Heart valve calcification and degeneration refer to progressive structural changes in the valve tissue. These conditions impair valve opening and closure, leading to restricted blood flow, heart strain, and potential development of heart failure if left untreated.
Risk factors include aging, chronic kidney disease, hypertension, and metabolic disorders. Early symptoms may present as shortness of breath, chest pain, or fainting. Echocardiography remains the gold standard for diagnosis and evaluation of severity.
Treatment options vary depending on disease stage, ranging from medication to surgical valve replacement or transcatheter valve implantation (TAVI). Early intervention prevents further deterioration and improves patient prognosis significantly.
Long-term management requires regular cardiology follow-up, lifestyle modifications, and strict control of comorbidities. Preventive care plays a major role in reducing complications and maintaining functional heart performance in affected patients.
| Medical Term | Valve degeneration or calcific valve disease |
| Definition | Calcium deposits in the heart valves, resulting in decreased motion and/or structural deterioration |
| Most Frequently Affected Cover | Aortic valve (aortic stenosis) – Less frequently mitral valve (mitral annular calcification) |
| Main Causes | Aging, hypertension, hypercalcemia, chronic kidney disease, hyperlipidemia |
| Symptoms | Initially asymptomatic – As it progresses, shortness of breath, chest pain, fainting, palpitations |
| Physical Examination Finding | Murmur – Systolic ejection murmur in aortic stenosis |
| Diagnostic Methods | Echocardiography (valve thickness and restriction of motion), ECG, chest radiography, CT (for calcium score) |
| Complications | Heart failure, arrhythmias, syncope, sudden death |
| Treatment Methods | Follow-up in mild cases – Surgical valve replacement in severe cases |
| Follow-up Process | Clinical and echocardiographic monitoring – Intervention is planned if there is symptom development or EF decline |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is heart valve calcification and how does it affect the heart?
The valves in your heart are normally extremely thin and flexible structures. However, when the calcification process begins, calcium, cholesterol and various mineral deposits begin to build up on these valves. This deposit gradually thickens and hardens the valve leaflets, severely limiting their mobility.
This complex process is usually triggered by damage to the protective layer of cells lining the surface of the valves. Factors such as high blood pressure or irregularities in blood flow can cause this initial damage. The damaged area acts as a magnet for bad cholesterol (LDL) and other fats in the blood to stick to. When our body perceives this deposit as a threat, it initiates a defense mechanism and sends immune cells to the area. This leads to a chronic inflammation that we are not aware of.
The most critical stage of the process is when this inflammation causes normal cells in the valve tissue to change character and become bone-forming cells. These abnormal cells begin to deposit calcium, just like our skeletal bones. As a result, the valve tissue, which should be flexible, becomes “petrified” and hardened.
The end result of this process is a dangerous narrowing of the valve opening. In medicine, we call this stenosis. Your heart has to work with much more force than normal to get the blood the body needs through this narrow door. Over time, the heart muscle, which is constantly working against this high pressure, becomes tired, thickens, and eventually fails. Therefore, a problem that starts in the valve, if left untreated, turns into a condition that threatens the health of the entire heart.
What causes heart valve calcification and who is most at risk?
Heart valve calcification is not caused by a single cause but by a combination of factors. These risk factors largely overlap with the factors that lead to the development of atherosclerosis. We can categorize these factors into two groups: those that we cannot intervene and those that we can control.
Some risk factors are unfortunately beyond our control. These unchangeable factors are:
- Advancing age
- Male gender (especially for aortic valve)
- Family history of valve disease (genetic predisposition)
- Congenital valve anomalies (e.g. bicuspid aortic valve)
Fortunately, there are risk factors that we can influence and control by maintaining our overall heart health. These modifiable risk factors are as follows:
- Cigarette smoking
- High blood pressure (hypertension)
- High cholesterol and triglycerides
- Diabetes (diabetes)
- Chronic kidney disease
- History of rheumatic fever
- Radiotherapy to the chest area
Being aware of these factors is a warning for people, especially those at risk, to keep regular medical check-ups and adopt healthy living habits. For example, having a congenital aortic valve with two leaflets can bring the calcification process forward by decades and lead to severe valve stenosis at a much earlier age than normal. Similarly, smoking or leaving high blood pressure uncontrolled significantly accelerates this process.
Which heart valves are more commonly affected by calcification?
Although your heart has four valves, calcification overwhelmingly affects the aortic and mitral valves on the left side of the heart. The reason for this is quite simple: physics and pressure.
The left side of your heart has the heavy workload of pumping cleansed blood at high pressure throughout the body. This high-pressure system causes the aortic and mitral valves to be subjected to more mechanical stress with each beat, and the blood flow through these valves becomes more turbulent. Scientific evidence shows that calcium deposition is concentrated precisely in areas of this turbulent and stressful flow.
In contrast, the tricuspid and pulmonary valves on the right side of the heart are subjected to less stress because they only send blood to the lungs, i.e. into a much lower pressure circulation. Therefore, calcification of the valves on the right side is extremely rare.
Aortic Valve Calcification: The valve most commonly affected by calcification is the aortic valve, the main outlet of your heart. Since it is located just at the exit of the left ventricle, which pumps blood throughout the body, it is exposed to the highest pressure and the fastest blood flow. This makes it the most vulnerable valve to calcification.
Mitral valve calcification: The second most commonly affected valve is the mitral valve, located between the left atrium and the left ventricle. Calcification of the mitral valve usually progresses in a different way to that of the aorta and mostly affects the annulus, the ring-shaped structure where the valves sit. This may cause both stenosis and leakage by restricting valve movements.
What symptoms does heart valve calcification cause?
One of the most deceptive aspects of heart valve calcification is that it can progress completely silently and insidiously over many years. Your heart muscle works extraordinarily hard to compensate for the increased workload created by the narrowed valve. For this reason, patients can go on living their normal lives for years, even decades, without any symptoms. During this asymptomatic period, the disease is often discovered by chance during a routine medical examination for another reason, when the doctor hears a non-innocent sound called a “murmur” while listening to the heart with a stethoscope.
However, when the stenosis reaches a critical level, the heart’s compensatory mechanisms can no longer carry the load. At this point, symptoms begin to appear during physical activities when the body’s oxygen demand increases. The appearance of these symptoms is an alarm that the disease has progressed to an advanced stage and requires urgent medical evaluation. Especially in severe aortic stenosis, the “classic triad of symptoms” is characterized by urgent complaints.
This classic triad of symptoms are:
- Shortness of breath
- Chest pain (angina)
- Dizziness or fainting (syncope)
In addition to these main symptoms, other symptoms may also occur due to valve calcification. Other possible symptoms include:
- Increased fatigue and weakness
- Palpitations
- Swelling in the feet and legs (edema)
Shortness of breath is usually the first symptom to appear, and is most common in exertional situations, such as climbing stairs. Fainting is usually the last and most serious symptom, indicating a momentary lack of blood supply to the brain and a risk of sudden death. The presence of any of these symptoms indicates a significantly shortened life expectancy if left untreated.
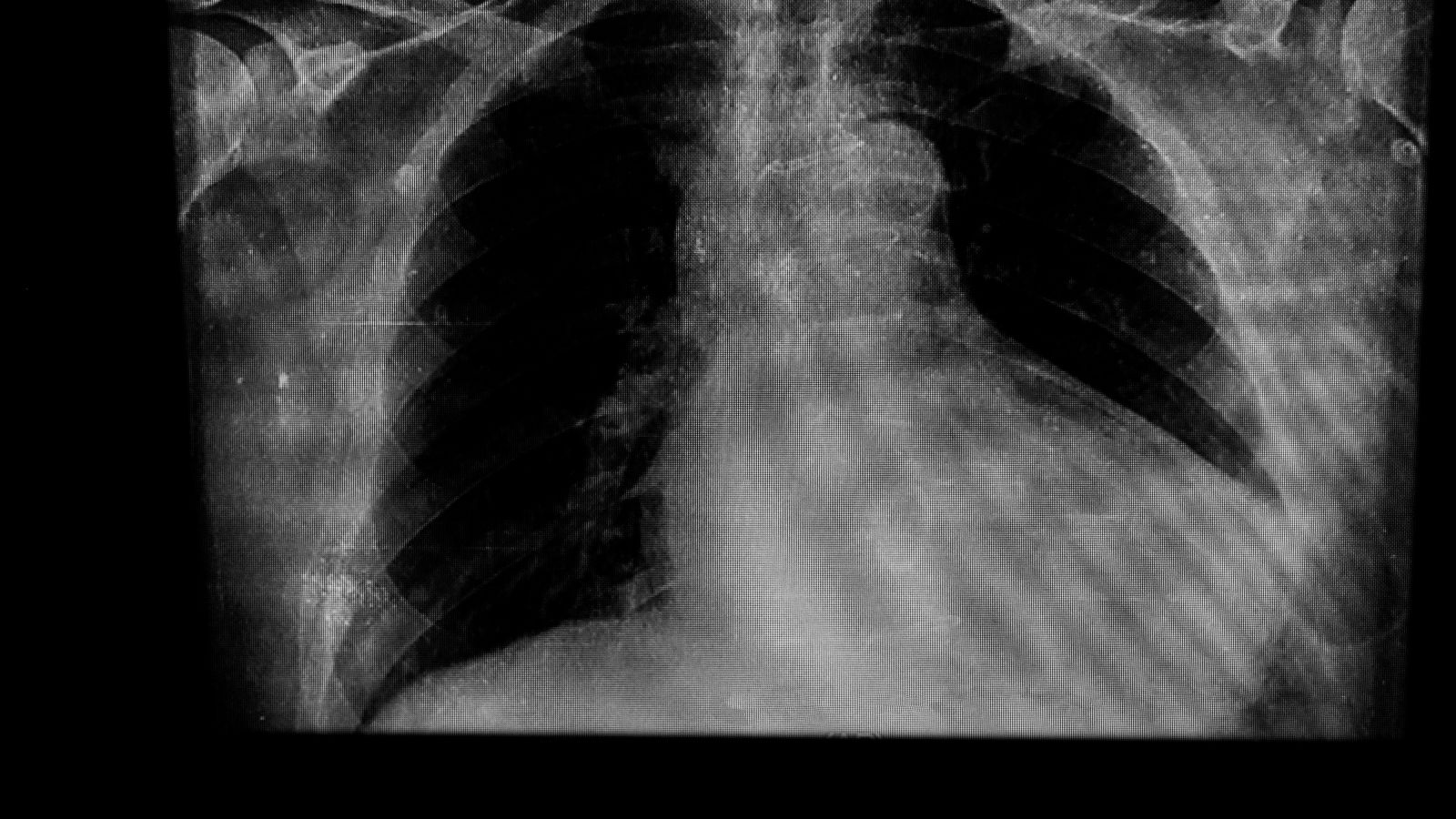
What methods are used to diagnose heart valve calcification?
Calcification of the heart valve is diagnosed through a combination of a careful history, a detailed physical examination and advanced imaging technologies. This process is vital to confirm the presence of the disease, determine its severity and chart the best course of treatment.
The main methods used in the diagnostic process are:
- Physical examination and patient history
- Echocardiography (ECHO or ultrasound of the heart)
- Computed Tomography (CT)
- Electrocardiogram (ECG)
- Chest radiography
- Effort test (stress test)
- Cardiac catheterization (angiography)
The first step in diagnosis is usually for the doctor to listen to your heart with a stethoscope and hear the typical “murmur” created by blood flowing through the narrowed valve. However, the gold standard method for definitive diagnosis and determining the severity of the disease is echocardiography (ECHO). This painless and harmless test uses sound waves to create real-time, moving images of your heart and valves. ECHO clearly shows how thickened and calcified the valve leaflets are, how much their mobility is reduced and whether the stenosis is mild, moderate or severe. It is also assessed whether the pumping power of your heart is affected. Computed tomography (CT) has become an indispensable tool for anatomical measurements of valve and vascular structures, especially when planning modern, non-surgical treatment methods such as TAVI.
Is untreated heart valve calcification a fatal problem?
This question should be answered with a clear and unambiguous “yes”. Severe valvular stenosis, especially when it is symptomatic, is a rapidly worsening and unfortunately fatal disease if left untreated. After the onset of symptoms (shortness of breath, chest pain, fainting), time starts to work against the patient. If the valve is not replaced at this stage, the average life expectancy is reduced to just 2 to 3 years. Some scientific studies have shown that within 5 years of the onset of symptoms, the survival rate can be as low as . These statistics reveal that severe and symptomatic aortic stenosis is even more dangerous than many types of advanced cancer.
Left untreated, a number of dangerous complications begin to develop in your body. Major complications include:
- Heart failure
- Rhythm disorders (arrhythmias)
- Blood clots and stroke (paralysis)
- Pulmonary hypertension
- Sudden cardiac death
The most inevitable consequence of this process is heart failure. The heart muscle, which is under constant overload, first thickens, then becomes fatigued, weakens and finally becomes unable to perform its pumping function. This leads to fluid accumulation in the lungs and legs, severe shortness of breath and extreme fatigue. In addition, life-threatening risks such as stroke or sudden cardiac death during exertion are part of the natural course of this disease. It is therefore vital to recognize this as an emergency and seek treatment immediately when symptoms appear.
How does heart valve calcification go away or can its progression be slowed down?
One of the questions patients are most curious about is whether there is a medicine that can stop or reverse this calcification. the most honest answer to the question “What is good for heart valve calcification?” is this: Unfortunately, scientific studies to date have clearly demonstrated that once valve arthritis has started, there is no drug treatment that can stop or reverse the process.
It was hoped that treatments such as cholesterol-lowering drugs (statins) and blood pressure medications might slow this process, but extensive research has not confirmed this expectation. Although medications cannot treat arthritis itself, they are used to improve patient comfort and manage complications before definitive treatment (surgery or TAVI). For example, we use medicines to control high blood pressure, reduce fluid retention due to heart failure (diuretics) and regulate arrhythmias.
So, is there nothing we can do in this process? Of course there is. Although it cannot directly stop arthritis, adopting healthy lifestyle habits protects our overall cardiovascular health by controlling underlying risk factors, potentially slowing the rate of disease progression and making us better prepared for possible treatment.
Here are steps you can take to protect your heart health:
- Heart-healthy nutrition
- Regular physical activity
- Quit smoking
- Rigorous control of existing diseases
- Taking care of oral and dental health
It is especially important to avoid saturated fats, processed foods, salt and sugar and to eat fresh fruits, vegetables and whole grains. Smoking is one of the biggest enemies of both arteriosclerosis and valvular calcification and must be quit. It is very important to keep your chronic diseases such as high blood pressure and diabetes under strict control in cooperation with your doctor.
What are the modern treatment options for severe heart valve calcification?
When valve calcification progresses and leads to severe stenosis and the patient develops symptoms, drug treatments are no longer sufficient to solve the problem. At this stage, the problem is mechanical and the solution must also be mechanical. In other words, the only permanent and effective solution is to physically intervene on the damaged valve. This intervention involves repairing the valve or, more often, replacing it with a completely new artificial (prosthetic) valve.
Valve Repair: When possible, the preferred method is for the surgeon to correct the valve structure by preserving the patient’s own valve tissue. However, with a severely calcified, hardened and petrified valve (especially in aortic stenosis), repair is usually not technically feasible and valve replacement becomes the only option.
Valve Replacement: In this procedure, the calcified valve that has completely lost its function is removed and replaced with an artificial valve. There are two main types of artificial valve that can be chosen according to the patient’s age, general health and lifestyle.
Mechanical Covers: Manufactured from highly durable carbon materials. The main features are:
- They are theoretically durable for life.
- They are very unlikely to require reoperation.
- They require lifelong use of blood thinners to prevent the formation of blood clots.
- Regular blood test (INR test) follow-up is mandatory.
Biological (Tissue) Valves: They are made from animal tissues such as bovine or porcine heart membranes that have undergone special processing. The main features are the following:
- They have a very low risk of forming a clot.
- They usually do not require lifelong use of blood thinners.
- They are at risk of wear and re-calcification over time.
- Their average lifespan varies between 10 and 20 years, after which re-intervention may be necessary.
The choice between these two types of valves is made individually by a joint decision of the patient and the heart team, discussing all the advantages and disadvantages.
Should TAVI or open surgery be preferred in the treatment of heart valve calcification?
The biggest revolution in the treatment of severe aortic stenosis in recent years has been the non-surgical method called TAVI (Transcatheter Aortic Valve Implantation). This means that there are now two main treatment options for patients: traditional open heart surgery (SAVR) and TAVI. The decision on which patient is best suited for which treatment is no longer made by a single doctor, but jointly by a “Heart Team” consisting of cardiologists, cardiac surgeons, anesthesiologists and imaging specialists. This approach enables the safest and most effective treatment strategy to be determined for the patient.
Surgical Aortic Valve Replacement (SAVR): In this method, which has been considered the “gold standard” for years, the sternum is cut open and the surgeon, after stopping the heart and connecting the patient to a heart-lung machine, removes the calcified valve and sews a new valve in its place.
Transcatheter Aortic Valve Implantation (TAVI): A procedure performed without opening the rib cage, usually by inserting a thin catheter through an artery in the groin. A new compressed biological valve at the end of this catheter is inserted into the working heart where the old calcareous valve is located and expanded. The new expanding lid pushes the old one to the edges, snaps into place and starts working immediately.
The main factors considered when choosing the treatment method are:
- Patient age and surgical risk
- Appropriateness of the anatomical structure of the valve and vessels
- General health status and comorbidities of the patient
- Life expectancy and lifetime management strategy
As a general rule, TAVI is primarily considered in patients over 75-80 years of age or at high surgical risk, whereas in younger and low-risk patients under 65 years of age, surgery with better long-term outcomes (SAVR) is still a strong option. between the ages of 65-80 is considered the “gray zone” where the decision is personalized according to the patient’s anatomical features, preferences and life expectancy.
How does the recovery process differ after heart valve calcification surgery?
| Recovery Time | 10-15 days . |
| Physical Activity | Light walking is recommended for the first 2-4 weeks, after which a cardiac rehabilitation program is beneficial. |
| Medication Use | Lifelong blood thinners (warfarin) for mechanical valves; short-term for biological valves. Beta blockers and other supportive medications may also be given. |
| Blood Values Monitoring | INR (in patients with mechanical valves) should be checked regularly. |
| Nutrition | A heart-healthy diet that promotes blood pressure and cholesterol control. |
| Infection Prevention | Because of the risk of endocarditis, oral hygiene and protection from infections are of great importance. |
| Before Dental Treatments | Antibiotic prophylaxis may be required; physician should be consulted. |
| Sexual Activity | It is usually possible within 4-6 weeks, depending on physical capacity. |
| Complications | Valve dysfunction, infection (endocarditis), bleeding (especially in warfarin users), arrhythmias. |
| Controls | Frequent echocardiography and cardiology follow-up is required in the first months and annually thereafter. |
| Psychological Status | Anxiety and adaptation may be experienced; support should be sought when necessary. |
| Smoking and Alcohol | Strongly not recommended; it has a negative effect on vascular and heart health. |
| Vehicle Use | after 15 days, if reflexes and attention level are appropriate. |
One of the most important factors determining a patient’s post-treatment experience is the speed and comfort of the recovery process. This is where the most striking difference between TAVI and surgery emerges.
Recovery after TAVI is exceptionally fast due to the minimally invasive nature of the procedure. Since the rib cage is not opened and there is no major surgical trauma, patients recover very quickly. The hospital stay is usually only 1 to 3 days. Patients can walk and eat the day after the procedure and are discharged within a few days and can return to most of their daily activities such as driving and doing light housework in as little as a week.
Recovery after traditional open heart surgery (SAVR) is by nature a longer and more arduous process. Cutting the sternum and stopping the heart is a major intervention. Therefore, intensive care and ward follow-up takes longer. The average hospital stay is 5 to 7 days or more. It usually takes 4 to 12 weeks (1-3 months) for the sternum to completely fuse and for the patient to regain his/her former physical strength and return to work and social life.
Although both treatments improve quality of life in the long term to a similar degree and in an excellent way, the rapid recovery and early comfort offered by TAVI is an invaluable advantage, especially for elderly, frail patients or those who wish to return to a normal life as soon as possible.
What are the considerations when planning the treatment of heart valve calcification in young patients?
One of the most pressing issues for cardiac teams is what is the best way to treat aortic stenosis in a younger patient population, such as those under the age of 65. Treating a young patient is not only about solving the immediate problem, but also about planning to manage their heart health optimally over the next 30-40 years of life. We call this strategic approach “lifetime management”.
Many critical factors are carefully considered when making treatment decisions in young patients:
- Cover durability and need for re-intervention
- Future coronary artery access
- Risk of permanent pacemaker
A biological valve implanted in a young patient (whether surgically or with TAVI) has a lifespan and there is a high probability that the patient will need a second valve intervention later in life. Therefore, the initial procedure must make a possible second intervention in the future (e.g. a new TAVI implanted into a failing valve) technically feasible and safe. In addition, the higher risk of permanent pacemaker implantation after TAVI compared to surgery is an issue that needs to be weighed carefully as it may mean lifelong pacemaker replacement surgeries and pacemaker-related long-term problems in a young patient.
Although the available clinical data show that the 5-year results of TAVI in young and low-risk patients are as successful as surgery, we do not yet have very long-term durability data of 15-20 years. It is therefore essential that the decision to treat young patients is still taken very carefully, individualized and through a “shared decision-making” process in which the patient is thoroughly informed about all these factors.
Frequently Asked Questions
Is Heart Valve Calcification Fatal?
If left untreated in advanced stages, calcification can lead to heart valve stenosis and heart failure, which can be life-threatening. However, early diagnosis and the right treatment can eliminate this risk. When symptoms are noticed, consulting a doctor immediately saves lives.
Is There a Medication Treatment for Heart Valve Calcification?
There is no medicine that completely stops or reverses arthritis. The medication given eases the load on the heart and reduces symptoms. The main treatment is to solve the mechanical problem with the valve: surgical repair or valve replacement. Medication improves your comfort until the operation.
How Should People with Heart Valve Calcification Eat?
A heart-friendly diet is recommended: Reduce salt, avoid processed foods and saturated fats. A Mediterranean-type diet (lots of vegetables, fruit, whole grains, legumes, olive oil and fish) is best for your heart valve and overall vascular health.
What happens as a result of heart valve decay?
Heart valve decay (infective endocarditis) is a serious microbial disease. The valve loses its function, the heart develops severe leaks and heart failure rapidly develops. Clots that break off from the infected tissue can lead to life-threatening complications such as stroke. Early diagnosis and treatment is critical.
Is Heart Valve Decay Surgery Risky?
Of course, infected heart valve surgery is risky, but the real risk is not having surgery. If the infection is not under control, it is life-threatening. With surgery performed by experienced teams, these risks can be minimized and surgery is often life-saving.
Is Herbal Treatment of Heart Valve Decay Possible?
It is absolutely not possible. Heart valve infections can only be treated with strong antibiotics and, if necessary, surgery. Turning to herbal or alternative treatments can be life-threatening. Stick to the treatments offered by modern medicine.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.