Cyanosis is the bluish discoloration of the skin and mucous membranes caused by insufficient oxygen in the blood. It may be localized or generalized, depending on whether the underlying problem is respiratory, cardiac, or circulatory in nature.
Central cyanosis often indicates serious cardiopulmonary disease such as congenital heart defects, severe lung conditions, or circulatory failure. It usually presents with bluish lips, tongue, and mucosa, requiring urgent evaluation.
Peripheral cyanosis is frequently associated with reduced blood flow in extremities, commonly due to cold exposure, arterial obstruction, or circulatory insufficiency. It primarily affects the fingers, toes, or nose without mucosal involvement.
Treatment focuses on addressing the root cause, such as improving oxygenation, correcting circulatory problems, or surgical interventions in congenital heart disease. Prompt management prevents complications related to chronic oxygen deprivation.
| Medical Name | Cyanosis |
| Common Symptoms | – Bruising of the lips, fingertips, nails or skin – Feeling cold – Fatigue – Shortness of breath (may be accompanied) |
| Causes | – Decreased oxygenation – Congenital heart disease – Lung diseases (COPD, pneumonia, embolism) – Heart failure – Vascular occlusions |
| Risk Factors | – Chronic heart or lung disease- Smoking- History of congenital heart disease- Old age |
| Complications | – Oxygen deficiency in organs – Loss of consciousness – Respiratory or circulatory failure |
| Diagnostic Methods | – Physical examination- Oxygen saturation measurement- Blood gas analysis- Lung radiography- Echocardiography |
| Treatment Methods | – Treatment of the underlying cause – Oxygen support – Medication or surgery if necessary |
| Prevention Methods | – Regular treatment of chronic diseases – Smoking cessation – Regular medical follow-up |
Why does our body turn blue and why does cyanosis occur?
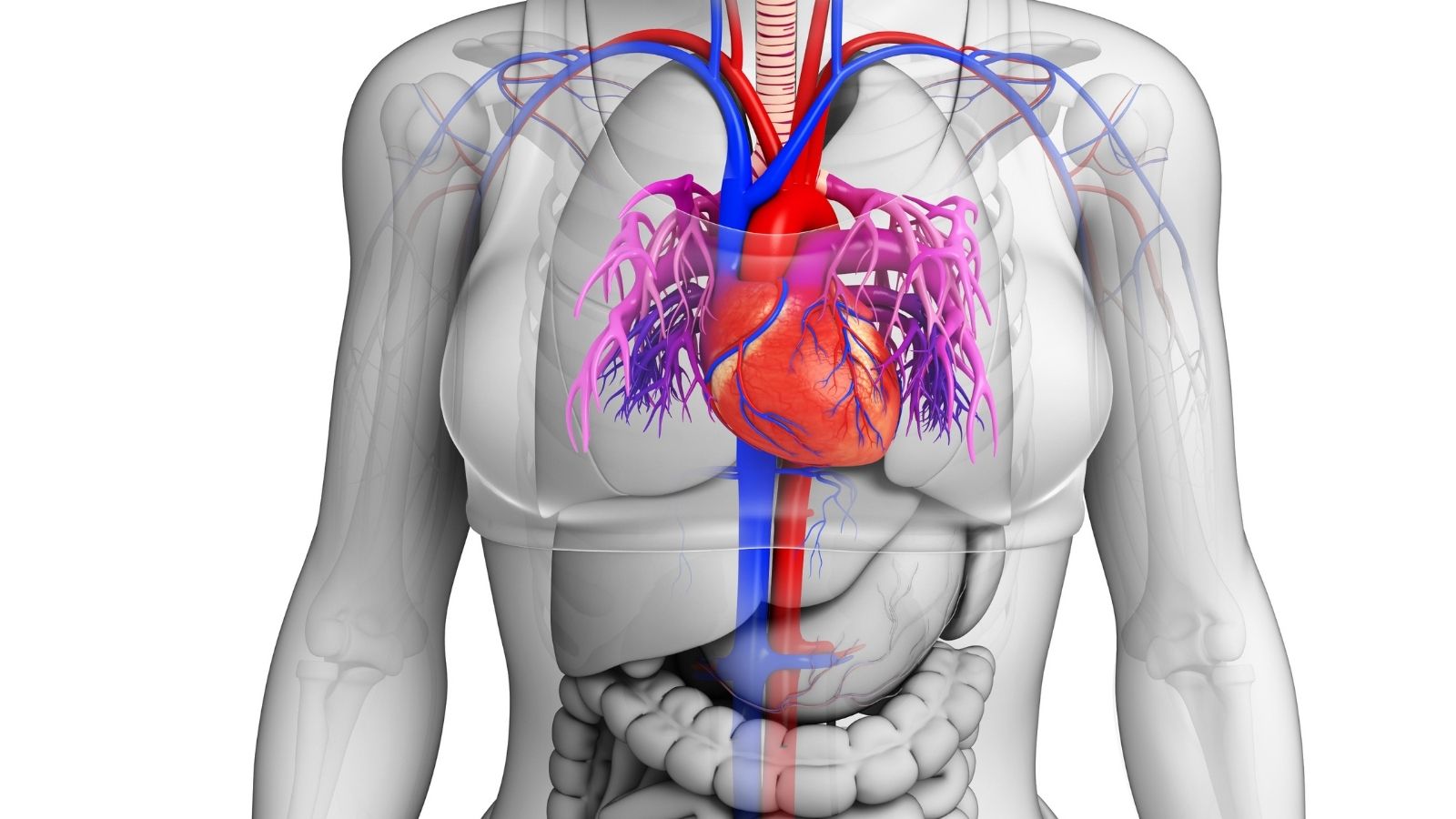
To understand this better, let’s take a look at our blood. There is a protein called “hemoglobin” that gives our blood its red color and whose most important job is to carry fresh oxygen from the lungs throughout our body. Filled with oxygen, hemoglobin is a bright, vibrant red color. This gives our skin that healthy, rosy appearance.
After hemoglobin releases vital oxygen to tissues and organs, its color darkens, becoming dark red-purple. Cyanosis is an optical reflection of the increased amount of this dark hemoglobin that has been deprived of oxygen in the thin capillaries close to our skin. Normally this is not noticeable, but when the oxygen level in the blood drops below a certain threshold (usually below ), this bluish-purple color becomes visible on the skin and mucous membranes. This is a sign that either the lungs are not getting enough oxygen or the heart is not distributing oxygenated blood properly throughout the body.
What are the Most Common Symptoms of Cyanosis?
Cyanosis can present itself in different places and where these symptoms are located gives us important clues about the severity of the underlying problem. The most common symptoms of cyanosis are the following:
- Bluish or purplish discoloration of the lips
- The tongue loses its normal pink color and turns purple
- Prominent bruising in the nail beds
- Coldness and purple color in fingers and toes
- Bruising of the tip of the nose and earlobes
- A general pallor and bluish tint to the skin
Are There Types of Cyanosis and What Is the Difference Between Them?
Yes, we divide cyanosis into two main groups. This distinction is like a roadmap for understanding the source of the problem and is critical for accurate diagnosis.
Central Cyanosis (Central Cyanosis): In this type of cyanosis, the problem is with the blood before it is distributed throughout the body, in the center (heart or lungs). The blood flowing out of the lungs is not sufficiently oxygenated. This is often a sign of a more serious condition. It is most reliably recognized by looking at warm, well-blooded areas, such as the tongue and the inner surface of the lips. If these areas are purple, this indicates central cyanosis.
Peripheral Cyanosis (Environmental Cyanosis): What is peripheral cyanosis? In this condition, there is enough oxygen in the blood pumped from the heart. However, when the blood reaches the extremities of the body (such as the fingers and toes), the blood flow slows down. Because the slower blood stays in the tissues longer, the tissues take up more oxygen than usual and the blood oxygen is depleted. As a result, bruising is seen in that area. With this type of cyanosis, the tongue and lips remain pink, only the extremities turn purple and are usually cold to the touch.
What Causes Bruising on Fingernails?
Bruising of the fingernails or finger bruising is one of the most common complaints and is often an indicator of peripheral cyanosis. So, what causes bruising at the base of the fingernails? There are several common reasons behind this:
The simplest and most harmless cause is cold air. Our body works by an intelligent mechanism to maintain the temperature of the vital organs in the center, and in the cold it constricts the veins in the hands and feet. This slows down blood flow and causes a temporary bruising of the fingers. When it warms up, this situation completely resolves.
However, there may be more serious causes underlying this condition. In a person with heart failure, blood circulation slows down because the heart cannot pump blood through the body strongly enough. This slows down, causing the blood to stagnate, especially at the extremities, and to lose oxygen, causing bruising. Similarly, if there is congestion or narrowing of the arteries in the arms or legs due to atherosclerosis, there is not enough blood supply to the area, which can lead to bruising of the fingers.
Why Is Lip Bruising More Dangerous?
Cyanosis of the lips, especially the tongue, i.e. central cyanosis, is usually a sign of a more urgent and serious condition than peripheral cyanosis. Because this indicates that the problem is not just due to a local circulation problem in the hands or feet, but that the oxygen level of the blood distributed throughout the entire body is low.
This means that there is a fundamental problem in the lungs, where oxygen passes into the blood, or in the heart, where oxygenated blood is pumped into the body. For example, there may be a congenital hole in the heart where dirty blood mixes with clean blood. Or there may be a serious anomaly where large blood vessels exit the heart upside down. In the lungs, life-threatening conditions such as a severe pneumonia or a clot in the lung (pulmonary embolism) can cause central cyanosis. Therefore, if bruising is noticed on a person’s tongue or lips, it should never be ignored and medical attention should be sought immediately.
Is Cyanosis Dangerous? When is it necessary to see a doctor?
The answer to this question depends entirely on the underlying cause. It would not be right to say a clear yes or no to the question of whether cyanosis is dangerous. It is not alarming if your fingers turn slightly purple when they are cold and go away when they warm up. However, there are some cases where cyanosis is a sign of very serious danger and requires emergency intervention.
In the following cases, you should immediately contact a health care provider:
- If the bruising started suddenly
- If accompanied by shortness of breath
- If you have chest pain
- If you experience nausea or fainting
- If the bruising is in central areas such as the tongue and lips
- If detected in a newborn baby
What are the Main Causes of Cyanosis?
The answer to the question of why cyanosis occurs is quite broad. The reasons can be grouped under three main headings.
Heart Causes: The most serious causes of cyanosis are usually related to the cardiovascular system.
- Tetralogy of Fallot
- Transposition of the Great Arteries (TGA)
- Truncus Arteriosus
- Total Abnormal Pulmonary Vein Dilation (TAPVD)
- Eisenmenger Syndrome (due to advanced heart defects)
- Severe heart failure
- Cardiogenic Aok
Lung Causes: Since the lungs are where the blood is oxygenated, serious problems there can lead directly to cyanosis.
- Advanced stages of COPD
- Severe asthma attack
- Heavy pneumonia (pneumonia)
- Pulmonary embolism (clot in the lung)
- Acute respiratory distress syndrome (ARDS)
- Drowning or obstruction of the airway
Other Causes: Sometimes the problem can be outside the heart or lungs.
- Sudden ascent to very high altitudes (mountain sickness)
- Poisoning with certain medicines, chemicals or poisons
- Rare blood disorders such as methemoglobinemia or sulfhemoglobinemia
- No seizure
- Severe hypothermia (dangerous drop in body temperature)
How is Cyanosis Diagnosed Step by Step?
When assessing a patient with cyanosis, we try to put the pieces of the puzzle together to see the big picture. This process consists of a series of diagnostic steps.
First, we take a detailed history of the patient and perform a thorough physical examination. Then we move on to specific diagnostic tests. These tests include:
Pulse Oximeter: With this simple finger-worn device, we instantly measure oxygen saturation in the blood.
Arterial Blood Gas: With a small sample of blood taken from an artery, we can precisely determine the levels of oxygen and carbon dioxide in the blood.
Hyperoxia Test: We make the patient breathe pure oxygen and observe the increase in oxygen levels. This test helps us distinguish whether the problem is in the heart or the lungs.
The chest radiograph: It allows us to assess the size and shape of the heart and the condition of the lungs in general.
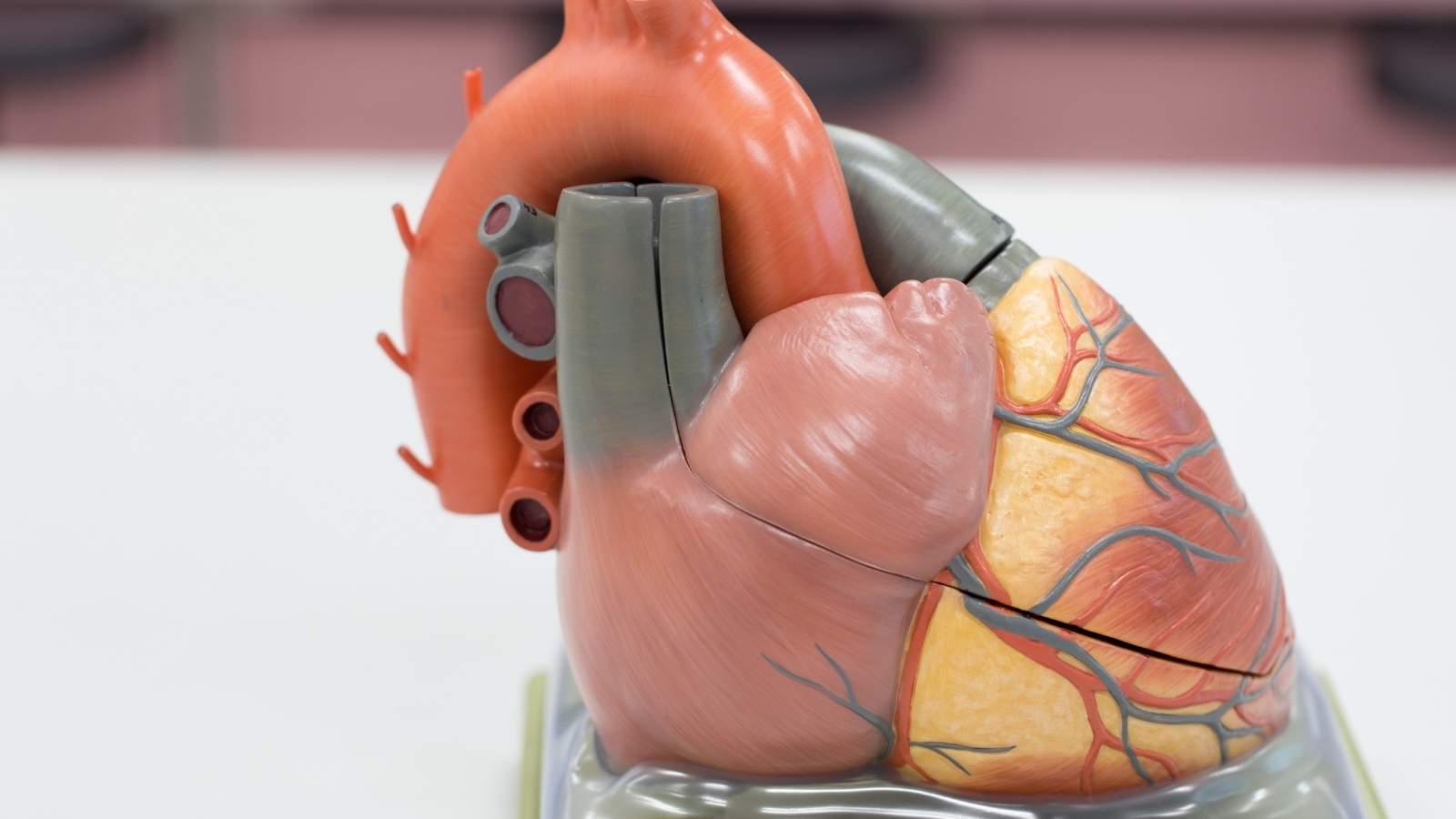
Echocardiography (ECHO): Ultrasound of the heart is the cornerstone of diagnosis. It allows us to see in detail the structure of the heart, its chambers, valves, whether there are holes and the force of contraction.
Cardiac CT and MRI: We use these high-tech methods especially when large vessels (such as the aorta) or complex heart anomalies need to be visualized in three dimensions.
Cardiac Catheterization (Angiography): This method can be both diagnostic and therapeutic. By entering through a vein in the groin or arm, we measure the pressures inside the heart, calculate the pulmonary vascular resistance and take a film of the heart chambers. This data plays a critical role in predicting the risk and success of a particularly major surgery.
How is cyanosis treatment planned?
It is important to remember that treatment for cyanosis is not about applying a cream or swallowing a pill to eliminate bruising. Treatment is entirely directed at the underlying disease causing the cyanosis. As a cardiovascular surgeon, our role is to diagnose and treat heart and vascular diseases that require surgical intervention.
What is the Surgical Treatment of Cyanosis Due to Congenital Heart Disease?
Thanks to modern cardiac surgery, many congenital heart diseases that cause cyanosis can now be successfully treated. The surgical methods used depend on the type and complexity of the disease and the age of the patient.
Temporary (Palliative) Surgeries: Especially in newborn babies, if the lung vessels or heart structures are too small for a complete correction surgery, temporary procedures called “Asant” are performed. These surgeries aim to increase blood flow to the lungs, thereby increasing the baby’s oxygen levels and enabling it to grow safely for the full correction surgery.
Complete Correction Surgeries: When the patient’s condition allows, surgeries are performed to completely correct the anatomical defect in the heart. For example, in Tetralogy of Fallot, the hole in the heart is closed with a patch and the stenosis at the exit of the pulmonary artery is removed. In Transposition of the Great Arteries, an operation called “Arterial Switch” is used to relocate the main arteries draining from the heart and restore normal blood circulation. These operations have dramatically increased the life expectancy and quality of life of patients. However, regular lifelong follow-up of these patients is crucial to detect potential late-stage problems early.
What are the treatments for bruising of the finger due to vascular occlusion?
In so-called “critical limb ischemia”, which develops in the arms or legs due to blocked arteries, the aim is to open the blocked vessel and restore blood flow to the area.
Endovascular (Closed) Methods: It is performed without a surgical incision, like angioplasty, by entering through the groin or arm vein. These methods include the following:
- Balloon angioplasty
- Stent placement
- Atherectomy (intravascular trauma)
Open Surgery (Bypass): For long occlusions where closed methods are not suitable, a new vascular access (bridge) is created to carry blood beyond the occluded area. The most ideal material for this bridging procedure is the saphenous vein, which is taken from the patient’s own leg.
What Are Surgical Options for Cyanosis Due to Advanced Heart Failure?
In patients with end-stage heart failure, where drug therapy is no longer effective, more advanced surgical options are indicated for cyanosis and other severe symptoms caused by a decrease in the heart’s pumping power.
Cardiac Assist Devices (VAD): These devices are mechanical pumps that take over the role of a weakened heart. They can serve as a bridge for patients awaiting a heart transplant, or as a permanent treatment option for patients without the chance of transplant. This technology has advanced the treatment of heart failure.
Heart Transplant: When all other treatment options have failed, heart transplantation is the last resort. This is a life-saving operation in which a diseased heart is replaced with a healthy heart from a brain-dead donor.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.