Chest cage pain is a common complaint with causes ranging from musculoskeletal strain to life-threatening heart or lung conditions. Proper evaluation is crucial to distinguish between benign and serious origins of thoracic pain.
Musculoskeletal causes such as costochondritis, trauma, or muscle strain are frequent and often present with localized tenderness. These conditions typically improve with rest, pain relievers, and physical therapy interventions.
Cardiac causes include angina, myocardial infarction, or pericarditis. In such cases, chest pain is often associated with shortness of breath, dizziness, and radiating discomfort, necessitating urgent medical attention.
Pulmonary causes such as pulmonary embolism, pleurisy, or pneumonia can also trigger chest cage pain. Diagnosis relies on clinical examination, imaging, and laboratory tests, while treatment varies depending on the underlying disease.
| Possible Causes | Cardiac: angina, heart attack – Pulmonary: pulmonary embolism, pleurisy, pneumonia – Gastrointestinal: reflux, esophagitis – Musculoskeletal: costochondritis, muscle strain – Psychogenic: anxiety, panic attacks |
| Emergency Indicators | Severe chest pain, radiating to the left arm/jaw, shortness of breath, sweating, altered consciousness |
| Characteristics of Pain | Pressure, burning, stinging, compressive; varies according to duration and localization |
| Diagnostic Methods | ECG, chest radiography, CT angiography, blood tests (troponin, D-dimer), endoscopy |
| Differential Diagnosis | Myocardial infarction, reflux disease, costochondritis, anxiety disorder |
| Treatment Methods | Depends on the cause: emergency medical treatment for cardiac causes, analgesics and rest for musculoskeletal disorders, antacids for reflux |
| When is an emergency intervention needed? | Chest pain accompanied by shortness of breath, dizziness, palpitations or loss of consciousness |
Why Sternum Pain Should Always Be Taken Seriously?
A pain in the chest area naturally worries many people and the first thing that comes to mind is a heart attack. This concern is not unfounded, as this pain can indeed be the first signal of a life-threatening condition. But there is another side to the coin. A significant proportion of chest pain can actually be caused by digestive, lung, musculoskeletal or even psychological stress. Our body’s nervous system is very complex. Pain signals from different organs such as the heart, esophagus and lungs reach the brain via common nerve pathways. For this reason, the brain can sometimes misinterpret the true source of pain. In medicine, we call this “reflected pain”. This is why the pain of a heart problem can be felt in the jaw, back or arm. This complexity makes self-diagnosis impossible and extremely dangerous. So the rule is simple: Any chest pain that is new onset, severe or of unknown origin should be evaluated by a physician.
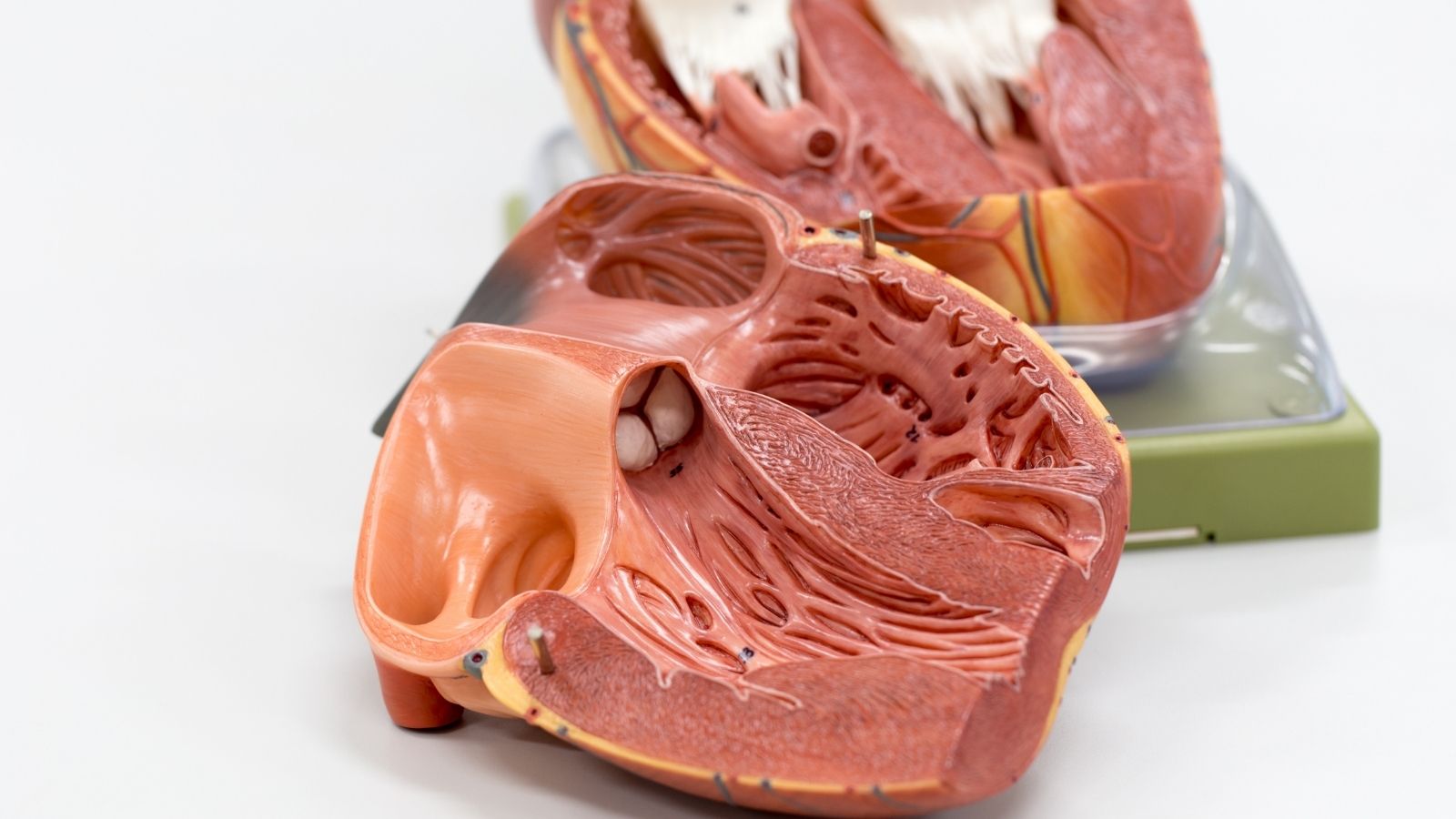
Which Heart Problems Cause Sternum Pain?
The most urgent and life-threatening causes of chest pain are those originating in the heart and major blood vessels. In these cases, a sudden disruption of blood flow can have serious consequences within minutes. It is therefore vital to recognize these symptoms.
Heart Attack (Acute Coronary Syndrome)
This is a generic name for conditions that occur when blood flow in the coronary arteries that supply the heart is suddenly and critically reduced. Almost all of them are caused by atherosclerosis, a build-up of fat and cholesterol deposits called “plaques” that have accumulated on the artery walls over the years. The problem starts when one of these plaques suddenly cracks. The body recognizes this crack as a wound and sends a blood clot to repair it. This clot quickly blocks the blood vessel, cutting off blood and oxygen to the heart muscle. Deprived of oxygen, the heart muscle screams for help with the famous chest pain called “angina”. If the blockage is not opened quickly, the heart muscle cells begin to die irreversibly. This is called a heart attack or myocardial infarction.
The classic pain suggestive of a heart attack is a feeling of pressure, tightness or heaviness, usually in the center or slightly to the left of the chest. Patients often describe it as “like an elephant sitting on my chest” or “like my chest is being squeezed with a vice”. This pain does not stay in one spot, but tends to spread.
The areas where pain can spread are:
- Left arm (most common)
- Both arms
- Shoulders
- Neck
- Jaw
- Back (between the shoulder blades)
- Stomach area (upper abdomen)
This pain is often accompanied by other symptoms. It is very important to recognize these accompanying symptoms.
Other symptoms of a heart attack include
- Cold and sticky sweating (diaphoresis)
- Sudden onset of shortness of breath
- Nausea and sometimes vomiting
- Feeling dizzy or lightheaded
- Excessive and sudden onset of weakness, fatigue
- Intense anxiety or a feeling that “something bad is going to happen”
It should be noted that women, the elderly and diabetics in particular may not experience these typical symptoms. In them, a heart attack may only be manifested by a sudden shortness of breath, extreme fatigue or indigestion.
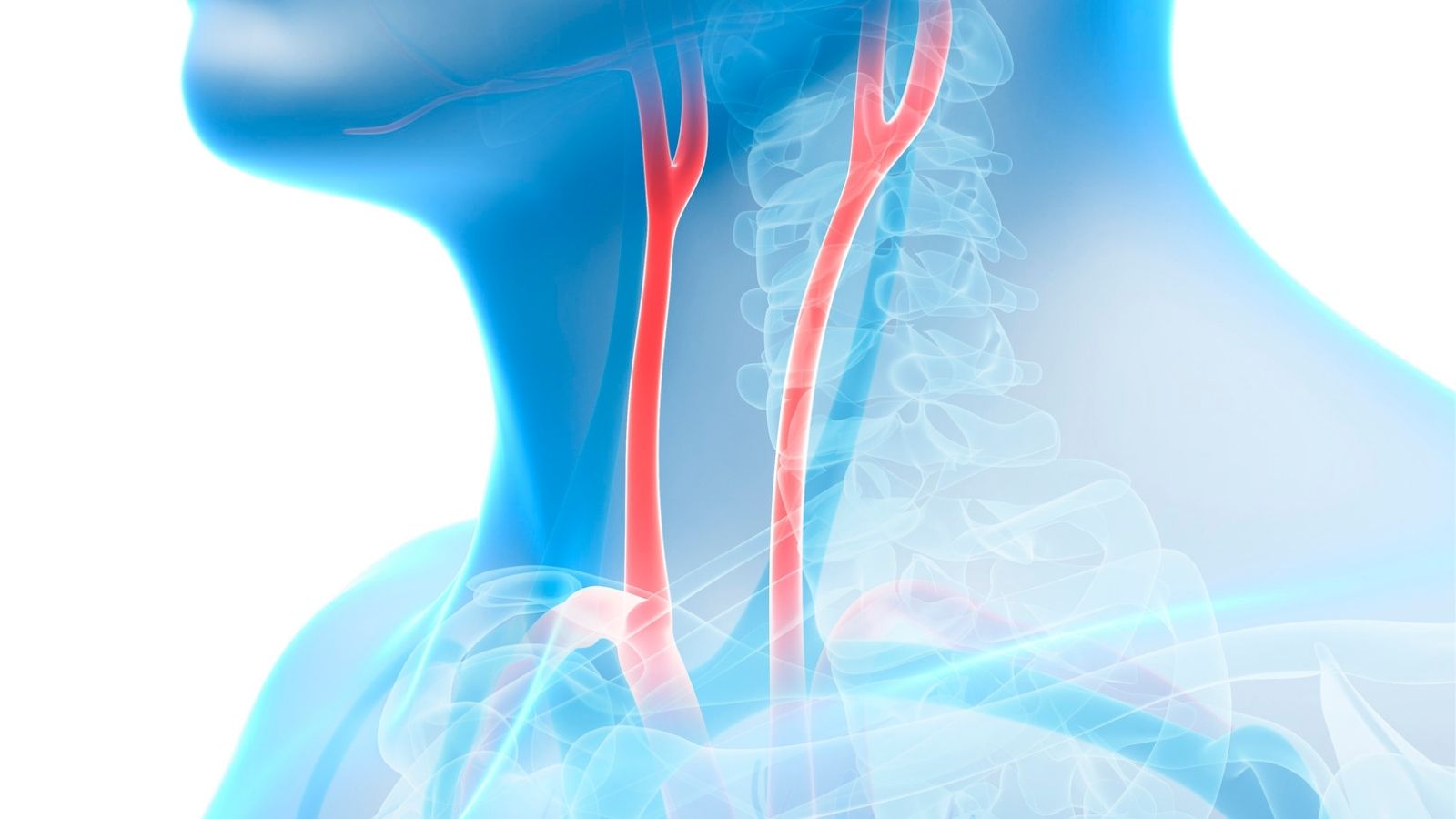
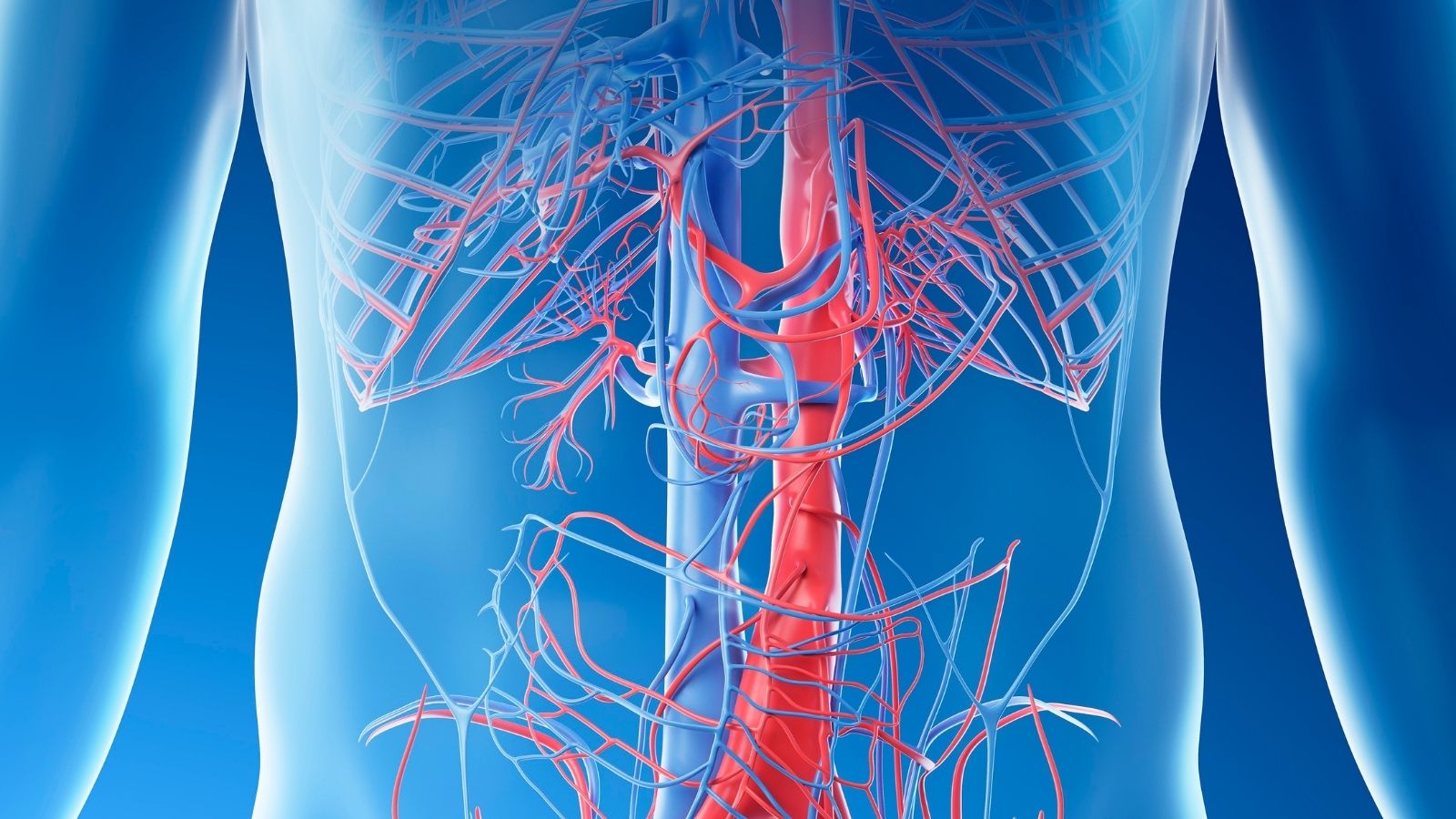
Aortic Rupture (Aortic Dissection)
This is completely different from a heart attack, but just as urgent. It is an internal rupture of the wall of the aorta, the main artery of the body that exits the heart. It is usually caused by a weakening of the aortic wall due to uncontrolled high blood pressure or certain genetic diseases. The most typical symptom is a sudden onset of unprecedented, unusually severe pain, described as “stabbing” or “tearing”. The pain is usually felt in the chest or back, between the shoulder blades and can radiate into the abdomen as the tear progresses. This is a fatal vascular catastrophe that requires urgent surgical intervention.
Pulmonary Embolism (Pulmonary Embolism)
This is when a blood clot, usually in the veins of the legs, breaks off and travels through the bloodstream to block one of the lung vessels. Although it occurs in the lung, the consequences directly affect the heart. The blockage puts a sudden strain on the right side of the heart and can lead to right-sided heart failure. The pain of a pulmonary embolism is usually different. It is a sharp, stabbing pain that increases markedly with deep breathing or coughing. This is known as “pleuritic pain”.
The other most common symptoms are:
- Sudden onset and unexplained shortness of breath
- Accelerated heartbeat (palpitations)
- Rapid breathing
- Coughing up phlegm, sometimes with blood
- Dizziness or fainting
Can Sternum Pain Be Caused by Stomach or Muscle?
Yes, and quite often. In a significant proportion of patients presenting to emergency departments with chest pain, the cause is non-cardiac. However, these diagnoses are always made after the most dangerous cardiovascular diseases have been definitively ruled out. This is a security measure.
Stomach and Intestinal System Pain
The close proximity of the esophagus to the heart in the rib cage often causes pain from this area to be confused with heart pain.
Reflux (Gastroesophageal Reflux Disease – GERD): The most common cause of non-cardiac chest pain. It occurs when stomach acid backs up into the esophagus. It usually causes a burning sensation behind the breastbone, also known as “sternum burning”. This pain can sometimes resemble the pressing sensation of heart pain. There are some clues that make pain suspicious of reflux.
Conditions that trigger or increase reflux pain:
- After fatty or spicy dishes
- Consuming large portions
- Lying down immediately after a meal
- Leaning forward
In addition, digestive system symptoms such as bitter water in the mouth, belching and bloating also suggest reflux.
Other Digestive Problems: Gallbladder inflammation can cause pain radiating to the right upper abdomen and back, especially after a fatty meal. Pancreatitis or stomach ulcers can also cause pain that radiates to the chest.
Musculoskeletal Pain
Pain from the muscles, bones and cartilage that make up the chest wall is also quite common. The main characteristic of these pains is that they usually occur with movement or touch.
Costochondritis Inflammation of the cartilage that connects the ribs to the breastbone. It is very common. The most typical feature of the pain is that the tenderness or pain is re-triggered by pressing a finger on certain points on the sides of the breastbone. Movements such as deep breathing, coughing or twisting the trunk can increase the pain.
Muscle Strains Lifting something heavy, straining during sports or even a severe coughing fit can cause a chest muscle strain. This pain is usually in a specific area and worsens with movements that exercise that muscle.
When and Which Doctor Should I Go to for Sternum Pain?
The most critical decision you have to make when you experience chest pain is whether to seek emergency help. Given the consequences, it is always better to be overly cautious. When in doubt, call 112 Emergency Services. Trying to get to the hospital on your own risks worsening your condition on the way. Emergency responders can start life-saving treatments until they reach the hospital.
If any of the following “red flag” symptoms are present, emergency help should be called without waiting a second:
- Feeling of pressure, tightness, heaviness or crushing in the chest
- Sudden onset of severe, tearing pain in the chest or back
- Pain that does not go away with rest and lasts longer than a few minutes
- Pain radiating to the arms, neck, jaw or back
- Severe shortness of breath accompanied by pain
- Cold and sticky sweating
- Nausea or vomiting
- Fainting or severe dizziness
- Significant blood pressure or pulse difference between the two arms
The first place to go with chest pain is the emergency department of a hospital. After the initial evaluation, you may be followed up by a Cardiology or Cardiovascular Surgery specialist, depending on the underlying cause. If the problem is related to the musculoskeletal system, you may need to be referred to Physical Therapy and Rehabilitation, and if it is related to the digestive system, you may need to be referred to Gastroenterology.
How is chest pain diagnosed?
When you arrive at the emergency room, doctors race against time to quickly rule out life-threatening conditions. During this process, some basic tests are carried out immediately.
Electrocardiogram (ECG): This simple and painless test, which records the electrical activity of your heart through electrodes attached to your chest and limbs, is performed in seconds. It is the most important way to immediately diagnose major heart attacks (STEMI), especially those requiring emergency vascularization. But remember, a normal ECG does not mean there is no heart problem. Sometimes it can take time for changes to appear, so the test may need to be repeated at regular intervals.
Cardiac Troponin Blood Test: Troponins are proteins that enter the bloodstream when the heart muscle is damaged. Today’s high-sensitivity troponin tests can detect even the slightest heart damage. Just like an ECG, troponin levels can take time to rise. For this reason, a blood sample is usually taken when you arrive at the emergency room and again a few hours later to see if there is an increase in levels. Elevated troponin levels are conclusive evidence of a heart attack.
Depending on the results of these initial and most critical tests, further imaging modalities may be used to clarify the diagnosis or investigate other possible causes.
Some of these are:
Chest X-ray It may indicate conditions such as pneumonia or collapse of the lungs, signs of heart failure or an enlargement of the aorta.
Computed Tomography (CT) Angiography: This special CT scan with intravenous dye is the gold standard method for clearly visualizing pulmonary embolism or aortic rupture.
Echocardiography (ECHO): Ultrasound of the heart. Sound waves are used to examine the heart’s structure, valves and contractility. During a heart attack, it may indicate that a part of the heart muscle is not contracting well.
Coronary Angiography: The “gold standard” method for imaging the heart vessels. The heart vessels are accessed with a thin tube (catheter) inserted into an artery, usually at the wrist or groin. A dyed substance is injected into the vessels and films are taken. This allows the location and severity of stenosis or blockage to be clearly determined. Often, if a blockage is found, it can be treated with a balloon and stent procedure in the same session.
How to treat sternum pain?
Treatment depends entirely on the underlying cause of the chest pain. If the situation is urgent, the aim is to solve the problem quickly and prevent permanent damage.
Treatment of Cardiovascular Occlusion (Angioplasty and Bypass)
Balloon and Stent (Percutaneous Coronary Intervention – PCI): This is now the most common treatment for heart attacks and severe vascular stenosis. The blocked vessel detected during coronary angiography is opened with a wire with a tiny balloon at the end. By inflating the balloon, the plaque is crushed and the vascular access is opened. Then a small tube made of wire, called a “stent”, is permanently inserted into the vein to prevent it from closing again.
Coronary Bypass Surgery (CABG): This open heart surgery, commonly known as “bypass”, may be a better option for patients with blocked main arteries, especially those with severe stenosis in multiple arteries, or those with comorbidities such as diabetes. The logic of the surgery is to create a new pathway, a bridge, to bring blood beyond the blocked vessel.
The vessels used to create these bridges (grafts) are
- The artery inside the chest wall (LIMA)
- Artery in the arm (Radial artery)
- Vein in the leg (Safhen vein)
Using one of these vessels, the surgeon sutures one end to the aorta, the main artery, and the other end beyond the blocked area. The blood then “bypasses” the blockage and continues to supply the heart muscle.
Aortic Rupture Treatment
A ruptured aorta in the first part that exits the heart (Type A) is the most dangerous and requires emergency surgery as soon as it is diagnosed. In this complex open-heart surgery, the torn aorta is removed and replaced with a synthetic vascular graft called “Dacron”. If the tear is in a lower area (Type B), the condition is usually managed primarily with medication and very tight control of blood pressure. However, if complications such as bleeding or organ malnutrition develop, the ruptured area can be closed from the inside with a stent-graft using an endovascular (closed) method called “TEVAR”, which is performed through the groin.
What can be done to avoid chest pain in the future?
Modern medicine and surgery have achieved incredible success in the treatment of cardiovascular diseases. But the best treatment is undoubtedly prevention. Lifestyle changes to protect your heart health and avoid similar problems in the future are just as valuable as surgery.
Here are steps you can take to protect your heart health:
- Keep your high blood pressure under control.
- Manage your cholesterol levels.
- Strictly control your diabetes, if you have it.
- Stop smoking and all tobacco products immediately.
- Achieve and maintain a healthy weight.
- Get regular physical activity (such as brisk walking for at least 150 minutes a week).
- Adopt a Mediterranean-style diet rich in vegetables, fruits and whole grains.
- Avoid processed foods, sugary drinks and saturated fats.
- Find healthy ways to manage your stress (meditation, yoga, hobbies).
Remember that chest pain is an important message your body is sending you. Reading this message correctly, seeking timely professional help and then taking care of your lifestyle is the key to a healthy and long life.
Frequently Asked Questions
What is rib cage pain?
Rib cage pain is a condition characterized by pain originating in the ribs, muscles, cartilage structures or internal organs.
Is chest pain a sign of a heart attack?
Yes, it may indicate a heart attack, especially if it is pressing, radiating to the left arm, accompanied by shortness of breath and sweating. However, not all chest pain indicates a heart attack and must be evaluated.
What are the common causes of sternum pain?
Muscle strains, costochondritis, traumas, reflux, anxiety and cardiovascular diseases are the main causes.
Does costochondritis cause chest pain?
Yes, costochondritis is an inflammation of the rib cartilages and causes localized pain, which is increased especially with movement.
How to recognize chest pain?
Pain from the heart is usually unchanged by movement. Musculoskeletal pain, on the other hand, increases with pressure or movement. In case of doubt, a physician should be consulted.
What does it mean if chest pain increases when breathing?
It usually indicates musculoskeletal problems or involvement of the lining of the lungs (pleura).
Which tests evaluate chest pain?
ECG, chest X-ray, blood tests and, if necessary, imaging methods such as CT and MRI are used.
Do psychological causes cause chest pain?
Yes, chest tightness or stabbing pain can occur, especially during anxiety and panic attacks.
Which doctor to see for sternum pain?
It can start with the family doctor, followed by referral to cardiology, pulmonology or orthopedics depending on the condition.
When is chest pain an emergency?
Severe, sudden onset, accompanied by symptoms such as shortness of breath, fainting or jaw-arm pain, requires urgent intervention.
Does chest pain occur in children?
Yes, it can develop due to stress, muscle strain or posture disorders, especially in growing children.
Can reflux cause pain in the chest?
Yes, when stomach acid escapes into the esophagus, it can cause burning, pressure and pain in the chest.
What can be done at home for chest pain?
Rest, hot and cold applications, painkillers and stress-reducing techniques can be helpful. However, prolonged pain requires medical evaluation.
What does chest pain with back pain indicate?
Serious conditions such as spinal problems, muscle strains or, rarely, aortic dissection can be considered. If these symptoms are present, consult a doctor without delay.
Does chest pain go away completely?
It depends on the cause. While musculoskeletal pain usually resolves with treatment, some cases may require long-term follow-up. Do not despair, early diagnosis and appropriate treatment can often lead to a full recovery.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.