Pulse refers to the rhythmic expansion of arteries caused by the heartbeat and is an essential indicator of cardiovascular health. The normal resting pulse rate for adults typically ranges between 60–100 beats per minute, depending on age, physical condition, and activity level.
Pulse measurement methods are crucial for identifying cardiovascular disorders. Radial, carotid, and femoral artery palpation are commonly used to assess rhythm, strength, and regularity, providing clinicians with valuable diagnostic insights into circulatory function.
Low pulse rates, medically termed bradycardia, may signal conduction abnormalities, metabolic disorders, or side effects of certain medications. Persistent bradycardia can cause dizziness, fatigue, or fainting, and may require advanced diagnostic evaluation for underlying conditions.
High pulse rates, known as tachycardia, can arise from fever, anemia, thyroid disease, or cardiac arrhythmias. Persistent tachycardia not related to exertion may compromise cardiac efficiency, highlighting the importance of clinical evaluation and timely management.
| Medical Name | Pulse (Pulse, Heart Rate) |
| Common Symptoms | – Acceleration (tachycardia) or slowing (bradycardia)- Irregular pulse (arrhythmia)- Fatigue- Dizziness- Palpitations |
| Causes | – Exercise or physical activity- Excitement, stress, fear- Fever, infection- Heart diseases- Thyroid diseases- Medications |
| Risk Factors | – Hypertension- Cardiovascular diseases- Anemia- Thyroid disorders- Electrolyte imbalances |
| Complications | – Fainting with low or high pulse rate- Insufficient blood supply to organs- Heart failure- Arrhythmia |
| Diagnostic Methods | – Pulse counting (manual or electronic devices)- Electrocardiography (ECG)- Holter monitoring |
| Treatment Methods | – Treatment of the underlying cause – Sedatives or heart rhythm regulators (if necessary) – Regular exercise – Healthy lifestyle |
| Prevention Methods | – Regular exercise- Healthy diet- Stress management- Reducing caffeine and smoking |
What is the pulse and how is it measured?
The pulse, in its simplest definition, is the palpable fluctuation in the vessel walls caused by the blood pumped into the arteries by the heart with each contraction. It is not just a number; it is a dynamic indicator that reflects the rhythm and strength of your heart and the overall flexibility of your vascular system.
It is quite easy to measure the pulse and you do not need a special instrument. The most common and easiest to feel is on the inside of the wrist, just below the thumb. The radial artery that runs through here is ideal for measuring the pulse. You can follow a few simple steps to take an accurate measurement. First, sit in a comfortable place and rest for a few minutes to allow your body to calm down. Then gently press the tips of your index and middle finger on the inside of the wrist of the other hand, at the level of the thumb. It is important that you do not use your thumb here, as its own strong pulse can falsify the measurement. When you feel the rhythmic beats in the vein, you can start counting. If your pulse is regular, you can easily calculate the number of beats per minute by counting for 15 seconds and multiplying the number by 4. However, if you feel an irregularity in your pulse, a misfire or excessive acceleration, you should always count for a full minute to get the most accurate result.
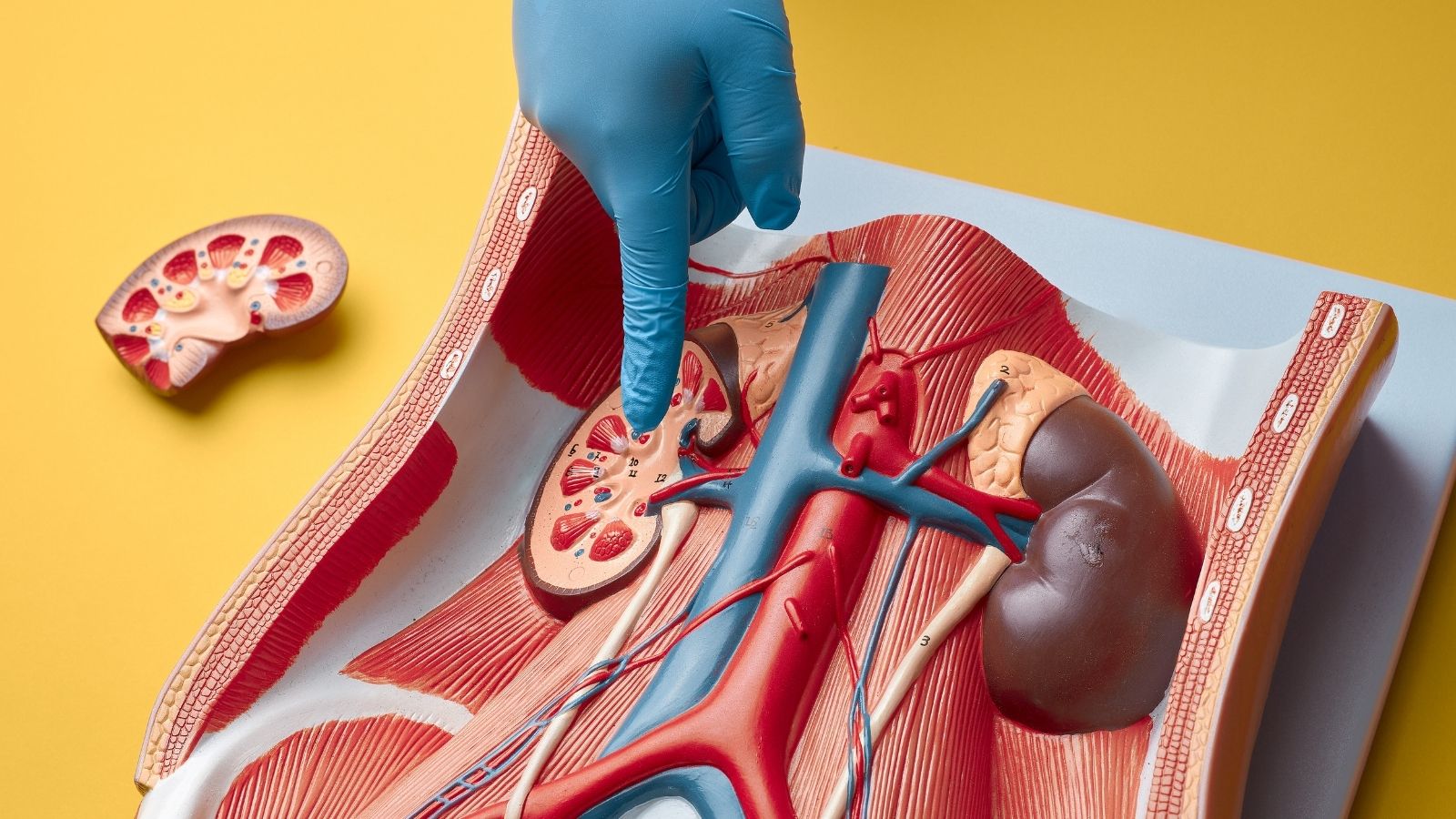
Apart from your wrist, there are other important points where you can feel your pulse. During an examination, a doctor will check these different points to assess whether your blood circulation is reaching all parts of the body in a healthy way.
These points are:
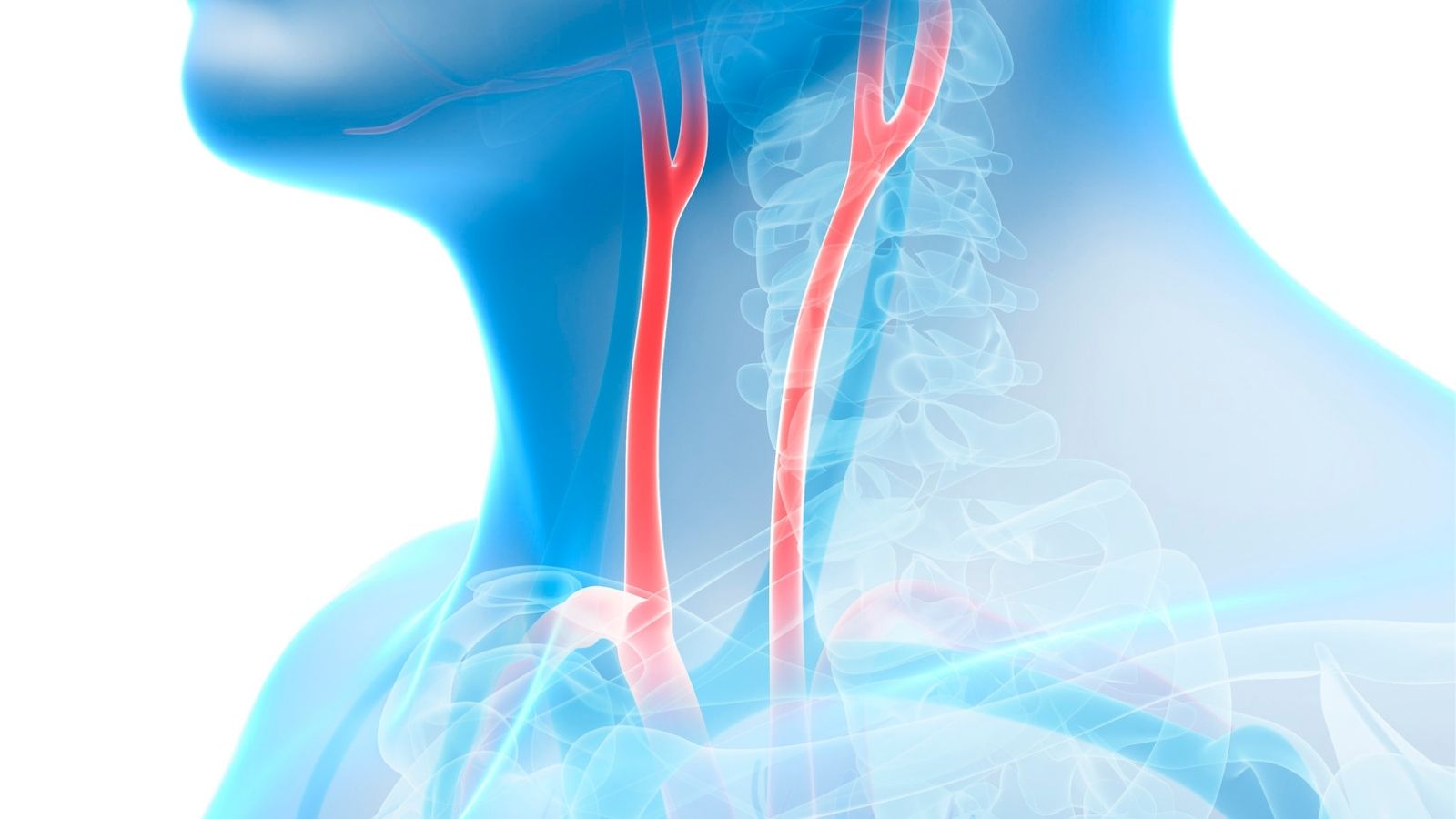
- Carotid artery (Carotid)
- Arm vein (Brachial)
- Inguinal vein (Femoral)
- Vein behind the knee (Popliteal)
- Back of the ankle (Posterior tibial)
- Back of the foot (Dorsalis pedis)
For example, a strong pulse in the groin area but a very weak or absent pulse on the back of the foot is an important clue that there may be a problem with the blood vessels supplying the lower parts of the leg. A pulse examination is therefore not only about finding out the heart rate, but also about mapping the vascular system:
What is the difference between heart rate and pulse rate?
Although these two terms are often used interchangeably in everyday life, medically there is a subtle but important difference. Understanding this difference can be critical in interpreting some health issues. Heart rate is the electrical activity of the heart. It shows how often the sinoatrial node, a natural battery inside the heart, “fires”, that is, how often it sends the heart the command to contract. This is most accurately measured by ECG (electrocardiogram).
The pulse rate is a mechanical phenomenon that occurs as a result of this electrical impulse. It is the frequency with which the pressure wave created by the blood pumped into the arteries with each effective contraction of the heart is felt in the blood vessels. In a healthy person, each electrical impulse of the heart causes an effective contraction and therefore a palpable pulse wave. This is why heart rate and pulse rate are usually the same.
But sometimes there can be a mismatch between the two. Your heart may appear to be beating 100 times a minute on the ECG, while you can only count 80 pulses on your wrist. This is called a pulse deficit (pulse deficit). This means that some of the beats in the heart are so weak that it cannot pump blood effectively around the periphery and create a palpable pressure wave in the blood vessels. This is a classic symptom of arrhythmias, in which the heart works too fast and irregularly and therefore cannot fill with enough blood for each beat. One of the most common examples is atrial fibrillation. Such a finding is a direct indication that the heart is working inefficiently and requires an ECG to investigate the underlying cause.
What should be the heart rate by age?
There is no one magic number that is considered “normal” for the pulse rate. The ideal pulse rate varies significantly at different stages of life. Our heart is a dynamic organ that adapts to the changing needs of the body and this is reflected in the pulse rate.
The pulse rate, which is highest at birth, gradually slows down throughout childhood and stabilizes within a certain range in adulthood. Normal pulse ranges at rest according to age are generally as follows.
Newborn (0-1 month): 70-190
Infant (1-11 months): 80-160
Child (1-2 years): 80-130
Child (3-4 years): 80-120
Child (5-9 years): 70-115
children 10 years and older and adults: 60-100
For adults, a resting pulse rate between 60 and 100 beats per minute is generally considered normal. However, even values within this range can have different meanings. For example, a resting pulse rate near the lower end of the range, such as 60-70, is often seen as a sign of good cardiovascular fitness and an efficiently functioning heart. In contrast, a resting pulse rate that is consistently near the upper limits of 80-100, although considered “normal”, may be a risk factor for future cardiovascular disease.
So, what should be the blood pressure and pulse rate over the age of 65? or what should be the blood pressure and pulse rate at the age of 70? For a healthy individual in advanced ages, the resting pulse rate is expected to be in the range of 60-100. However, since additional diseases such as high blood pressure and diabetes are more common in this age group, regular monitoring of both blood pressure and pulse rate and keeping them within the targets set by the physician becomes even more important. If you are wondering what the pulse rate should be on the blood pressure monitor you use at home, the pulse rate measured by these devices should be interpreted according to the same 60-100 range.
A special group to keep in mind is athletes. In endurance athletes who train regularly and intensively, it is quite common for the resting pulse to be between 40-60 as the heart adapts to work more efficiently, a healthy condition called “athletic bradycardia”.
What is the pulse rate considered dangerous?
The rate is not the only factor that determines whether the pulse is dangerous. The symptoms accompanying the change in pulse rate and the underlying cause of this change determine the severity of the condition.
High Pulse (Tachycardia)
When an adult’s pulse rate is consistently over 100 per minute at rest, this is called tachycardia. It is a completely normal body reaction for your pulse rate to rise temporarily when you run, get excited or have a fever. However, if your pulse rate is consistently high at rest for no apparent reason, this may indicate a problem.
Here are some conditions that may underlie a persistently high pulse:
- Anemia (Anemia)
- Dehydration of the body (dehydration)
- Overactive thyroid gland (hyperthyroidism)
- A clot in the lung (pulmonary embolism)
- Heart failure
- Febrile illnesses and infections
- Rhythm disorders such as atrial fibrillation
- Excessive consumption of caffeine, alcohol or stimulants
- Intense stress and anxiety
There is no single answer to the frequently asked question of what is the pulse rate in a heart attack. During a heart attack, the pulse usually quickens as the body responds to stress. However, if the attack is in an area that affects the heart’s conduction system, the pulse can become dangerously slow or completely irregular. Therefore, any sudden and abnormal changes in the pulse rate accompanied by symptoms such as chest pain should be taken seriously.
Low Pulse (Bradycardia)
When the pulse rate is consistently below 60 beats per minute at rest, this is called bradycardia. Whether this condition is dangerous or not depends on the person and the accompanying symptoms. As mentioned above, while a pulse of 50 is healthy for an athlete, the same value for a sedentary older person could be a sign that the body is not getting enough blood.
A low pulse is considered pathological, i.e. due to a disease, if it is accompanied by the following symptoms
- Dizziness
- Excessive and persistent fatigue
- Confusion or forgetfulness
- Shortness of breath
- Blackouts, fainting sensation or fainting (syncope)
These symptoms indicate that the heart is unable to pump enough blood to carry the oxygen and nutrients the body needs. The underlying causes of pathological bradycardia may include disturbances in the heart’s own electrical system (sick sinus syndrome, AV blocks), underactive thyroid gland (hypothyroidism) or certain heart and blood pressure medications.
So, how low does the pulse rate drop and death occurs? There is no clear numerical answer to this question. The danger to life occurs when the heart stops pumping blood efficiently (cardiac arrest) rather than when the pulse rate falls below a certain number. However, severe bradycardia that causes symptoms and is left untreated can set the stage for this dangerous condition.
What problems can an irregular pulse indicate?
Not only the rate of the pulse, but also the rhythm of the pulse can provide important information about heart health. If you notice an irregular pulse, it should be evaluated by a physician and confirmed with an ECG. There are two main types of disorder:
Irregularly Irregular: This is a completely chaotic rhythm with no logical order or pattern between the pulse beats. It is almost like an irregular drum beat. This is the most characteristic sign of atrial fibrillation (AFib). In atrial fibrillation, the atria of the heart vibrate chaotically instead of contracting in an organized way. This causes the ventricles to contract irregularly and often rapidly. Because the time between each contraction is different, the heart cannot fill with enough blood and the amount of blood pumped varies with each beat. You feel this in your wrist as strong and weak, completely irregular beats. The biggest danger of atrial fibrillation is that it can lead to the formation of clots inside the heart, seriously increasing the risk of stroke. Therefore, its diagnosis and treatment is vital.
Regularly Irregular: In this case, there is a repeating pattern within the irregularity. For example, one premature beat after every two normal beats. This may indicate premature beats (extrasystole), often originating from different foci of the heart, or certain types of block in the heart’s electrical conduction system (e.g. second-degree AV block).
Does the character of the pulse give a clue about a disease?
For an experienced physician, a pulse examination is a kind of stethoscope with the fingertips. Not only the number or rhythm of the pulse wave is assessed, but also its “character” – how strong it is, how quickly it rises and disappears. This is best assessed in large arteries close to the heart, such as the carotid artery. The specific patterns of the pulse wave are a signature for certain structural cardiovascular diseases.
Important pulse characteristics and the conditions they may be associated with are as follows:
Slow Rising and Weak Pulse (Pulsus Parvus et Tardus): Aortic Valve Stenosis
Leaping, Pounding Pulse (Hyperkinetic Pulse): Aortic Valve Failure
Double Peaked Pulse (Pulsus Bisferens): Coexistence of Aortic Stenosis and Insufficiency or HOCM (a Special Heart Muscle Disease)
One Strong and One Weak Pulse (Pulsus Alternans): Severe Left Heart Failure
Pulse weakened by breathing (Pulsus Paradoxus): Cardiac Tamponade (accumulation of fluid in the pericardium) or Serious Lung Diseases
Rapid and Filamentous Pulse: Shock Conditions (Blood Loss, Serious Infection)
What does a weak or absent pulse mean?
A weak or absent pulse, especially in the legs or feet, is usually the most important sign that there is a problem with the blood flow to that area. The most common cause behind this condition is Peripheral Arterial Disease (PAD). This disease is a narrowing or blockage of the arteries outside the heart, especially in the legs, usually due to atherosclerosis (arteriosclerosis).
Risk factors for Peripheral Arterial Disease are:
- Smoking (the most important risk factor)
- Diabetes (diabetes)
- High blood pressure (hypertension)
- High cholesterol (hyperlipidemia)
- Advanced age
The typical symptom of this disease is cramping pain in the legs that occurs when exertion is required, such as walking. This pain goes away with rest. As the disease progresses, pain may occur even at rest and the feet may develop wounds that do not heal.
When a weak pulse is detected, a simple but invaluable test is performed to confirm the diagnosis and determine the severity of the disease: Ankle-Brachial Index (ABI) or Ankle-Arm Index. In this test, a Doppler device is used to measure the blood pressure in both the arms and the ankles, and then compare them to each other. This ratio objectively shows how much blood flow in the legs is reduced. An ABI value below 0.90 is diagnostic for Peripheral Arterial Disease.
After the diagnosis is made, imaging methods such as Doppler ultrasonography and CT angiography are used to see the location and extent of the blockage. Treatment is aimed at opening the blocked vessel. This can be accomplished with balloon/stent procedures using angiography-like methods or bypass surgery, which aims to create a new vascular access around the blockage.
Is a palpable pulse in the abdomen a danger sign?
It can be normal, especially in thin people, to feel the pulsation of the aorta, the body’s main artery, in the abdomen. However, if this pulse is felt as a palpable, enlarged mass that feels like a ball, it may be a sign of an abdominal aortic aneurysm (AAA) that requires urgent medical evaluation.
An aneurysm is a weakening and abnormal expansion of the artery wall into a balloon. An aneurysm is when the diameter of the abdominal aorta exceeds 3 cm. These aneurysms usually grow silently without any symptoms and their greatest danger is that they burst (rupture), causing life-threatening internal bleeding. A ruptured aneurysm can present with the triad of sudden and severe abdominal or back pain, low blood pressure and a mass in the abdomen.
Ultrasonography is the most commonly used method for diagnosing and monitoring AAA. It is both harmless and extremely sensitive. The treatment decision is based entirely on the diameter and growth rate of the aneurysm. Intervention is usually required when the diameter reaches 5.0-5.5 cm or when it shows rapid growth.
Today, there are two main methods for treating AAA:
Endovascular Aneurysm Repair (EVAR): It is the insertion of a fabric-covered stent into the aneurysm with the help of a catheter through small incisions made in the groin. This stent covers the aneurysm from the inside, protecting it from blood pressure and eliminating the risk of rupture. It is less invasive and the healing process is faster.
Open Surgical Repair: This is a procedure in which an incision is made in the abdomen and the aneurysm is removed and replaced with an artificial vessel (graft). Although it is a larger operation, in some cases it may offer a more permanent solution.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.