Pericarditis is the inflammation of the pericardium, the thin sac surrounding the heart. It can cause sharp chest pain, which often worsens with breathing or lying down, and may lead to complications such as pericardial effusion or constrictive pericarditis if untreated.
The causes of pericarditis include viral infections, autoimmune diseases, heart surgery, trauma, and certain medications. Identifying the underlying cause is essential for determining the appropriate treatment and preventing recurrence.
Clinical findings typically include pericardial friction rub, characteristic ECG changes, and imaging evidence of pericardial thickening or fluid accumulation. Echocardiography is the most useful diagnostic tool for detecting complications such as cardiac tamponade.
Treatment usually involves anti-inflammatory medications such as NSAIDs or colchicine. Severe or recurrent cases may require corticosteroids or surgical procedures. Timely medical intervention is vital to avoid long-term complications and preserve cardiac function.
| Types | Acute Pericarditis, Subacute Pericarditis, Chronic Pericarditis, Constrictive Pericarditis, Effusive Pericarditis |
| Causes | Viral infections (most common), bacterial infections, autoimmune diseases, post-myocardial infarction (Dressler syndrome), trauma, uremia, radiotherapy |
| Risk Factors | History of infection, connective tissue diseases (lupus, rheumatoid arthritis), renal failure, previous heart surgery |
| Symptoms | Chest pain (especially worse when lying on your back and worse when leaning forward), shortness of breath, fever, weakness, palpitations |
| Diagnostic Methods | ECG (diffuse ST elevation), echocardiography (presence of effusion), chest X-ray, CT/MR, blood tests (CRP, sediment, troponin) |
| Treatment Options | NSAIDs (ibuprofen, aspirin), colchicine, corticosteroids (in rare cases), antibiotics (in bacterial causes), pericardiocentesis (if effusion is present) |
| Complications | Pericardial effusion, cardiac tamponade, chronic pericarditis, constrictive pericarditis, recurrent pericarditis |
| Protective Measures | Prevention of viral infections, treatment of underlying diseases, regular cardiologic follow-up |
What is pericarditis?
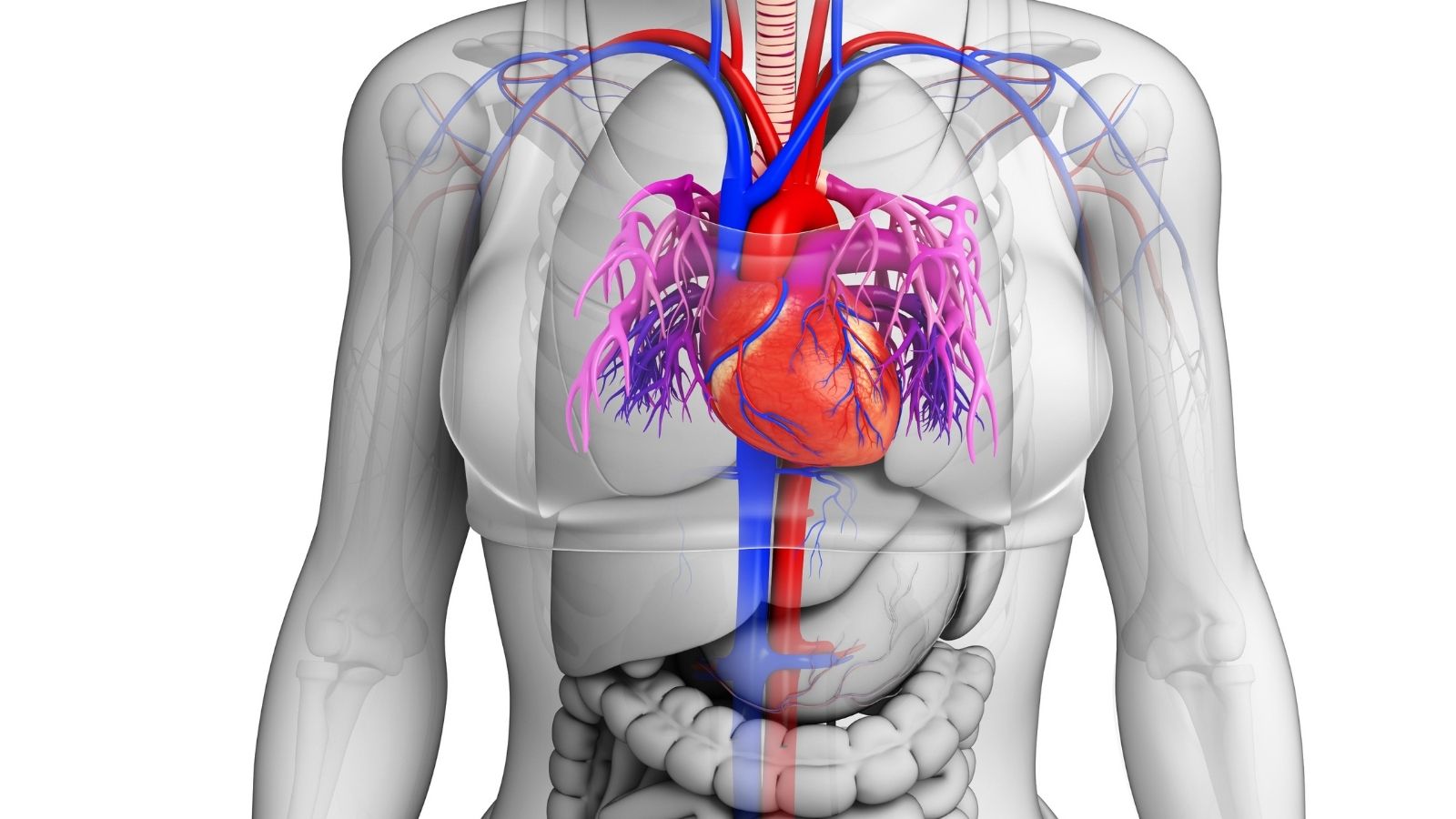
Imagine a double-layered membrane that surrounds our heart like a protective cradle inside the rib cage. This membrane is called the pericardium. Its role is very important: It holds the heart in place, prevents it from overfilling with blood and stretching and, most importantly, acts as a shield against infections from neighboring organs such as the lungs. Between this double layer of membrane is a lubricating fluid, normally a teaspoon or two. Thanks to this fluid, the heart can move freely and frictionlessly inside this sheath with each beat.
Pericarditis begins with inflammation of this protective sheath. Just as any part of the body swells, reddens and becomes tender when it becomes inflamed, the pericardium reacts in the same way. The layers of the inflamed membrane thicken, become rough and begin to rub against each other. This friction is the root cause of the famous sharp pain of pericarditis.
Moreover, the inflammatory process triggers the production of fluid between the membrane layers. This fluid, which is normally very little, can increase abnormally with inflammation. We call this a “pericardial effusion”, which is colloquially known as a build-up of fluid around the heart or a blister in the heart. If this fluid builds up too much or increases too quickly, it can put severe pressure on the heart. The heart cannot relax and fill with blood because of the pressure of the fluid surrounding it. This can lead to “cardiac tamponade”, which requires emergency intervention and can be life-threatening. In short, pericarditis is a health problem that can turn the protective armor of our heart into a source of pain and pressure.
What are the symptoms of pericarditis?
Pericarditis often presents with symptoms that are too obvious to ignore. Knowing these signs can enable you to seek medical help in a timely manner. The most common symptoms of pericarditis are:
- Sharp and stabbing chest pain
- Shortness of breath
- Weakness and fatigue
- Dry cough
- Light fever
- Palpitations
- Swelling in the legs (in advanced cases)
- Difficulty swallowing
Among these symptoms, chest pain is almost the identity of pericarditis. Although it is often confused with heart attack pain, pericarditis pain has its own distinctive features. The pain is usually felt behind the breastbone or in the left chest. The most typical feature is that it changes with position. If you lie on your back, breathe deeply or cough, the pain stabs like a knife and intensifies. In contrast, if you take a sitting position and lean forward slightly, you will notice that the pain is significantly reduced. This is due to the reduced pressure on the heart and the friction of the inflamed membranes against each other. This positional feature is one of the most important clues that distinguish pericarditis from other causes of chest pain.
Which conditions can cause pericarditis?
The answer to the question of what causes water retention in the heart or what triggers pericarditis is quite broad. Sometimes, despite all the research, no clear cause can be found and this is called “idiopathic pericarditis”. But there is usually an underlying cause. The main causes that can lead to pericarditis:
Viral Infections
- Influenza (Influenza)
- Common cold viruses (Adenovirus, Echovirus)
- Epstein-Barr virus (EBV)
- COVID-19
Bacterial Infections
- Tuberculosis (Tuberculosis)
- Staphylococcal and Streptococcal infections
Autoimmune Diseases
- Rheumatoid arthritis
- Systemic lupus erythematosus (Lupus)
- Scleroderma
Conditions Affecting the Heart and Chest Area
- Previous heart attack
- Open heart surgery
- Blows to the chest (trauma)
- Radiation therapy to the chest area
Other Reasons
- Advanced renal failure (uremia)
- Spread of cancers to the heart (Metastasis)
- Side effects of some medicines
- Thyroid gland diseases
As you can see, many conditions can predispose to pericarditis, from a simple flu infection to a serious systemic illness. Therefore, when pericarditis is diagnosed, it is very important not only to treat the inflammation, but also to find the underlying cause that triggered it.
What steps are taken to diagnose pericarditis?
When you present with suspected pericarditis, a series of assessments are carried out to reach a diagnosis. This process starts with a detailed interview with you. It is very important for us to find out when and how your pain started, its character, whether it changes with position, and whether you have had a recent infection. Then the physical examination begins. A squeaking-like sound known as a “pericardial friction sound”, which can be heard when listening to your heart with a stethoscope, is a valuable diagnostic clue.
After this initial assessment, we move on to diagnostic tests. These are the main methods we use to confirm the diagnosis and understand the severity of the condition:
- Electrocardiogram (ECG)
- Echocardiogram (ECHO – Heart Ultrasound)
- Blood tests
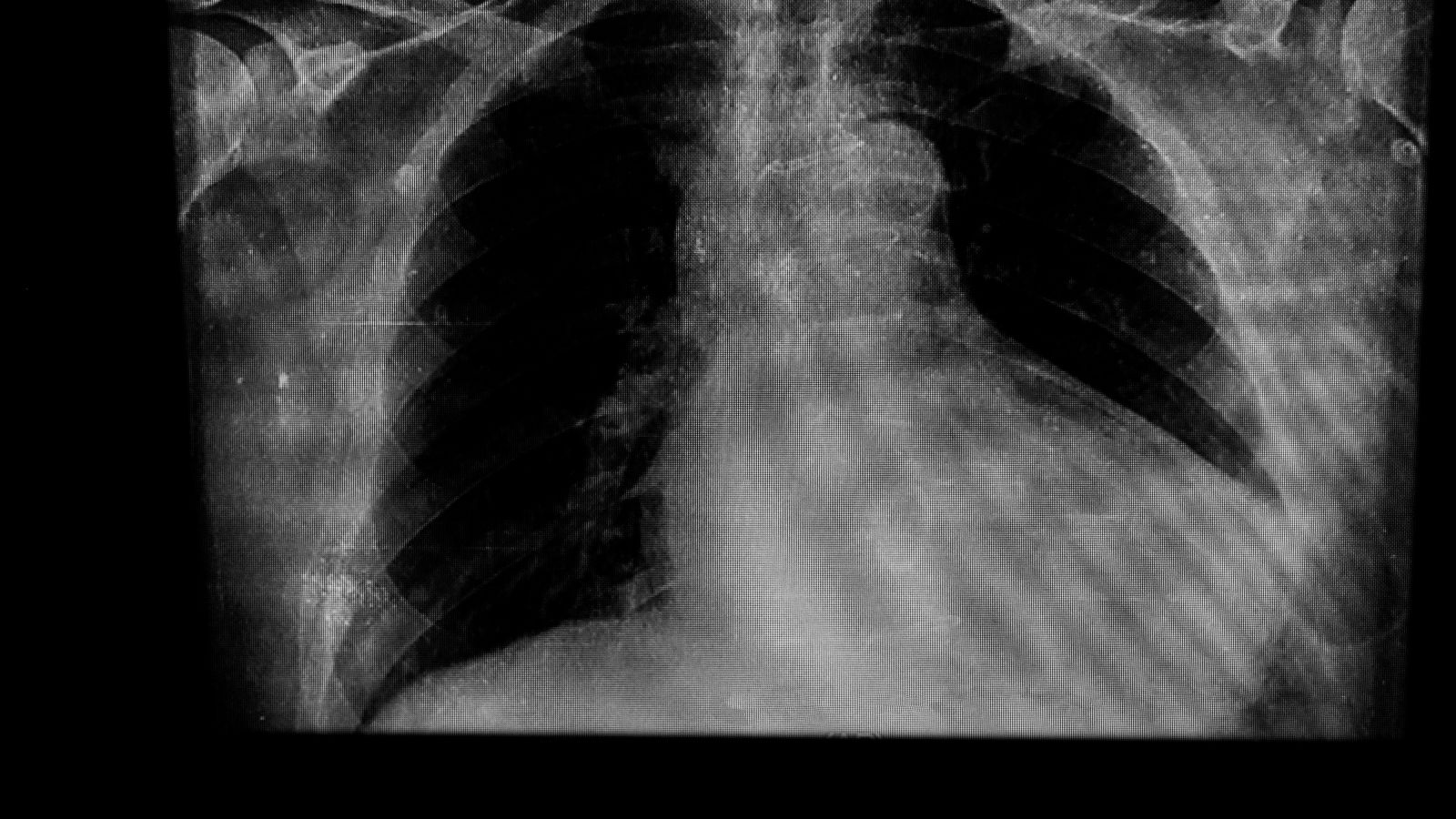
- Chest X-ray
- Cardiac MRI or Computed Tomography (CT)
The ECG measures the electrical activity of the heart and shows typical changes characteristic of pericarditis. An echocardiogram is perhaps one of the most important tests; it allows us to see clearly whether there is fluid accumulation in the pericardium, the amount if any, and whether this fluid is pressing on the heart. Blood tests measure the level of inflammation in the body (CRP, sedimentation) and detect damage to the heart muscle (troponin). Advanced imaging modalities such as chest X-ray and especially Cardiac MRI allow us to examine the structure of the pericardium in detail when the diagnosis is uncertain or when we suspect complications such as constrictive pericarditis.
How is pericarditis treatment planned?
The treatment of pericarditis requires an individualized roadmap. Our main goals in treatment are very clear:
- Eliminate pain and inflammation
- Prevent recurrence (relapse) of the disease
- If there is an underlying cause, treat it
- Prevent the development of serious complications such as cardiac tamponade or constrictive pericarditis
The treatment modalities we use to achieve these goals are usually medication and, when necessary, interventional interventions. Medication for fluid accumulation in the heart is usually the first step. We often use a combination of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and a drug called colchicine to control inflammation and pain. Colchicine is a key cornerstone of treatment, especially as it significantly reduces the risk of disease recurrence.
If there is no response to this treatment, or if the underlying cause is a different condition, such as a rheumatic disease, stronger inflammation-suppressing drugs such as corticosteroids (cortisone) may be considered. Newer, targeted therapies, such as biological agents that directly target the inflammatory cycle, may also be on the agenda, especially in cases that are resistant to standard treatments, recurrent and severely impair the patient’s quality of life.
If the accumulation of fluid around the heart reaches a level that puts pressure on the heart, then interventional procedures are inevitable. with a procedure called “pericardiocentesis”, we relieve the heart by draining this excess fluid with the help of a needle under ultrasound guidance. If the fluid accumulation is recurrent, a small surgical procedure called “pericardial window” can be used to ensure continuous drainage of the fluid. The last and largest surgical intervention is “pericardiectomy”. This surgery is performed to surgically remove this hardened membrane to free the heart, especially in the case of “constrictive pericarditis”, where the pericardial membrane thickens and squeezes the heart like a suit of armor.
Which pericarditis symptoms signal an emergency?
While pericarditis is a condition that can usually be managed at home with medication and rest, some symptoms may indicate a danger that requires immediate medical attention. It is vital to know these alarm symptoms. If you experience any of the following situations, you should contact the nearest emergency room immediately:
- Intolerable, severe chest pain
- Excessive difficulty in breathing, breathlessness
- Dizziness or fainting
- Cold and damp skin
- Intense anxiety and panic
- Blurred consciousness
- Marked swelling of the neck veins
These symptoms can often indicate a life-threatening condition known as cardiac tamponade, in which fluid around the heart compresses it and prevents it from pumping blood. This is a true medical emergency where minutes count.
Is pericarditis a dangerous disease?
This is the most natural and most important question in the mind of every patient who receives this diagnosis. I can state this clearly: Pericarditis is a disease that, in the vast majority of cases, can be completely cured and managed with the right approach. Patients who have acute pericarditis, especially for the first time, usually return to their normal lives without permanent damage with proper treatment and rest.
So, does pericarditis kill or is a collection of fluid in the heart fatal? The answer to these questions depends on whether the disease develops complications. Pericarditis can become dangerous because of its two main complications.
The first is Cardiac Tamponade, which we mentioned above. This is an acute and urgent condition. You can think of it as the fluid around the heart suffocating the heart. Without timely intervention, yes, it can be fatal. However, the symptoms are often noisy and a timely pericardiocentesis (fluid drainage) procedure can eliminate this risk.
The second is Constrictive Pericarditis, which is more insidious and develops over time. In this condition, the pericardium loses its elasticity and turns into a thick, hard shell, restricting the heart’s movements. This leads to chronic heart failure and severely reduces quality of life. The only permanent solution is a major surgical intervention called pericardiectomy.
After all, it is not the pericarditis itself that is dangerous, but its potential complications. Therefore, our task is not only to treat the existing inflammation, but also to protect you from these dangerous complications. These risks can be minimized through early diagnosis, full compliance with treatment and regular medical check-ups.
How does life go on after pericarditis?
Being diagnosed with pericarditis can be alarming, but the good news is that the overwhelming majority of patients make a full recovery. Once the treatment process is complete and your doctor has given the go-ahead, you can return to your normal life. However, there are some important points you should pay attention to during and after the recovery period.
Here are some suggestions for managing the healing process in a healthy way.
Rest: It is very important to give your body time to heal, especially in the acute phase.
Avoid Physical Activity: You should avoid strenuous exercise and competitive sports until the inflammation has completely subsided and your blood values, such as CRP, have returned to normal. This period can usually be at least 3 months.
Taking Medication Regularly: It is critical that you take the medication prescribed by your doctor regularly for the recommended duration, even if your symptoms go away, to prevent the disease from recurring.
Do not skip check-ups: You should definitely go to your follow-up appointments after treatment. These check-ups are done to make sure that the disease is completely gone and to detect a possible relapse early.
Healthy Lifestyle: General health rules such as a balanced diet, adequate sleep and avoiding stress will strengthen your immune system and contribute to your recovery.
Pericarditis is a condition that can be overcome if managed correctly. The important thing is to listen to your body’s signals, consult a specialist physician and be patient during the treatment process. Remember you are not alone on this path.
Frequently Asked Questions
What is pericarditis?
Pericarditis is an inflammation of the pericardium, the membrane that surrounds the heart. It is usually manifested by chest pain.
What causes pericarditis?
The most common cause is viral infections. It can also be caused by bacteria, autoimmune diseases, the period after a heart attack and certain medications.
Is pericarditis contagious?
Pericarditis is not directly contagious. However, if the cause is a viral infection, the virus may be contagious.
What are the symptoms?
Chest pain, pain in the back and shoulders, stinging sensation when breathing, fever, weakness and sometimes palpitations may occur.
How to distinguish pericarditis from a heart attack?
Both can cause chest pain, but pericarditis pain usually decreases with sitting and increases with lying down. ECG and imaging methods are used for diagnosis.
How is pericarditis diagnosed?
It is diagnosed by ECG, echocardiography, chest X-ray, blood tests and sometimes MRI.
Is pericarditis a dangerous disease?
Mild cases usually improve with treatment. However, if fluid accumulates, it can compress the heart and threaten life (cardiac tamponade).
What are the treatment methods?
Anti-inflammatory drugs, colchicine and, if necessary, antibiotics or cortisone therapy. Surgical intervention is rarely required.
Is pericarditis permanent?
Most of the time it is temporary. However, in some cases it can recur or become chronic.
What about chest pain in pericarditis?
It is usually stinging, sharp and increases with deep breathing or lying down.
Does pericarditis require rest?
Yes, physical activity should be restricted and rest should be taken, especially in acute periods.
Does pericarditis recur?
Yes, pericarditis may recur in some patients. This may require long-term medication.
Does pericarditis prevent sports?
It should be strictly avoided in the acute period. After recovery, activities can be resumed under the supervision of a doctor.
What happens if fluid accumulates in pericarditis?
If too much fluid accumulates in the pericardial cavity, the heart can be compressed, which requires emergency intervention (cardiac tamponade).

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.