Heart spasm, also known as angina pectoris, is a condition caused by sudden narrowing of the coronary arteries. It leads to chest tightness, pain, or discomfort, often mistaken for a heart attack, requiring prompt evaluation to rule out severe cardiac disease.
Symptoms of heart spasm include chest pain radiating to the arm, jaw, or back, shortness of breath, sweating, and palpitations. Attacks may occur during rest, stress, or exertion, and their severity varies depending on the underlying coronary circulation.
Causes of cardiac spasm involve stress, smoking, excessive caffeine, uncontrolled hypertension, or coronary artery disease. Spasms reduce blood flow to the heart muscle, increasing the risk of myocardial infarction if left untreated.
Treatment options include lifestyle modifications, anti-anginal medications, and in severe cases, angioplasty or stenting. Early diagnosis and management are essential to prevent complications and improve overall heart health and quality of life.
| Medical Term | Coronary artery spasm (Prinzmetal’s angina) |
| Key Feature | Chest pain caused by a temporary narrowing of the coronary arteries that supply the heart |
| Symptoms | Feeling of tightness or pressure in the chest, pain radiating to the left arm or jaw, sweating, shortness of breath, palpitations |
| Starting Method | Usually during rest, especially at night or early in the morning |
| Sequence | It usually takes a few minutes |
| Trigger Factors | Cold air, stress, smoking, drug use (especially cocaine), alcohol |
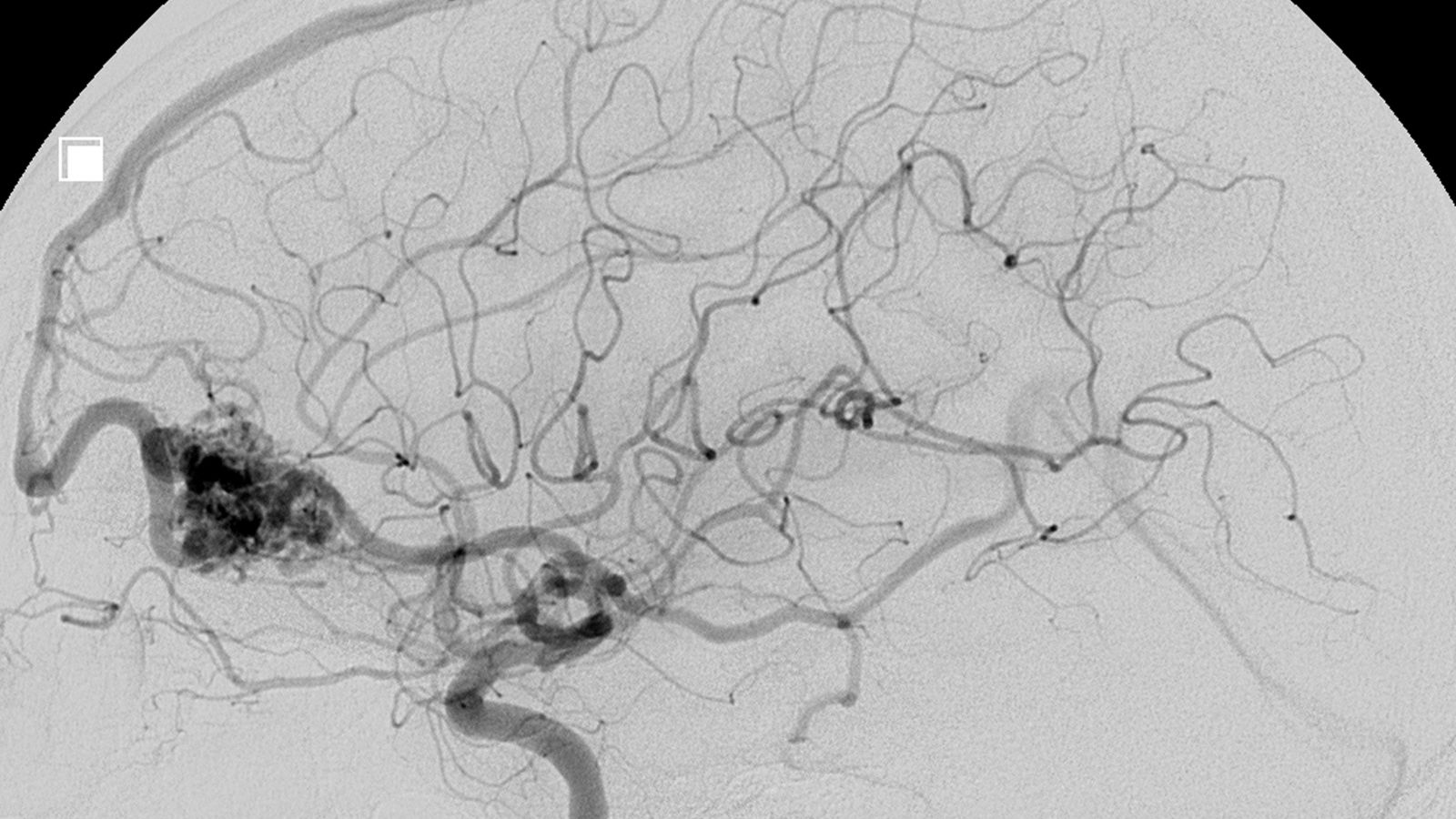
| Diagnostic Methods | ECG, effort test, coronary angiography, Holter monitoring |
| Differential Diagnostics | Stable angina, myocardial infarction, gastroesophageal reflux, anxiety |
| Treatment Methods | Calcium channel blockers, nitrates, lifestyle changes (quitting smoking, reducing stress) |
| Complications | Heart rhythm disorders, myocardial infarction |
| Emergency Symptoms | If the pain is prolonged, does not go away with rest, or if there is shortness of breath or loss of consciousness, urgent intervention is required |
What is Heart Spasm?
In its simplest form, you can think of a heart spasm as a kind of “cramp” in the arteries (coronary arteries) that supply your heart. For some unknown reason, the muscles in the walls of these arteries, which are normally flexible and allow blood to flow freely, suddenly and violently contract. This constriction narrows the vessel so much that the blood flow to the heart is severely reduced, sometimes even stopping completely.
Blood carries the oxygen needed for the heart muscle to work. When this flow is interrupted, the heart muscle is deprived of oxygen. Just as you feel when you hold your breath for a long time, the heart muscle becomes “breathless” and this manifests itself in the typical, pressing chest pain we call angina.
This is the main point that distinguishes heart spasm from classic cardiovascular disease, in which cholesterol plaques gradually clog the vessels. The problem is not a “deposit” that builds up inside the vessel, but rather the momentary malfunctioning of the vessel wall. This is why tests such as coronary angiography can make your blood vessels appear completely open and “squeaky clean”. This is the answer to the question that confuses many patients, “If my blood vessels are open, why do I have this pain?” Heart spasm is a real medical condition that needs to be taken seriously, even if it is not a permanent obstruction in your blood vessels.
What Are Other Medical Names Used for Heart Spasm?
You may hear different names for this condition when you talk to your doctor or read your medical reports. These terms all mean the same thing and can help you understand the condition better. Here are some names you may come across:
- Prinzmetal angina
- Vasospastic angina
- Variant (variant) angina
These names are inspired by the doctor who first described the condition (Dr. Prinzmetal) or the underlying mechanism (vasospastic, i.e. due to vascular spasm). No matter what name is used, they all refer to the picture created by the temporary contraction of the vessels that feed the heart.
What is the Main Difference Between Heart Spasm and Typical Heart Pain (Angina)?
“Heart pain is heart pain”, you may think, but there is a huge difference between them. Knowing this difference is vital for proper diagnosis and treatment. This is the difference between a heart spasm and a heart attack.
This is the case with classic angina, i.e. angina due to atherosclerosis: Your arteries are already narrowed by plaques that build up over time. When you climb stairs, walk fast or get stressed, your heart works faster and needs more oxygen. However, the narrowed blood vessel cannot meet this increased demand and pain occurs. When you rest, your heart slows down, the need for oxygen decreases and the pain goes away. This is why this pain is usually triggered by exertion and is experienced during daylight hours.
What about heart spasm? Heart spasm usually occurs in the opposite scenario:
- It often occurs at rest, or even in the hours between midnight and dawn, waking you from sleep.
- Your heart does not need to work harder for the pain to start; the blood vessel just contracts.
- An angiogram does not show a severe narrowing of the vessels, as in classic angina. Your blood vessels may appear normal.
- Although both pains respond to sublingual nitroglycerin, resting does not relieve the pain, as the spasm pain starts when you are already at rest. The pain goes away either on its own or with medication.
- These fundamental differences play a key role in understanding the cause of your chest pain and in determining the right course of treatment.
How to identify chest pain during a heart spasm?
Patients who experience heart spasms often describe the pain as very severe and uncomfortable. It is not just a simple whimper. What you feel is a sense of pressure or heaviness that is concentrated right in the center of your rib cage. It may feel as if someone is sitting on your chest or as if your chest is being squeezed with a vise. Some patients also describe it as burning, fullness or tightness. The intensity of the pain is usually enough to worry the person and can sometimes be sharp, like a knife stab.
Does Heart Spasm Pain Spread to Other Parts of the Body?
Yes, this is very common and is a typical characteristic of pain of cardiac origin. That feeling of pressure that starts in the chest doesn’t stay in one place, it can spread to other parts of the body. This diffusion is usually felt in these regions:
- Left arm (the most common site of spread)
- Shoulders
- Neck
- Jaw (even the teeth may feel sore)
- Back (especially between the small bones)
- Upper abdominal area (may be confused with stomach pain)
Symptoms of heart spasm can sometimes be different, especially in women. Instead of the typical chest pain, only a sharp pain in the arm, jaw or back may take center stage. It is therefore also important to take seriously any pain that occurs in these areas that cannot be explained by any other cause.
When and How Often Do Heart Spasm Attacks Usually Occur?
One of the most distinctive features of cardiac spasm is the timing and regularity of the attacks. This is one of the most important tips that differentiates it from exertional heart pain.
Timing: Attacks overwhelmingly occur during rest. In particular, the hours between midnight and 8 am are the most common time of day for spasms. Many patients wake up in the middle of the night with a severe chest pain.
Duration: An episode of spasm usually does not last very long. It typically lasts between 5 and 15 minutes and then passes on its own or with medication. Sometimes it can be very short, such as 30 seconds, but rarely it can last for more than 30 minutes.
Frequency: The frequency of attacks varies enormously from person to person. Some people have only one or two attacks a year, while others may experience them several times in one day. Sometimes the attacks are cumulative over several days or weeks, i.e. they recur frequently and then are not seen at all for a long time.
What Are Other Symptoms Associated with Heart Spasm?
During an episode of cardiac spasm, your body may not only signal with chest pain. Deprivation of oxygen to the heart muscle leads to a number of other reactions in the body. Other symptoms that often accompany chest pain include
- Shortness of breath
- Cold sweating
- Nausea (sometimes with vomiting)
- Dizziness or feeling dizzy
- Sudden fatigue and weakness
- Palpitations (feeling that your heart is beating too fast, too strong or irregularly)
- Fainting (syncope)
Fainting is a sign that the spasm has severely reduced blood flow and that the situation can be dangerous.
When to Get Emergency Help When Experiencing Heart Spasm Symptoms?
This is perhaps the most important question. And the answer is very clear: in all cases where you are not sure. It is impossible for you or someone close to you to know at that moment whether the chest pain you are experiencing is a simple spasm or the beginning of a life-threatening heart attack. A severe and prolonged heart spasm can indeed lead to a heart attack or fatal arrhythmia. It is therefore essential not to take risks. The first answer to the question of what to do after a heart spasm is to take the situation seriously.
In the following situations, you should call 112 or go to the nearest emergency room without waiting a second:
- If your chest pain started suddenly and severely.
- The pain lasts for more than a few minutes (e.g. more than 5 minutes).
- The pain does not go away or is not relieved despite resting or taking sublingual medication prescribed by your doctor.
- If your chest pain is accompanied by the symptoms listed above, such as shortness of breath, cold sweats, dizziness or fainting.
Remember that “let me wait a bit and it will pass” is the most dangerous approach in cardiac conditions. Early intervention saves lives.
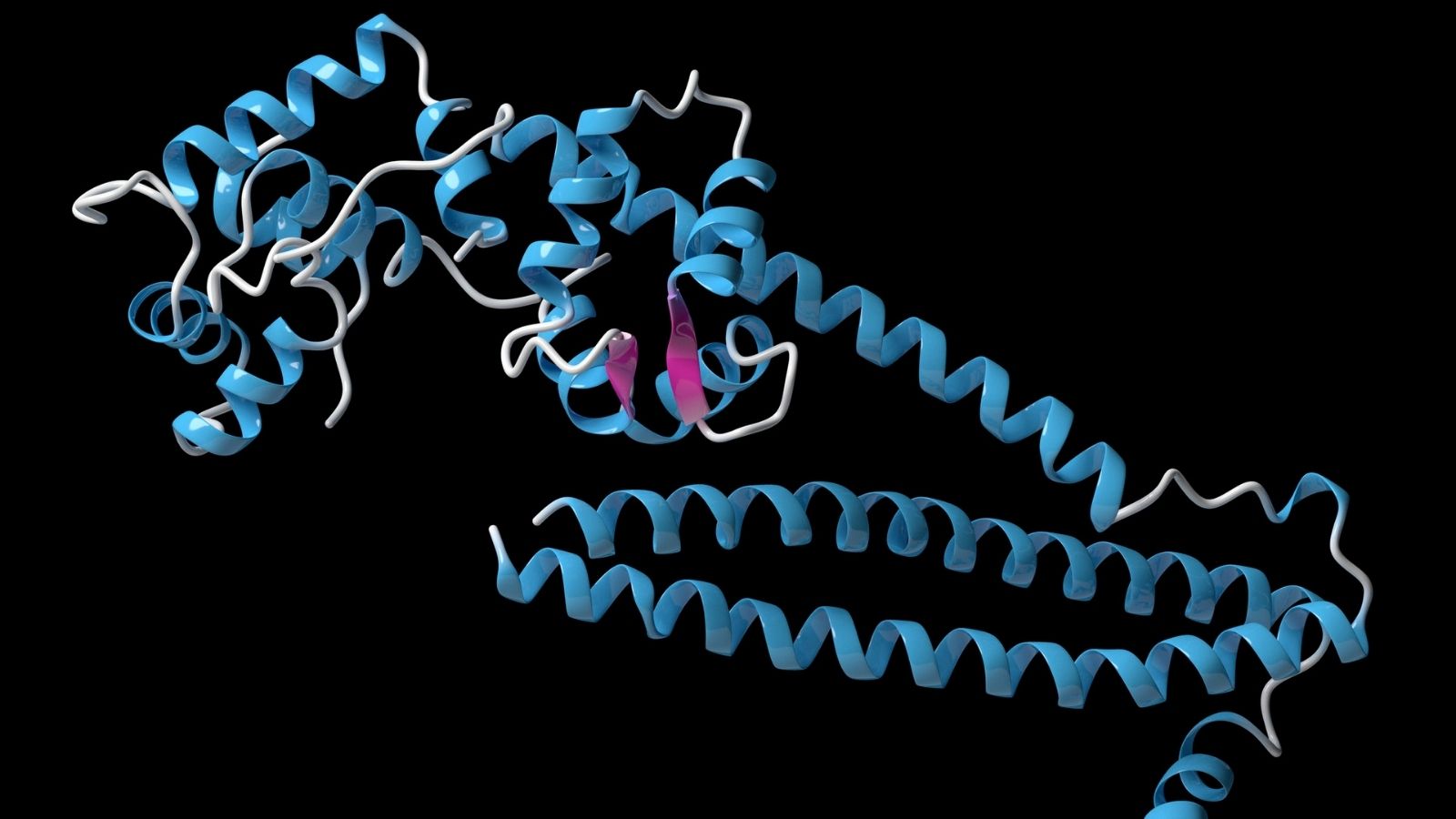
What Is the Basic Mechanism Underlying Heart Spasm?
But why do these vessels contract for no reason? Why does heart spasm happen? The answer to this question is quite complex and does not depend on a single cause. The basic underlying problem is that the vessel itself becomes “overly sensitive” and reactive. There are several main reasons for this sensitivity.
Deterioration of the Inner Surface of the Vessel (Endothelial Dysfunction): Arteries have a very thin layer of cells, called the endothelium, lining the inside of the arteries. This layer secretes chemicals that control when the artery relaxes and when it contracts. A healthy endothelium skillfully relaxes the vessel according to the blood flow. But when its function is disrupted by smoking, stress or inflammation, the balance is upset. In a situation where it should relax, on the contrary, it may contract.
Overreaction of the Vascular Wall Muscles: Smooth muscle cells in the vessel wall become more sensitive than normal. While they normally respond mildly to a mild stimulus, in spasm-prone vessels they respond to even the slightest signal with an extreme and prolonged contraction.
Nervous System Imbalance: Fluctuations in the autonomic nervous system, which manages the involuntary functions of our body, can also trigger spasms. These natural changes in the nervous system, especially at night when the body goes into rest mode, are thought to explain why attacks often occur at night.
What Factors Can Trigger Attacks of Heart Spasm?
Even if your veins are prone to spasm, attacks are often triggered by a specific “trigger”. Knowing these triggers and avoiding them is one of the most important steps in treatment. Here are the most common triggers:
- Tobacco and smoking (the strongest and most common trigger)
- Intense emotional stress (anger, sadness, excessive excitement)
- Exposure to cold air
- Entering cold water (sea, pool) or taking a cold shower
- Illegal stimulants such as cocaine
- Amphetamine-containing substances
- Cannabis use
- Some migraine medications (especially triptans)
- Some nasal sprays or cold sensing medicines containing ephedrine
- Excessive and rapid breathing (hyperventilation)
- Alcohol withdrawal
What are the Known Risk Factors for Heart Spasm?
Unlike classic heart disease, heart spasm can sometimes occur even in people with no known risk factors. This means that you can have a heart spasm even if you do not have high blood pressure or high cholesterol. However, some conditions significantly increase this risk.
Smoking: This is by far the most important of the modifiable risk factors. A very large proportion of patients diagnosed with heart spasms either smoke or have smoked in the past:
- High blood pressure (hypertension)
- High cholesterol
- Insulin resistance or diabetes
Genetic predisposition: Similar family history may increase the risk. The fact that it is more common, especially in the Japanese population, suggests that there may be a genetic background.
Other vascular disorders: People with other spasmodic disorders, such as Raynaud’s phenomenon, which is characterized by cold-induced bruising and blanching of the fingers and toes, or migraine, are at higher risk of heart spasms.
Magnesium deficiency: There are studies suggesting that low levels of magnesium in the body can also increase the tendency to spasm.
Is There a Relationship Between Heart Spasm and Atherosclerosis?
Yes, there is, and this relationship is very important. Cardiac spasm is not a complete blockage of the artery by plaque, but often spasm occurs in areas where atherosclerosis has started or is present, even mildly. So arteriosclerosis is almost a breeding ground for spasm.
Even the earliest stages of plaque formation disrupt the lining of the vessel (endothelium), making it more vulnerable and prone to spasm. Even in vessels that appear “clean” on angiography, more sensitive intravascular imaging methods will often reveal mild plaque or inflammation in the areas of spasm.
This can also turn into a partial cycle. Recurrent severe spasms can damage the vessel wall and accelerate inflammation and plaque formation. Therefore, when planning treatment, not only preventing the spasm but also controlling the underlying atherosclerosis risk factors (blood pressure, cholesterol, smoking, etc.) is very important for long-term vascular health.
What tests are done when a doctor is consulted for suspected heart spasm?
Diagnosing a heart spasm is sometimes like detective work. This is because attacks come and go and by the time you reach the doctor, everything may appear normal. Diagnosis is therefore usually a process of ruling out other possible causes and gathering evidence of the presence of the spasm. The steps followed are usually the following.
- Detailed Conversation and Examination: This is the most important part of the process. Your doctor will ask you in great detail what your pain is like, when it started, how long it lasted, what triggered it and how it makes you feel. The clues you give are the first and most important step in diagnosis.
- Electrocardiogram (ECG): This simple test, which records the electrical activity of your heart, is worth its weight in gold if it can be taken during an attack. However, an ECG taken between attacks is usually completely normal.
- Blood tests: Heart enzymes such as troponin are checked to see if a severe spasm has damaged the heart muscle.
- Echocardiography (ECHO): This is an ultrasound of your heart. It is done to see how well your heart muscle is working, the condition of your valves and if there are any other structural problems.
- Effort Test (Stress Test): This test is usually used to rule out classic exertional angina. Since heart spasm usually occurs at rest, the result of this test may be normal, but it is important in the differential diagnosis.
What is the Role of ECG and Holter in the Diagnosis of Heart Spasm?
ECG and Holter are essential tools that allow us to understand the electrical language of your heart.
- ECG: When the heart muscle is deprived of oxygen during an episode of spasm, this leads to very typical changes in the ECG recording. In particular, what we call “ST segment elevation” is very characteristic for spasm. The problem is that this change is only visible at the moment of the spasm and once the spasm is over, the ECG returns completely to normal. It is not always possible to catch this moment.
- Holter Monitoring: This is where the Holter comes in. This is a small ECG device that you carry in your body for 24 or 48 hours, sometimes even longer. It records continuously while you go about your normal life. If you have an attack during this time (whether painful or quiet), the Holter captures the moment and provides your doctor with evidence of the spasm. However, if your attacks are infrequent, you may not have an attack on the day you wear the Holter and the result may still be normal.
Why Coronary Angiography is Important in the Diagnosis of Heart Spasm?
Coronary angiography is a turning point in the diagnosis of heart spasm. It is a procedure in which a thin tube (catheter) is inserted through the groin or arm and a dye is injected into the heart vessels and a film is taken. It serves two main purposes.
- Excluding Serious Vascular Blockages: The first and most basic goal of angiography is to make sure that the cause of your chest pain is not due to a persistent and severe stenosis in your blood vessels. If the angiography shows that your blood vessels are open and you have typical pains that occur at rest, the suspicion of heart spasm is very strong.
- Preparing the Groundwork to Prove Spasm: Angiography is where the provocation (trigger) test is done to confirm the suspicion. Without this test, a definitive diagnosis is often not possible.
How is Provocation Testing Performed in the Diagnosis of Heart Spasm?
If, despite all tests, the cause of your pain is unclear and heart spasm is strongly suspected, a “provocation test” is performed to confirm the diagnosis. This test is the “gold standard”, the most reliable method of diagnosing heart spasm.
This test is done during the angiography procedure, in a controlled and safe environment. With the angiography catheter inside your heart vessel, a special drug such as acetylcholine is slowly and in very low doses given into the vessel. This drug is designed to temporarily contract the vessel, which is prone to spasm. During this time, three things are observed at the same time.
- Symptoms of the patient: It is questioned whether the patient has the onset of the typical chest pain.
- ECG Changes: The ECG is monitored for the appearance of the typical electrical changes (ST elevation) that indicate spasm.
- Angiographic Image: The screen shows live whether the vein in which the drug is administered is actually contracting (constricting above).
If these three findings come together, the diagnosis of heart spasm is definitive. Although the test sounds scary, in experienced hands it is extremely safe. As soon as the spasm is triggered, it is completely relaxed within seconds with nitroglycerin administered intravenously. This test is not performed in all centers as it requires special expertise and shows why the diagnosis of this condition should be carried out by a specialist.
What to Use for Emergency Treatment During a Heart Spasm Attack?
When an attack of spasm begins, the immediate goal is one: to relax the contracted vessel as quickly as possible, restore blood flow to normal and relieve the pain. The most effective weapon for this is short-acting nitrates. So what is good for heart spasm?
Nitroglycerin: These medicines are available as a sublingual tablet or spray. When placed under the tongue or sprayed during an attack, it quickly enters the bloodstream, dilates blood vessels and relieves spasm within seconds. It is vital that every patient diagnosed with heart spasm carries this medicine with them at all times.
Which Long-Term Drugs Are Prescribed to Prevent Heart Spasm?
The emergency medicine stops the attack, but the main goal is to ensure that these attacks never happen. Heart spasm treatment is based on this preventive approach. Two groups of medicines form the basis of treatment.
- Calcium Channel Blockers: These drugs are the mainstay of heart spasm treatment. Muscle cells in the vessel wall need calcium to contract. By blocking the entry of calcium into the muscle cells, these drugs keep the vessels more relaxed and reduce the risk of spasms. Drugs such as diltiazem, amlodipine, nifedipine are in this group. They are usually recommended to be taken in high doses at bedtime and at night, when spasms are common.
- Long Acting Nitrates: They are added to treatment when calcium channel blockers are inadequate. They stay in the body longer, helping to keep blood vessels loose throughout the day.
In addition to these medicines, statins (cholesterol medicines) may be used to improve the health of the inner surface of the arteries, especially in patients with atherosclerosis, or other special medicines in treatment-resistant cases.
Why Some Drugs (e.g. Beta Blockers) Should Be Avoided in the Treatment of Heart Spasm?
This is a vital point. Beta blockers (such as beloc, concor, saneloc) are very common and very useful drugs in the treatment of high blood pressure, heart failure and classic angina. However, in the case of heart spasm, they can worsen the condition, especially the non-selective types. This is because these drugs can block some of the signals that relax the vessels, while causing the effect of the signals that contract the vessels to become more suppressive. This increases the tendency to spasm. This is why it can be dangerous to randomly prescribe a heart medication to a patient with chest pain without a proper diagnosis.
What is the Role of Lifestyle Changes in Heart Spasm Management?
As important as medicines are, your lifestyle changes are just as important, if not more important. Drugs suppress symptoms, while lifestyle changes help you get to the root of the problem.
- Quit Smoking Immediately: If you smoke, this is the most important and effective thing you can do.
- Avoiding Triggers: If you know what triggers your spasms (stress, cold, certain medications), you should consciously avoid them.
- Learning to Manage Stress: Stress management techniques such as meditation, yoga, regular exercise or hobbies can reduce the frequency of attacks.
- Avoiding Cold: Simple measures such as wearing layers of clothing, scarves and beanies can be very helpful during the winter months.
- Paying Attention to Nutrition: A diet rich in fresh vegetables, fruits, whole grains and healthy fats, such as the Mediterranean diet, improves your overall vascular health.
- Avoiding Stimulants: Substances such as cocaine, amphetamines should never be used. Caution should also be exercised with energy drinks and some unprescribed supplements.
Are Interventional Methods (Stents) or Devices Necessary in the Treatment of Heart Spasm?
Because heart spasm is a dysfunction, it is not usually treated with interventional methods such as stents or surgery.
- Stenting: Because the problem is not a permanent stenosis in one part of the vessel, but a general tendency of the vessel to spasm, stenting in one spot is usually not the solution. The spasm may recur right next to the stent or in a completely different vessel. Only in very rare cases, a stent may be considered if it is proven that the spasm always occurs over a slight stenosis in the same spot.
- ICD (Implantable Shock Device): This is more of a safety measure than a treatment. If it is proven that a dangerous life-threatening arrhythmia (ventricular tachycardia/fibrillation) has occurred during an episode of heart spasm, it may be necessary to implant an ICD (implantable cardioverter-defibrillator) to prevent life-threatening arrhythmia in a similar future situation. This device saves lives by detecting the dangerous rhythm and shocking the heart.
- Pacemaker: In very rare cases, when the spasm causes the heart to slow down too much (bradycardia) or stop, a pacemaker may need to be implanted to support the heart’s work.
Frequently Asked Questions About Heart Spasm
What is heart spasm?
Cardiac spasm is a temporary chest pain or feeling of tightness caused by a sudden narrowing of the coronary vessels that supply the heart. It usually lasts a few minutes and leaves no permanent damage to the heart muscle.
What is the difference between a heart spasm and a heart attack?
A heart attack is a complete blockage of a blood vessel, resulting in damage to heart tissue. A heart spasm is a temporary narrowing and usually leaves no permanent damage. However, frequent recurrent spasms may increase the risk.
What are the symptoms of heart spasm?
Symptoms may include chest tightness, a feeling of pressure, pain radiating to the left arm, shortness of breath, sweating and palpitations.
What causes heart spasm?
Stress, excessive smoking, cold air, arteriosclerosis and some medicines can cause heart spasms.
Is heart spasm dangerous?
Yes, over time it can lead to a heart attack or disrupt the heart rhythm. Especially recurrent spasms should be taken seriously.
How is heart spasm diagnosed?
Diagnosis can be made with ECG, exercise test, angiography and blood tests. ECG changes may be observed at the time of spasm.
Does a heart spasm go away on its own?
In some cases it may be temporary, but if it recurs frequently, it is essential to consult a specialist.
What to do if someone has a heart spasm?
The person should be sedated, provided with fresh air and, if necessary, given a sublingual pill. If complaints persist, 112 emergency should be called.
At what age do heart spasms occur?
Although it is more common in people over 40, it can also occur in young people with risk factors.
Does stress cause heart spasm?
Yes, intense stress and emotional trauma can lead to temporary narrowing of the blood vessels.
How to feel heart spasm in women?
Women sometimes experience atypical symptoms such as fatigue, nausea, back or jaw pain instead of the classic chest pain.
What medications are used to treat heart spasm?
Vasodilators and rhythm-regulating drugs such as nitrates, beta-blockers, calcium channel blockers are commonly used.
What should a person with heart spasms pay attention to?
They should quit smoking and stress, eat a healthy diet, exercise regularly and do not neglect their doctor’s visits.
Which doctor to go to for heart spasm?
It is best to consult a cardiologist about this.
Can heart spasm be completely cured?
With appropriate lifestyle changes and regular medication, heart spasm can be largely controlled and attacks can be prevented. Early diagnosis saves lives!

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.