate procedures such as EVAR and TEVAR. This process is like a step-by-step journey and each stage determines the safety and success of the next.
The basic methods used in the initial suspicion or screening phase are the following:
- Abdominal Ultrasonography: The most commonly used, easy, inexpensive and harmless method for diagnosing abdominal aneurysms.
- Roentgenogram of the chest: Sometimes it can raise suspicion by showing an enlarged aortic shadow when pulled for another reason.
- Echocardiography (ECHO): It is a cardiac ultrasound and is useful in evaluating the first section where the aorta exits the heart.
Once the suspicion has been confirmed and the treatment decision has been made, we move on to detailed imaging, the “gold standard” of surgical planning. This stage allows the surgeon to draw the roadmap for the surgery.
Computed Tomography Angiography (CTA): This method is indispensable for both EVAR and TEVAR. A special dye is injected into the vessel and the CT scan creates a three-dimensional, millimeter-detailed map of the aorta. With this map, the surgeon can see the exact location of the aneurysm, its diameter, length, and its neighborhood with critical structures such as the renal vessels. These measurements are vital for selecting the most suitable stent-graft (artificial vessel) for the patient’s anatomy.
Magnetic Resonance Angiography (MRA): It is an excellent radiation-free alternative for patients who are allergic to the iodized dye used in tomography or who have sensitive kidney function.
At what point are surgical interventions such as EVAR and TEVAR decided?
Not every patient with an aneurysm needs immediate surgery. This is one of the most common questions our patients ask: “When should I have surgery?” In making this decision, we weigh the risk of rupture of the aneurysm against the potential risks of surgery. Libra weighs heavily in favor of surgery at the point where the risk of rupture outweighs.
For small and asymptomatic aneurysms, a strategy of “active surveillance” or “watchful waiting” is followed. During this process, the patient is followed up with imaging tests at regular intervals (usually 6 months or 1 year) to see changes in the size of the aneurysm.
There are main situations that trigger the decision for surgery.
- Size: This is the most important criterion. Abdominal aneurysms (AAA) usually recommend surgery when they reach a diameter of 5.5 cm in men and 5.0 cm in women. In thoracic aneurysms (TAA), this limit is around 5.5-6.0 cm.
- Rapid Growth: Regardless of size, if the aneurysm grows by more than 0.5 cm in 6 months or more than 1 cm in a year, this is a sign of an increased risk of rupture and requires treatment.
- Symptoms: If the aneurysm starts to cause symptoms, such as pain, regardless of its size, this indicates that it is time for intervention.
- Special Conditions: In genetic diseases such as Marfan syndrome or those with a family history of rupture, the decision to operate can also be made in smaller scopes.
How is Traditional Open Surgery an Option Versus EVAR and TEVAR Methods?
The popularity of closed methods such as EVAR and TEVAR should not lead to the mistaken belief that traditional open surgery has been abandoned. Open surgery is the “gold standard” method of aneurysm treatment, which has been successfully applied for many years and whose long-term results are well known. In this method, a large incision is made in the abdominal or chest wall to access the site of the aneurysm directly, remove the damaged section and replace it with a healthy artificial vessel (graft) made of a synthetic material such as dacron.
Open surgery may still be the best option, especially for patients who are young, have no additional serious health problems and have a long life expectancy. Because this method eliminates the need for lifelong follow-up and potential additional intervention required by closed methods. In other words, open surgery is not an outdated method, but a valuable treatment option that has its own advantages and offers the most permanent solution for the right patient. The decision on which method is best for the patient is made on an individual basis, based on the patient’s age, general health and the anatomical structure of the aneurysm.
How are EVAR and TEVAR Procedures Implemented Step by Step and What is the Improvement Process?
EVAR and TEVAR procedures are performed under general or regional anesthesia (lumbar anesthesia) in a setting similar to an angiography unit. The logic is to solve the problem by using the vascular system from the inside, without making a large incision.
In general terms, the process involves the following steps.
- Introduction: Small incisions are made to access the arteries in both groins (femoral artery).
- Catheter Placement: Through this incision, a thin, flexible tube (catheter system) carrying the stent-graft is inserted into the artery.
- Guidance: Under X-ray (scopy) visualization, the surgeon carefully guides the catheter through the artery to the site of the aneurysm.
- Insertion: Once in the correct position, the stent-graft is released in a controlled manner. Like a spring, the graft is released and anchors itself firmly to the intact vessel wall at the beginning and end of the aneurysm.
- Control and Closure: After angiography confirms that blood is flowing smoothly through the new pathway and that there is no leakage into the aneurysm sac, the catheter is removed and the small incisions in the groin are sutured closed.
These procedures usually take 1 to 3 hours. The recovery process is much faster compared to open surgery. Patients usually stay in hospital for 1-3 days, are up and walking the next day and can return to their daily life in as little as 2-4 weeks.
What to Pay Attention to in Life After EVAR and TEVAR and What is Endoconstriction?
The success of the surgery does not only end in the operating room; the patient’s postoperative lifestyle and adherence to follow-ups directly affect the long-term durability of the treatment. There are some important lifestyle changes that our patients should follow after EVAR and TEVAR.
These changes aim to protect the entire vascular system, not just the implanted graft:
- Quitting smoking completely.
- Measuring blood pressure regularly and keeping it under control with medication.
- Lowering cholesterol levels (usually statin drugs are required).
- Eating a healthy and balanced diet.
- Regular and moderate exercise as approved by the physician.
What is Endoleak (Endos leakage)?
The most common complication of closed aneurysm repair, and the one that requires the closest follow-up, is “endoleak” or endos leakage. This is when, despite stent-graft placement, somehow blood continues to leak into the aneurysm sac. This leakage can cause the sac to come under pressure again, enlarge and put it at risk of rupture again. This is why regular follow-up after EVAR and TEVAR is vital. There are different types depending on the source of the complaint. Some types (e.g. Type II) are usually harmless and resolve on their own, but others (e.g. Types I and III) are high risk and require additional intervention.
Why Lifelong Follow-up is Essential After Successful EVAR and TEVAR Treatment
One of the most important features of EVAR and TEVAR treatment is that it requires regular follow-up for life. This may sound like a daunting concept for our patients, but it should not be seen as a burden, but as a guarantee for the protection of the investment made and the health gained. This is a health partnership between the patient and the physician that will last for years.
The follow-up program includes an imaging (usually CT scan) check-up, usually at 1, 6 and 12 months after surgery, and then once a year for life if all is well.
These regular checks have a basic purpose:
- To confirm that the stent-graft is in place and intact.
- To catch a possible endos leak (endoleak) at an early stage.
- Measure the dimensions of the aneurysm sac (the expectation is that the sac will shrink or at least remain stable).
- To check the graft for any slippage, shrinkage or structural distortion.
These simple annual check-ups are part of the comfort and rapid recovery that the closed method offers. This way, our patients can continue their lives with confidence, knowing that the treatment remains successful for many years to come.
Frequently Asked Questions
What is EVAR?
EVAR (EndoVascular Aneurysm Repair) is a minimally invasive procedure that treats aortic aneurysms in the abdominal region with a closed approach.
What is TEVAR?
TEVAR (Thoracic EndoVascular Aneurysm Repair) is the closed repair of aortic aneurysms in the thoracic region.
What is the difference between EVAR and TEVAR?
EVAR is applied to the abdominal aorta and TEVAR is applied to the thoracic aorta.
Why do these procedures?
It is used to repair dilatations in the aortic wall (aneurysms) before they burst and to prevent life-threatening conditions.
How to make EVAR and TEVAR transactions?
Through the muscular artery, a special device called a stent-graft is inserted into the aorta and the damaged area is supported.
Are these procedures safer than open surgery?
Yes, there is usually less risk, the hospital stay is shorter and recovery is faster.
Who is eligible for EVAR or TEVAR?
Patients with aortic aneurysms and vasculature suitable for stent placement are suitable.
What is the recovery process after EVAR and TEVAR?
Discharge is usually within 1 to 2 days. The pain is minimal and patients can return to normal life in a short time.
Do stents last forever?
Yes, it is permanent. However, its position and function should be monitored with regular checks.
What should be considered after EVAR or TEVAR?
Blood pressure control, regular follow-up imaging and a lifestyle to maintain vascular health are recommended.
How long do these procedures take?
Most EVAR and TEVAR procedures are completed in 1 to 3 hours and are performed under general anesthesia.
Is there a risk of complications?
In rare cases, complications such as stent displacement, vessel occlusion or endoleak may occur.
Which doctors perform these procedures?
It is usually performed by cardiovascular surgeons or interventional radiologists.
Are EVAR and TEVAR procedures covered by SSI?
In Turkey, if there is an indication and it is performed in a public hospital, in most cases it is covered by the SSI.
Is every aneurysm patient a candidate for EVAR or TEVAR?
No, factors such as vessel structure, location and diameter of the aneurysm are decisive for suitability.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.