Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid in tissues, leading to swelling, most commonly in the arms or legs. It arises from impaired lymphatic drainage due to surgery, radiation, or infection.
Symptoms include persistent swelling, heaviness, skin tightness, and recurrent infections. In advanced cases, fibrosis and skin changes occur, significantly impacting mobility and quality of life.
Conservative management consists of compression therapy, manual lymphatic drainage, exercise, and meticulous skin care. These measures aim to control swelling and prevent progression rather than provide a complete cure.
In severe cases, surgical options such as lymphatic bypass or lymph node transfer may be considered. Early diagnosis and multidisciplinary treatment improve outcomes and reduce the risk of complications.
| Medical Term | Lymphedema |
| Definition | Tissue swelling caused by fluid accumulation in the interstitial space as a result of disruption of the lymphatic system |
| Classification | Primary (congenital or genetic) – Secondary (after surgery, radiotherapy, infection) |
| Most Common Regions | Arm, leg, face, genital area |
| Main Causes | Lymph node dissection after breast cancer, pelvic cancer surgeries, radiotherapy, filariasis (in tropical regions) |
| Symptoms | Swelling (especially in the extremities), feeling of heaviness, tension, limitation of movement, thickening of the skin |
| Staging | Stage 0: No clinical signs – Stage 1: Swelling, reduced in the morning – Stage 2: Persistent swelling, no subsidence – Stage 3: Fibrosis, skin changes (elephantiasis) |
| Diagnostic Methods | Physical examination, lymphoscintigraphy, ultrasonography, MR lymphography |
| Treatment Methods | Complex decongestive therapy (manual lymph drainage, bandaging, exercise), compression garments, skin care, rarely surgery (lymphovenous anastomosis) |
| Complications | Infection (lymphangitis), limitation of movement, cosmetic problems |
| Prevention Methods | Skin hygiene, appropriate exercise, protection of the extremity from trauma, regular application of compression therapy |
What is lymphedema and how does it affect the body?
Let’s imagine our body as a complex and constantly working city. Our arteries are the pipelines that carry clean water to this city, and our veins are the main sewage system that takes back most of the used water. The lymphatic system is one of the most critical infrastructures of this city: the city’s sanitation, waste collection and recycling network. It is made up of thin vessels that collect “garbage” that the veins cannot carry, such as large protein molecules, waste materials, fats and bacteria, from between tissues. This collected fluid is filtered and cleaned in purification plants called “lymph nodes” and then re-enters the main bloodstream.
Lymphedema occurs when there is a malfunction in this “cleaning and recycling” system. When lymph vessels are damaged, blocked or congenitally deficient, this protein-rich fluid begins to accumulate in the tissues. This build-up leads to chronic swelling, lymphedema, which we usually see in the arms or legs, but can also occur in other parts of the body.
Why should lymphedema not be seen as just a simple swelling?
The main difference between swelling after an ankle sprain and lymphedema is the content of the accumulated fluid. Temporary swelling is usually water-dominated and easily absorbed by the body. In lymphedema, the accumulated fluid is “protein-rich”. These large protein molecules that accumulate in the tissues act like a sponge, drawing more water from their surroundings and causing the swelling to be persistent and progressive.
More importantly, the body perceives this accumulated protein as a threat and initiates an ongoing, low-level inflammatory reaction in the area. Over time, this chronic inflammation destroys the structure of the tissue. The initially soft tissue gradually hardens (fibrosis) and the number and volume of fat cells in the area increases. Therefore, while lymphedema is initially a “fluid” problem, if left untreated, it turns into a permanent “solid tissue” problem over time. This progressive nature explains why early diagnosis and proper treatment are so vital.
Is every lymphedema the same and what are the main types?
Lymphedema is divided into two main groups according to the underlying cause. This distinction is crucial for understanding risk factors and the treatment plan.
- Primary Lymphedema: This type is caused by a congenital structural defect of the lymphatic system. Due to a genetic inheritance or a developmental problem in the womb, the lymph vessels or nodes are either underdeveloped, underdeveloped or dysfunctional. Primary lymphedema is rarer and is subdivided according to the age of onset.
- Secondary Lymphedema: This is the most common type of lymphedema. It occurs when a previously completely healthy lymphatic system is damaged by a subsequent event. This damage can have many causes.
What are the most common risk factors for secondary lymphedema?
The main conditions and risk factors that can disrupt a healthy lymphatic system and lead to secondary lymphedema include
- Removal of lymph nodes during cancer surgery
- Receiving radiotherapy (radiation therapy)
- The tumor itself presses on the lymph pathways
- Recurrent skin infections (especially cellulitis)
- Major accidents, crush injuries or severe burns
- Vein diseases such as chronic venous insufficiency or deep vein thrombosis (DVT)
- Obesity (overweight)
- Prolonged immobility due to illness or injury
- Usually, instead of a single cause, a combination of multiple risk factors significantly increases the likelihood of developing lymphedema.
What are the most common symptoms of lymphedema?
The first signs of lymphedema are usually subjective symptoms felt by the patient, rather than visible swelling. It is very important to be alert to these early signs, especially if you have a known risk factor (for example, if you have been treated for breast cancer). The signs of lymphedema in the arm or lymphedema in the leg are similar. The most common symptoms of lymphedema are:
- Swelling in the affected arm or leg
- Feeling of heaviness or fullness
- Skin tightness
- Squeezing of items such as rings, watches or shoes
- Difficulty of movement in the joints
- Hardening or thickening of the skin
- Pain or discomfort
- Recurrent episodes of infection with redness, increased heat and pain (cellulitis)
Reviews of lymphedema patients confirm that the first thing they usually notice is this feeling of “heaviness and tightness” rather than swelling.
How does a doctor diagnose lymphedema?
In the vast majority of cases, the diagnosis of lymphedema can be made after a thorough evaluation by an experienced physician. This process consists of two basic steps. The first is to have a detailed interview with you and listen to your medical history and complaints. Topics such as your risk factors, when and how your complaints started, and your family history form the basis of this interview.
The second step is a careful physical examination. During this examination, the physician tries to exclude other possible causes of the swelling (such as heart failure, venous insufficiency, kidney disease) and looks for signs specific to lymphedema. In the early stages, a dimple (gode) is typical when the swollen area is pressed with a finger. In advanced cases, an important finding called “Stemmer’s sign” is looked for. When we try to pinch the skin on the second toe of the hand or foot, the inability to fold and lift the skin due to its thickening and adhesion to the underlying tissue indicates that this symptom is positive and greatly supports the diagnosis of lymphedema.
What further tests are used to diagnose lymphedema?
Although most of the time clinical evaluation is sufficient, sometimes further diagnostic procedures may be necessary to confirm the diagnosis, to objectively determine the severity of the disease or to plan a surgical treatment.
- Lymphoscintigraphy A test that provides a functional map of the lymphatic system. It clearly shows slowing or obstruction in lymph flow.
- Indocyanine Green (ICG) Lymphography: It is a mapping method that we use especially when planning modern lymphedema surgery, showing the working superficial lymph vessels in real time.
- Magnetic Resonance (MRI) or Computed Tomography (CT): It is used to exclude another structural problem (tumor, cyst, etc.) that may cause swelling and to get information about the structure of the tissue (ratio of fluid, fat, hard tissue).
- Bioimpedance Spectroscopy (BIS): It is a sensitive measurement method that can detect the smallest fluid increases in the tissue even before visible swelling occurs and is used in the follow-up of patients at risk.
What are the stages of lymphedema?
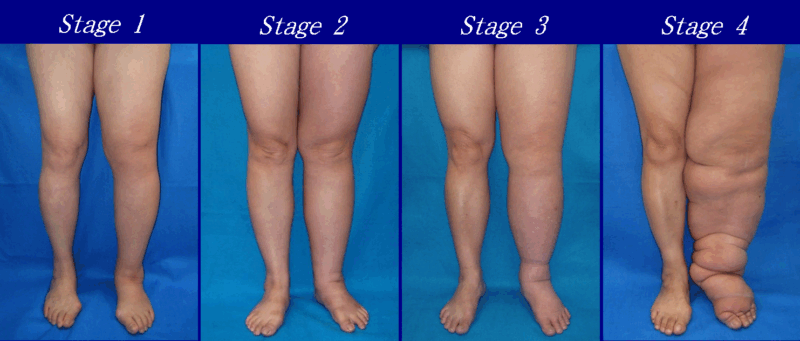
The International Society of Lymphology (ISL) staging system is used to define the severity of lymphedema in a standardized way. This system provides a roadmap for determining the treatment strategy.
- Stage 0 (Subclinical Stage): Lymph transport capacity is reduced but there is no swelling yet.
- Stage 1 (Reversible Stage): Swelling is present, soft and remains hollow when pressed with a finger. The swelling goes down when the limb is lifted up.
- Stage 2 (Non-Reversible Stage): The swelling is permanent and the tissue has started to harden. It does not go down completely by raising the limb.
- Stage 3 (Lymphostatic Elephantiasis): This is the most advanced stage. The swelling is very severe, the skin has undergone irreversible changes such as thickening and hardening.
What is Complex Decongestive Therapy (CDT), the cornerstone of lymphedema treatment?
Complex Decongestive Therapy (CDT) is the globally recognized “gold standard” for the non-surgical treatment of lymphedema. It is not just a massage or bandaging technique, but a comprehensive treatment program consisting of four complementary components. The aim is not only to reduce swelling but also to maintain the achieved result and give the patient the ability to manage their own condition. CBT is administered by certified lymphedema therapists with specialized training in this field and requires the patient’s active participation in the treatment. Treatment is usually conducted in two phases: an intensive initial phase aimed at reducing swelling and a lifelong maintenance phase aimed at maintaining the result.
The four main components of CBT are:
- Manual Lymph Drainage (MLD)
- Compression Therapy (Bandages and Compression Garments)
- Therapeutic Exercises
- Skin and Nail Care
How does Manual Lymph Drainage (MLD) work in the treatment of lymphedema?
Manual Lymph Drainage (MLD) is completely different from the classic massage we know. It is a technique consisting of very light, rhythmic, slow and special movements aimed at gently stretching the skin. The aim is to stimulate the superficial lymph vessels directly under the skin, not the muscles. The therapist “hijacks” the accumulated lymph fluid from the blocked area and directs it towards healthy and working lymph areas of the body. This is almost like a traffic diversion process. MLD is therefore applied not only to the swollen area but also to healthy areas where the fluid will drain.
Why does compression therapy play such a critical role in the management of lymphedema?
Compression, the application of external pressure, is perhaps the most important component of CBT. Its effect is much more profound than simply squeezing the limb. This controlled pressure applied from the outside reduces fluid leakage into the tissues, increases the reabsorption of existing fluid back into the lymph vessels and, most importantly, strengthens the “pump” effect of the muscles. Short-stretch bandages, used especially in the treatment phase, act as a hard wall when the muscle contracts, allowing the fluid to be pumped upwards much more strongly. In the maintenance phase of treatment, compression garments (cuffs, socks, etc.) are used, which are specially prepared according to the patient’s measurements. Wearing these garments regularly, usually during the daytime, ensures the success of the treatment and the permanence of the result.
Why is skin and nail care vital for people with lymphedema?
A limb with lymphedema is an area with a weakened immune system. The accumulated protein-rich fluid creates the perfect environment for bacteria to breed. Therefore, maintaining the integrity of the skin and preventing even the smallest injury is the fourth and vital component of CBT. The aim is not to create a gateway for infection.
Here are the basic skin care rules:
- Cleansing the skin daily with a pH-balanced, gentle soap
- Drying the skin completely after cleansing
- Using a low pH moisturizer to prevent skin cracking
- Protection from cuts, scratches and insect bites
- Wearing protective gloves when working in the garden or kitchen
- Cutting nails straight and never cutting cuticles
- Immediately clean even the smallest wound with soapy water and apply antiseptic
In which cases should surgical treatment for lymphedema be considered?
the most modern answers to the question “How to relieve lymphedema?” lie in surgical treatment options. Although surgery is not suitable for all patients, it is a promising option, especially for patients who do not respond adequately to conservative treatments such as CBT or who want to stop the progression of the disease more effectively. The decision for surgery depends on many factors, including the patient’s general health, the stage of lymphedema, the nature of the swelling (whether it is liquid or solid) and the patient’s expectations. A cardiovascular surgeon’s expertise in microsurgery and supermicrosurgery plays a key role in the success of these surgeries.
Lymphedema surgeries basically serve two main purposes:
- Physiologic Surgery: Aims to repair or bypass impaired lymph circulation.
- Reductive Surgery: It aims to remove the accumulated solid tissue (fat and fibrosis).
How is lymphedema treated with Lymphaticovenous Anastomosis (LVA) surgery?
LVA is one of the most delicate and technically challenging surgical procedures available today. The basic logic of this surgery is to create a new “bypass” pathway for blocked lymphways. We connect the functioning superficial lymph vessels to the very small veins (venules) right next to them. In this way, the lymph fluid that accumulates in the tissues bypasses the blocked system, enters the bloodstream directly and is removed from the body. This procedure is a “supermicrosurgery” technique performed under a very high magnification operating microscope using special instruments and sutures thinner than a hair. It is a minimally invasive and effective method for the treatment of lymphedema, especially in the arm. LVA gives the best results in the early stages of the disease, when the swelling is still predominantly fluid.
How does Vascularized Lymph Node Transfer (VLNT) offer a solution for the treatment of lymphedema?
VLNT is a more extensive reconstruction surgery, especially for patients whose lymph nodes have been completely damaged by cancer surgery or radiotherapy. The aim of this surgery is to bring new and working “lymph stations” to the area with lymphedema. Lymph nodes from a healthy part of the body (for example, the groin or abdomen), along with the blood vessels that supply them, are microsurgically transplanted to the lymphedematous area. These new lymph nodes create a new drainage center in the area, both absorbing fluid like a “sponge” and triggering the formation of new lymph pathways. A successful VLNT can lead to a reduction in swelling as well as a marked decrease in the frequency of cellulite attacks, especially recurrent ones.
What kind of treatment is liposuction for advanced lymphedema?
In the advanced stages of the disease, the main component of the swelling is no longer fluid but solidified fat and fibrotic tissue that has accumulated as a result of chronic inflammation. This solid volume cannot be eliminated by CBT or physiological surgeries. This is where the liposuction technique specially adapted for lymphedema comes into play. The aim of this procedure is not to solve the underlying lymphatic problem, but to physically remove the solid volume that occurs as a result of this problem. This dramatically reduces the size and weight of the limb, improving function and appearance. However, the success of this surgery and the permanence of the result depends on one thing: that the patient wears compression garments of the appropriate pressure 24 hours a day, without interruption, for life after surgery. This is a treatment partnership and the patient needs to be ready for this commitment.
What serious problems can untreated lymphedema cause?
Lymphedema is a disease that should be taken seriously and can lead to serious complications if left untreated:
- Recurrent and severe cellulitis infections
- Risk of infection entering the bloodstream (sepsis)
- Progressive hardening and thickening of tissues (fibrosis)
- Distortion of limb shape (elephantiasis)
- Severe limitation of joint movements
- Chronic pain
- Continuous leakage of fluid from the skin (lymphorrhea)
- Psychological problems such as anxiety and depression
- Very rarely, cancer development on the background of long-term lymphedema (Lymphangiosarcoma)
Is there a place for methods such as ‘turmeric’ or ‘cupping’ in the management of lymphedema?
It is natural for patients to research all kinds of treatment methods. However, it is critical to know the scientific facts on popular topics such as turmeric effects on lymphedema or lymphedema treatment with cupping. Some herbal products such as turmeric may have general anti-inflammatory properties, but there is no scientific evidence that they can treat lymphedema. Such supplements are never a substitute for evidence-based medical treatments. Practices that disrupt the integrity of the skin, such as cupping, are extremely dangerous for lymphedematous tissue. It can further damage the already sensitive skin and damaged lymph vessels, creating a gateway for serious infections. Therefore, such practices should be strictly avoided.
Why is nutrition and weight management important for lymphedema patients?
Lifestyle habits directly affect the success of treatment. In particular, weight management and nutrition play a critical role in reducing the burden on the lymphatic system. Excess weight is both a risk factor for lymphedema and significantly worsens the existing condition. Achieving and maintaining a healthy weight is one of the most important supporters of treatment. While there is no magic diet that “cures” lymphedema, there are some nutritional principles that help manage symptoms:
- Reducing salt (sodium) intake
- Consuming sufficient and balanced protein
- Focus on unprocessed, whole foods
- Drink plenty of water
- Limit alcohol and caffeine consumption
What precautions should be taken in daily life when living with lymphedema?
Living with lymphedema requires constant awareness to protect the affected limb from potential dangers. These measures help to minimize the risk of complications:
- Always use the healthy limb for blood collection, injections, etc.
- Always have blood pressure measured on the healthy arm.
- Avoid hot baths, spas and saunas.
- Do not wear tight clothing, clothes with tight cuffs or jewelry.
- Keep the affected limb above heart level when resting or sleeping.
- Always wear compression garments at the appropriate pressure during air travel.
Frequently Asked Questions
What is lymphedema?
Lymphedema is swelling, usually in the arms or legs, caused by the accumulation of lymph fluid in the body. It is caused by blockage or damage to the lymphatic system.
What are the symptoms of lymphedema?
Swelling, tension, a feeling of fullness, limitation of movement, stiffness and skin changes can be seen in the arm or leg.
What causes lymphedema?
Removal of lymph nodes after surgery, radiotherapy, infections or congenital lymph vessel disorders can lead to lymphedema.
Is lymphedema a sign of cancer?
No, but cancer treatments (especially after breast cancer) can increase the risk of lymphedema.
In which stages is lymphedema classified?
It is usually assessed in 4 stages: latent stage, reversible stage, persistent stage and fibrosis (hardened) stage.
Is lymphedema contagious?
No, lymphedema is not transmitted from person to person. It is related to the immune system and lymph flow.
How is lymphedema diagnosed?
Physical examination, patient history, measurements, lymphoscintigraphy and sometimes imaging such as MRI or ultrasound are used.
Can lymphedema be cured?
Although not completely cured, the swelling can be reduced and its progression stopped with appropriate treatment.
What treatments are available for lymphedema?
Manual lymph drainage, compression bandages/socks, exercise, skin care and, if necessary, pneumatic compression devices are used.
Is there medication for lymphedema?
There is no direct drug treatment for lymphedema. However, antibiotics may be needed if there is a risk of infection.
Does lymphedema go away with exercise?
Exercise alone is not a cure, but it can help reduce edema by increasing circulation. Low-intensity, controlled exercises are recommended.
How long does lymphedema take to develop?
In some cases it can occur immediately after surgery, but sometimes it can develop months or years later.
How does lymphedema change the skin?
Over time, the skin can thicken, harden and become susceptible to infection (for example: cellulite).
Should lymphedema be massaged?
Yes, but this should be manual lymph drainage with specialized techniques; unconscious massage can cause harm.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.