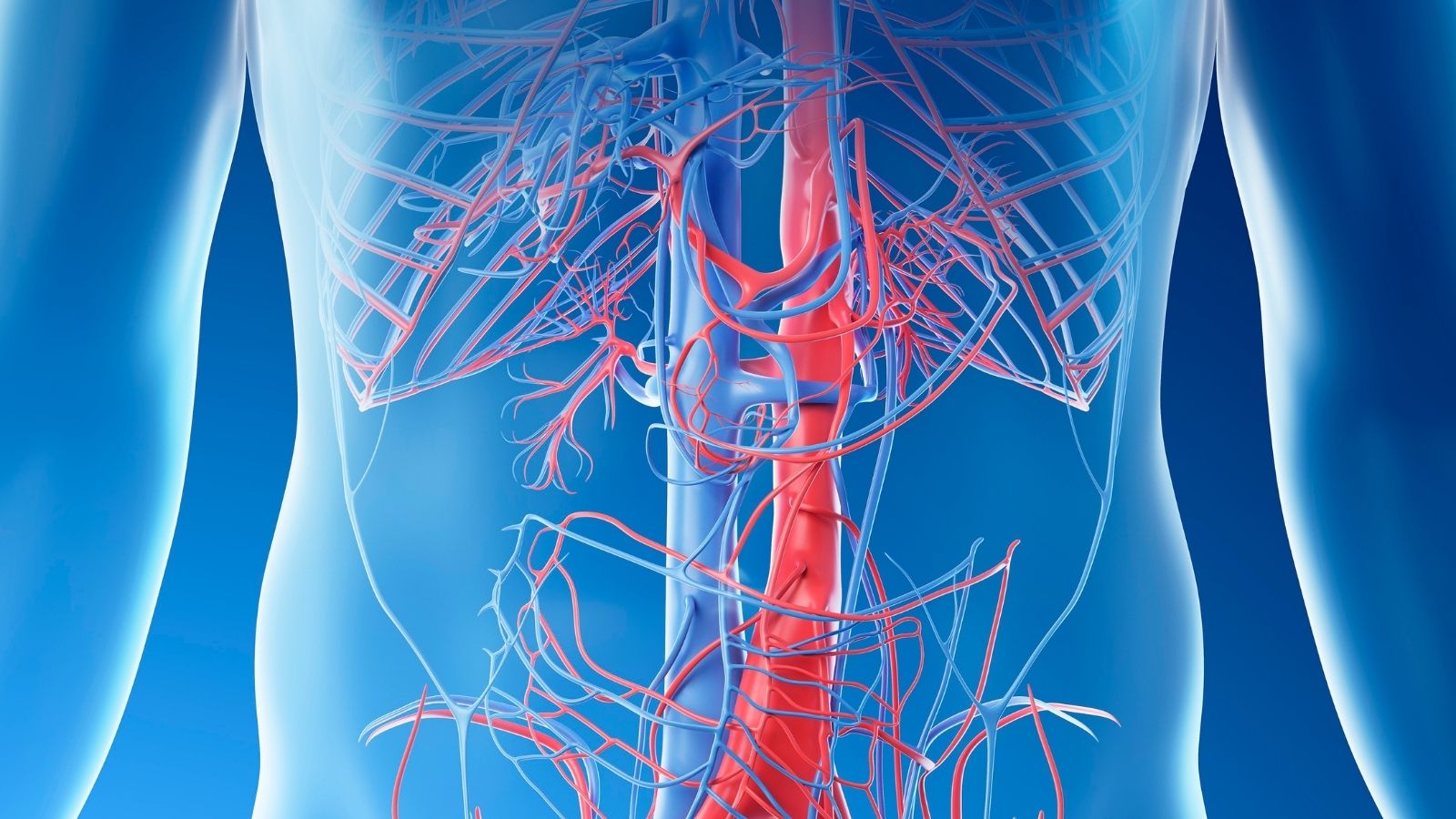
CT angiography, also known as virtual angiography, is a non-invasive imaging technique that visualizes blood vessels using computed tomography and contrast agents. It provides detailed insights into vascular anatomy and pathologies without requiring conventional catheter angiography.
Clinical applications of virtual angiography include evaluation of coronary artery disease, detection of aneurysms, and assessment of peripheral arterial circulation. It allows physicians to diagnose vascular conditions with high precision and minimal procedural risk.
The procedure involves intravenous administration of iodinated contrast followed by rapid CT scanning. Advanced software reconstructs three-dimensional vascular images, enabling accurate visualization of stenosis, occlusions, or malformations.
Advantages of CT angiography include reduced patient discomfort, faster recovery, and lower complication rates compared to invasive angiography. However, it requires careful consideration in patients with renal impairment or contrast allergies.
| Medical Name | Computed Tomography Angiography (CT Angiography, Virtual Angiography, Coronary CT Angiography) |
| Frequent Use Areas | – Suspicion of coronary artery disease – Evaluation of vessel blockages, narrowing and aneurysms |
| Causes | – Suspicion of cardiovascular disease such as chest pain, shortness of breath – Failure to obtain sufficient information with other diagnostic methods |
| Risk Factors | – Allergy to contrast media – Impaired renal function – Pregnancy (due to radiation) – Rapid heartbeat or arrhythmia |
| Complications | – Allergic reaction due to contrast media- Impaired renal function- Radiation exposure |
| Diagnostic Methods | – Clinical examination – Blood tests (kidney function, thyroid, etc.) – ECG and other cardiologic tests for preliminary evaluation |
| Treatment Methods | – Virtual angiography is a diagnostic method, not used for treatment |
| Prevention Methods | – Evaluation of allergy and renal function before the use of contrast media- Avoidance of unnecessary radiation |
What is Virtual Angiography?
Virtual angiography is not actually the name of a single device or procedure. It is an umbrella term that encompasses two key high-tech imaging modalities: Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA). Both have the same goal: to see the inside and walls of the blood vessels in detail. But the technologies they use to do this are completely different.
There is a big difference between taking a photograph of a building from the outside and creating a three-dimensional model of the building, showing the architectural plan, the plumbing inside the walls and the layout of the rooms. Virtual angiography creates this three-dimensional and detailed model of your blood vessels.
Computed Tomography Angiography (CTA): This is an advanced, vascular-specific version of what is commonly known as “tomography”. This procedure uses a very fast, high-resolution tomography machine. The key point of the procedure is the introduction of an iodine-based “contrast agent”, a dyed drug, through a vein in your arm, just like an IV drip. As this drug mixes with your blood and fills all your veins, the CT scanner takes hundreds of cross-sectional images in a matter of seconds. These images are like pieces of a puzzle. Powerful computer software puts them together to create an incredibly clear, three-dimensional map of your vascular network, especially the coronary arteries that supply the heart. With this map, we can see the slightest calcification, stenosis or plaque in the vessel wall.
Magnetic Resonance Angiography (MRA): This method uses a strong magnetic field and radio waves instead of X-rays. In other words, it is a customized version of the “MRI” device for imaging blood vessels. The biggest advantage of MRA is that it contains no radiation. This makes it a valuable option, especially for younger patients, patients requiring frequent follow-up or patients who need to avoid radiation. MRA can sometimes be performed with a “gadolinium”-based contrast agent to make the vessels more prominent, and sometimes without any drug at all. It is generally preferred for imaging of large vessels such as the aorta, leg or neck arteries.
What is the Virtual Angioplasty Experience?
One of the things our patients are most curious about is what they will experience during the procedure. Contrary to its name, virtual angioplasty is a very simple and comfortable process. We can summarize the process step by step from the moment you arrive at your appointment:
When you arrive at the center, you will first be briefly informed about the procedure and your consent form will be taken. If you are wearing any metal objects (jewelry, watches, belts, etc.), you will be asked to remove them. You will then be taken to the shooting room.
Here, you lie on your back on the table of the CT or MRI machine. If you are having a CTA, ECG electrodes will be attached to your chest to monitor your heart rhythm. This is a completely painless procedure. The nurse will then start a vein with a thin plastic needle (intravenous catheter), usually in a vein in the elbow area of your arm. This is no different from a standard blood transfusion or IV drip.
If your heart vessels are to be examined (coronary CTA), this is where the most critical part of the procedure – heart rate control – comes into play. We can get the clearest image of your heart when it is moving the least, that is, during the short pause between two beats. It’s like when you take a photograph and the subject remains still. For this reason, your heart rate should be regular and below 65 beats per minute. If your heart rate is high, you may be given a small dose of medication through your vein to slow it down. You will also be sprayed under the tongue just before the scan with a spray that slightly dilates the coronary arteries, making the image even clearer.
When all preparations are complete, the table of the device slowly moves into the annular part of the device (gantry). It is not a completely closed tunnel, it is quite spacious. During the shot, the operator will ask you to give a simple command through the microphone, such as “Breathe… Hold it!” through the microphone. In the short period of 5-10 seconds that you hold your breath, the dye is administered through your vein and the whole scan is completed. A momentary feeling of warmth in your body or a metallic taste in your mouth when the dyed substance is administered is normal and temporary.
As soon as the extraction is finished, you can get up from the table, get dressed and resume your daily life after your intravenous line is removed. There is no rest, hospitalization or special follow-up.
What to Consider Before Virtual Angioplasty?
For the quality and safety of the procedure, there are some simple but important preparations that you should pay attention to, especially before Coronary CTA. These preparations ensure the most accurate result.
Basic preparations to be made before the procedure:
- fasting for 4 to 6 hours (water can be drunk)
- Stop caffeine consumption from 12 hours before the procedure
- Coffee
- Tea
- Kola
- Chocolate
- Energy drinks
- Informing your physician about your medications (especially diabetes medications)
- Share your history of allergies to iodinated medicines or seafood, if any
- Wearing comfortable clothes on the day of the procedure
Who is a Good Candidate for Virtual Angioplasty?
Virtual angiography is a highly effective method for both diagnosing and excluding cardiovascular disease in a wide range of patients with suspected cardiovascular disease. Virtual angiography (CTA) is particularly useful in the following cases.
Some patient profiles and conditions that are suitable for this method:
- People with complaints such as chest pain but at low or moderate risk of heart disease
- Those with suspicious or indeterminate results on exertion or thallium testing
- Patients who have had bypass surgery before and whose complaints recur
- Patients with recurrence of symptoms after stent implantation and appropriate stent diameter
- Preoperative control of patients scheduled for a non-coronary heart surgery such as a heart valve
- Suspected congenital structural defects (anomalies) of the coronary arteries
- People with a family history of premature heart disease and in the risk group
Are There Any Situations In Which Virtual Angiography Is Not Feasible Or Recommended?
Although virtual angiography is a very safe procedure, it may not be suitable for all patients. There are some conditions that may prevent the procedure from being performed or may reduce the quality of the results.
Situations where the procedure is not generally recommended or requires special precautions:
- Proven history of severe (anaphylactic) allergy to iodinated contrast media
- Severe renal failure
- Severe heart rhythm disorders that cannot be controlled (e.g. atrial fibrillation with rapid ventricular response)
- Pregnancy (for BTA)
- General condition impairment to the extent that he/she cannot obey breath-holding commands
- Uncontrolled hyperthyroidism (risk of thyroid storm)
- Excessive and widespread vascular calcification (may impair image quality)
- Presence of MR incompatible metal implants in the body (for MRA)
What are the Advantages of Virtual Angiography over Classic Angiography?
Virtual angiography has many revolutionary advantages over traditional, catheterized angiography. These advantages have made it the first choice diagnostic modality in appropriate patients.
The main difference is in the nature of the procedure. Conventional angiography is an invasive procedure with a thin tube (catheter) that is inserted through the artery in the groin or wrist and then extended to the heart. Virtual angiography does not require such an intervention. This fundamental difference brings with it many advantages.
Here are the most obvious advantages of virtual angiography:
Non-Interventional: Since it does not enter the vein, it does not carry serious risks such as catheter-related bleeding, vessel rupture or stroke.
Painless: There is no pain or discomfort other than the simple opening of a vein.
Fast Speed: The shooting process takes seconds, the whole process takes 15-20 minutes.
Comfortable: There are no obligations such as hospitalization after the procedure, waiting on the back for hours with a sandbag. The person can immediately return to their social life.
More Comprehensive Information: While conventional angiography only shows the space inside the vessel (lumen), virtual angiography also shows the vessel wall. This provides information about the structure, quantity and danger potential of the plaques, which are the main source of the disease.
Detecting High Risk Plaques: It can detect soft plaques that are prone to rupture, which can cause a heart attack.
An Excellent Screening Test: If your virtual angiogram result is “clean”, there is almost zero chance that there is a significant problem with your blood vessels. This saves you unnecessary intervention and worry.
Is Virtual Angioplasty Risky?
As with any medical procedure, virtual angiography has potential risks, but these risks are much lower and manageable compared to conventional angiography. Risks need to be differentiated according to the technique used.
Risks of Computed Tomography Angiography (CTA): There are two main risks associated with this method. The first is radiation. Since CTA uses X-rays, the patient receives some radiation. However, there is no need to worry about this. Thanks to the dose reduction technologies used in today’s modern devices, the radiation dose received from a coronary CTA procedure has been reduced to levels close to the amount of natural radiation we receive from the environment in a year in daily life. This dose is often even lower than other nuclear medicine tests, such as a thallium test (heart scintigraphy).
The second risk is related to the iodinated contrast medium used. In people with normal kidney function, this substance is perfectly safe to use and is easily excreted through the kidneys. However, some side effects may rarely occur.
Possible contrast media reactions:
- Itching
- Skin rash (hives)
- Nausea
- Feeling of warmth in the body
These reactions are usually mild and temporary. Serious life-threatening allergic reactions are extremely rare and all medical equipment is available at the extraction centers for emergencies. If you have a known kidney disease, the use of this medicine will be carefully evaluated by your doctor.
Magnetic Resonance Angiography (MRA) Risks: There is no radiation risk with MRA. The most important issue is the presence of MR-incompatible implants in the body, such as pacemakers, metal prostheses or clips. These conditions can be a definite obstacle for MRA. Allergic reactions to gadolinium used in contrast-enhanced MRA are even rarer than to iodinated agents.
Can Virtual Angiography Open a Blockage in My Veins?
No, it is not. Virtual angiography is a diagnostic and diagnostic method, not a treatment method.
Its task is to provide a clear picture of the current state of your veins, to determine if there are any problems. If there is a blockage or stenosis, it shows us its location, degree and structure. However, it does not have the ability to open, dilate or stent this blockage.
These treatment procedures (balloon angioplasty and stenting) are interventions that can only be performed during conventional, interventional angiography. Virtual angiography is a roadmap that allows us to decide whether this intervention is needed. If the virtual angiogram reveals a critical stenosis that requires treatment, the patient is then referred to conventional angiography for a balloon/stent procedure. Therefore, virtual angiography provides the most reliable answer to the question “is there a need to open the vessel?” rather than the answer to the question “does it open the vessel?”.
How a Cardiac Surgeon Uses Virtual Angiography in Surgery Planning
For a cardiovascular surgeon, virtual angiography is a three-dimensional navigation system that allows us to master the patient’s anatomy before entering the operating room. It provides us with invaluable information, especially in the planning of complex heart surgeries, directly improving the safety and success of the operation.
Previous Bypass Patients (Re-operation): The most risky stage for a patient undergoing bypass surgery for the second or third time is reopening the breastbone. Because the bypass vessels from the first operation or the heart itself may be stuck just behind the bone. A virtual angiogram performed before surgery shows us the location of these vital structures and their relationship with the breastbone in three dimensions. Based on this map, we plan where to safely use the saw and where to avoid. This is a vital step that minimizes the risk of fatal bleeding during surgery.
Valve Surgery and TAVI Planning: Today, aortic valve replacement (TAVI) through the groin is based entirely on measurements obtained by virtual angiography. Planning a TAVI procedure without virtual angiography is unthinkable.
For TAVI, we have critical data from virtual angiography:
- Millimetric measurements of the patient’s own valve ring to determine the exact size of the valve to be implanted
- The exit height of the coronary arteries to prevent the new valve from blocking the mouth of the heart vessels
- Diameter and appropriateness of the vasculature from the groin to the heart (aorta and leg arteries)
- The amount and distribution of scale in the valves
- X-ray angle to get the most accurate image during the procedure
We also want to know if there are any problems in the coronary arteries of a patient undergoing a major operation such as valve surgery. Virtual angiography allows us to check this without putting the patient at risk of catheter angiography. If there is a stenosis, we perform the valve surgery and the bypass procedure in the same session.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.