Thoracic outlet syndrome is a condition caused by compression of nerves or blood vessels between the collarbone and first rib. It can result in pain, numbness, and circulation problems in the arms and shoulders, significantly affecting daily activities.
Neurological thoracic outlet syndrome is the most common type, presenting with tingling, weakness, and loss of function in the upper extremities. Vascular forms can cause swelling, color changes, or blood clots in the affected arm.
Diagnosis of thoracic outlet syndrome involves physical examination, imaging methods, and nerve conduction studies. Identifying the underlying cause of compression is crucial to determining the correct treatment strategy.
Treatment options include physiotherapy, postural correction, pain management, and in resistant cases, surgical decompression. Early intervention improves quality of life and prevents long-term complications associated with vascular or neurological damage.
| Medical Name | Thoracic Outlet Syndrome (TOS, Thoracic Outlet Syndrome) |
| Common Symptoms | – Pain in the shoulder, arm and hand – numbness and tingling in the arm or hand – arm weakness – discoloration or coldness of the fingers |
| Causes | – Cervical ribs (cervical costa)- Muscle, ligament or bone abnormalities- Trauma or repetitive forceful movements- Overdevelopment of muscles |
| Risk Factors | – Repetitive arm and shoulder movements- Excessive use of the shoulder in athletes- Neck or shoulder trauma- Genetic predisposition |
| Complications | – Permanent nerve damage – Vascular congestion or clot formation – Muscle wasting |
| Diagnostic Methods | – Physical examination – Magnetic resonance imaging (MRI) – Electrophysiological tests (EMG) – Vascular ultrasound and CT/MR angiography |
| Treatment Methods | – Physiotherapy and exercise- Painkillers and muscle relaxants- Surgical intervention if necessary |
| Prevention Methods | – Ergonomic posture and work – Regular exercise and muscle strengthening – Avoiding overload |
What is thoracic outlet syndrome and why does it happen?
Thoracic Outlet Syndrome, in its simplest terms, is an anatomical narrowing problem. It is the narrowing of the thoracic outlet, which is a natural corridor designed by our body for the nerves and vessels going to the arm, due to various reasons, resulting in compression of these structures.
We can liken this situation to a highway intersection with heavy traffic. Under normal conditions, traffic flows smoothly. However, if there is a road narrowing or an obstacle at this intersection, traffic gets stuck and vehicles cannot move forward. The thoracic outlet is such a junction for nerves and vessels going to the arm. An abnormality in the bone, muscle or connective tissue in this area narrows this “junction” and disrupts the “traffic” of nerves and vessels. The collection of symptoms that arise as a result of this compression is called Thoracic Outlet Syndrome. It is more common in young and active people, usually between 20 and 50 years of age.
Where is the “thoracic outlet” in our body?
The thoracic outlet is an anatomically narrow passage between the bridge bone (clavicle), first rib and neck muscles. This strategic corridor extends from the lower part of the neck to the armpit and is of vital importance because of the structures that pass through it. Structures that pass through this narrow space and are at risk of entrapment are:
- Brachial Plexus (a large nerve network)
- Subclavian Artery (Main artery)
- Subclavian Vein (Main vein)
Together these three structures are called the “neurovascular bundle”. The fact that the thoracic outlet is surrounded by hard bones (the bridge bone, the first rib) and flexible soft tissues (muscles, ligaments) makes the area an inherently vulnerable point to compression. Even the slightest anatomical change or postural disturbance can upset this delicate balance.
Why do nerves and vessels get stuck in this narrow space?
This compression can be likened to a “pinching” effect. The bundle of nerves and vessels is crushed between two hard structures or between a muscle and bone. The root causes are usually a combination of one or several factors. There are three potential narrow spaces where the squeeze occurs:
- Scalene (between the neck muscles and the first rib)
- Costoclavicular space (between the bridge bone and the first rib)
- Pectoralis Minor Gap (under the buttock muscle)
The reasons behind the narrowing of these areas vary from person to person. Sometimes a congenital predisposition, such as an extra rib (cervical rib), predisposes to this narrowing. Sometimes a trauma, bad posture habits or repetitive arm movements, such as in certain professions, disrupt the balance in this area over time, triggering a pinch.
What are the main types of Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome comes in three fundamentally different forms, depending on which structure is compressed. This classification plays a critical role in determining the direction of treatment because the symptoms and urgency of each type are different. These are the main types:
- Neutrogenic TOS (nTOS)
- Venose TOS (vTOS)
- Arterial TOS (aTOS)
Sometimes venous and arterial types are grouped together as “Vascular TOS”.
What is the most common Neurogenic TOS and what are the symptoms?
Neurogenic TOS (nTOS) is the most common type, accounting for -95% of all cases. In this type, the brachial plexus, the nerve supply to the arm, is compressed. It is more common in women between the ages of 20 and 50.
diagnosing nTOS can be one of the most challenging processes for patients. This is because, despite patients’ severe symptoms, nerve measurement tests such as EMGs can often be completely normal. This is referred to as “controversial nTOS” and can lead to patients not understanding their pain. Therefore, the diagnosis of nTOS is made on the basis of the patient’s history and a thorough physical examination, after ruling out all other possibilities that could lead to similar symptoms.
Typical symptoms of thoracic outlet syndrome (for the neurogenic type) include the following:
- Dull or sharp pain radiating to the neck, shoulder and arm
- Numbness and tingling in the inner side of the forearm and the 4th and 5th fingers
- Weakness in the hand and arm, difficulty grasping
- Clumsiness such as dropping things
- In advanced cases, melting of the muscle at the base of the thumb (Gilliatt-Sumner hand)
- Headaches radiating to the back of the head with neck pain
How to recognize venous TOS and why is it important?
Venous TOS (vTOS) is a rarer condition that occurs when a vein (subclavian vein) is compressed and requires immediate attention. It is more common in young, active men who usually play heavy sports or work in jobs that require repetitive arm movements.
Under constant pressure, the vein is damaged and a clot (thrombosis) can form in it. This condition is also known in medicine as Paget-Schroetter syndrome or “exertional thrombosis”. Symptoms are often very sudden and dramatic:
- Sudden and marked weakness in the entire arm, hand and fingers
- A bluish or purplish discoloration of the arm (cyanosis)
- Deep, aching pain and a feeling of heaviness in the arm
- Prominent superficial veins on the shoulder and chest
These symptoms are a sign that blood circulation in the arm is severely impaired and require urgent medical attention.
Does arterial TOS make thoracic outlet syndrome dangerous?
This is one of the most critical questions, especially for patients with the possibility of vascular compression, and the answer is unfortunately yes when it comes to Arterial Thoracic Outlet Syndrome (aTOS). aTOS is the rarest but also the most urgent and potentially most dangerous form of the syndrome.
This can be likened to pressing on a garden hose. In aTOS, an extra neck rib (cervical rib) or an abnormal muscle band, usually congenital, presses on the main artery (subclavian artery) that carries clean blood to the arm. This constant pressure and rubbing damages the vessel wall. Over time, this damage can lead to serious problems. These problems include the following:
- Vascular wall weakening and ballooning (aneurysm)
- Clot formation in a blood vessel (thrombosis)
This is where the real danger begins. The clots that form in the blood vessel can break off and be carried by the blood flow to the extremities of the arm, up to the fingers. This is called an “embolism” and can suddenly block the blood vessels to the fingers. Cutting off the blood supply can lead to tissue death, i.e. gangrene. Therefore, aTOS is a condition that requires urgent surgical intervention and should never be ignored.
What are the main risk factors and causes for TOS?
The development of TOS is usually not due to a single cause. It is often the result of a combination of an underlying anatomical predisposition and a triggering factor. The main causes and risk factors can be divided into three main groups.
Inborn (Congenital) Factors:
- Cervical rib (an extra neck rib)
- Deformity of the first rib or collar bone
- Abnormal fibrous bands (hard connective tissues)
- Abnormal attachment sites of the scalene muscles
Traumatic Factors:
- Whiplash injury after a traffic accident
- Fractures of the bridge bone
- First rib fractures
- Direct blows to the shoulder
Functional/Adaptive Factors:
- Repetitive overhead movements (swimmers, volleyball players, painters)
- Poor posture in which the shoulders are lowered forward (posture disorder)
- Excessive growth of the neck and shoulder muscles with bodybuilding (hypertrophy)
- Carrying a heavy backpack or shoulder bag
- Obesity
- Pregnancy
How is Thoracic Outlet Syndrome diagnosed?
The diagnosis of Thoracic Outlet Syndrome, especially for the most common form, nTOS, requires detective work. As there is no single definitive diagnostic test, it is considered a “diagnosis of exclusion”. In other words, the diagnosis is reached by eliminating all other more common and known conditions that can cause similar symptoms (cervical hernia, carpal tunnel syndrome, shoulder joint problems, etc.).
This process requires patience and experience. The most important steps in diagnosis are the following:
- Listening to the patient’s story in great detail
- Perform a thorough physical examination
- Eliciting symptoms with provocative tests
- Use of visualization methods deemed necessary
In this journey, especially for nTOS patients with normal test results despite their symptoms, consulting a specialist who understands the condition and is experienced in TOS makes a big difference.
What are the diagnostic tests for thoracic outlet syndrome?
During the physical examination, some specific maneuvers are used to elicit the patient’s symptoms by temporarily increasing the compression at the thoracic outlet. These provocative tests help to confirm the presence and location of the obstruction.
The most commonly used tests for thoracic outlet syndrome include the following:
- Adson Test
- Roos Test (Elevated Arm Stress Test – EAST)
- Wright Test
- Costoclavicular (Eden) Test
For example, in the Roos Test, the patient is asked to raise their arms in the “surrender” position with the arms bent at 90 degrees and slowly open and close their hands for 3 minutes. The appearance of pain, numbness, powerlessness or a feeling of heaviness in the arm during this time is a significant finding for TOS. It should be remembered that these tests alone are not diagnostic and should always be interpreted in conjunction with the patient’s general complaints and other findings.
What role do imaging methods play in diagnosis?
Imaging methods are used to confirm the diagnosis, determine the exact location and cause of the compression, and plan a possible surgery. Generally, a path from simple to complex is followed.
X-ray (X-ray): It is the first step to detect bone abnormalities such as cervical ribs or old fractures.
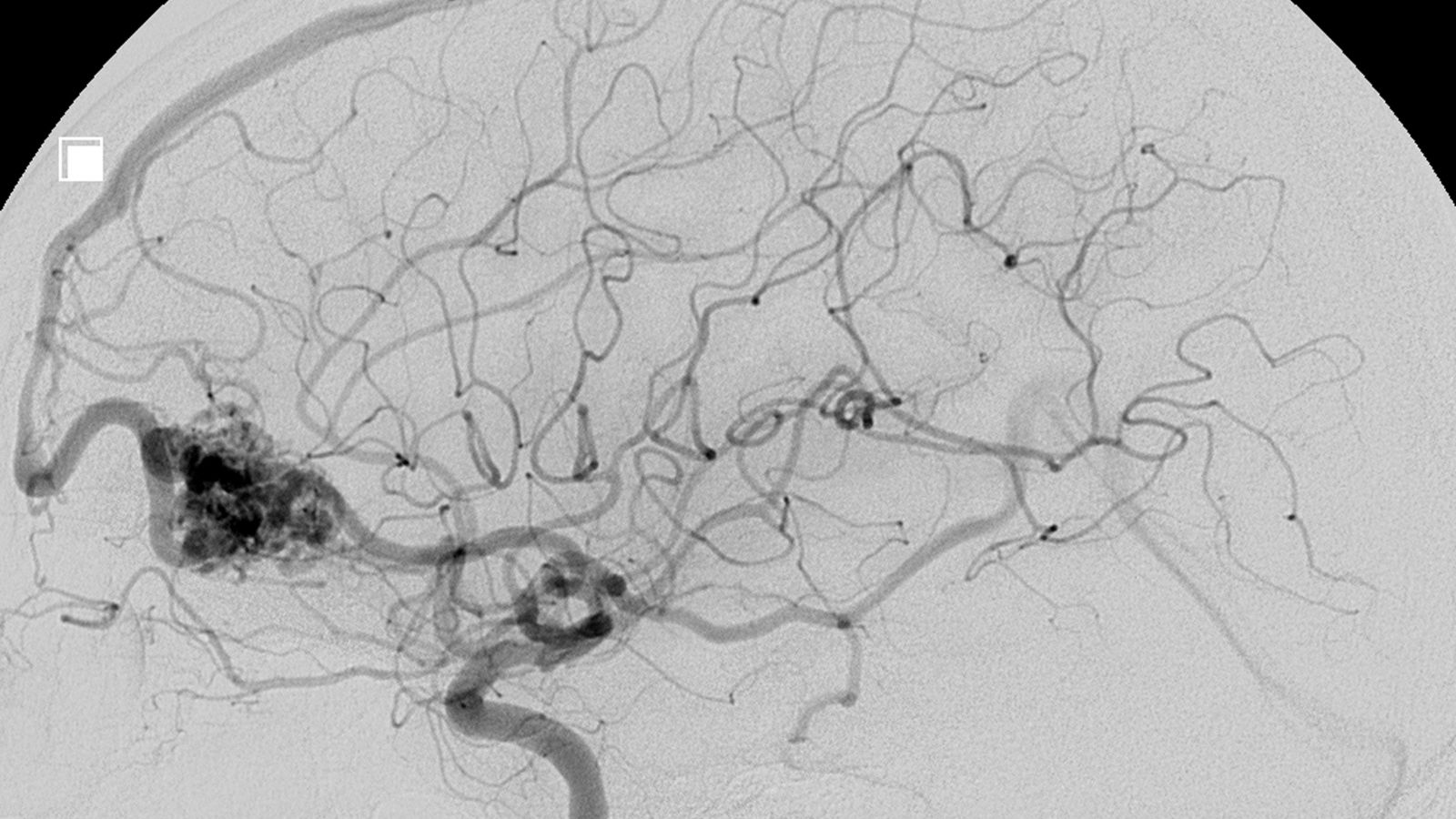
Doppler Ultrasound: A harmless and very effective test used to dynamically (during arm movements) assess the flow in blood vessels and possible compression, especially in the case of vascular TOS.
Computed Tomography (CT) / CT Angiography: Shows bone structures and vessels in detail in three dimensions. It is very valuable in surgical planning.
Magnetic Resonance (MR) / MR Angiography: The most advanced method for imaging soft tissues such as nerves, muscles and ligaments. It can show a direct visualization of the nerve network (brachial plexus) and whether it is compressed by a muscle or fibrous band.
When do you need further tests such as EMG or angiography?
These further examinations come into play when the diagnosis cannot be confirmed or when more details are needed for surgical planning.
Electromyography (EMG): Measures the speed at which nerves transmit signals. it is used to objectively prove nerve damage in suspicion of “true” nTOS or to rule out other nerve compressions such as carpal tunnel. However, in the most common “controversial” form of nTOS, the results are usually normal. A normal EMG does not rule out the diagnosis of TOS.
Catheter Angiography/Venography: Interventional procedures considered the “gold standard” for demonstrating vascular obstruction or stenosis. It is usually performed when the diagnosis of vascular TOS is strong, both to confirm the diagnosis and to perform treatment (such as clot dissolution, balloon dilation) in the same session.
Scalene Blockade: an important diagnostic test for nTOS. A local anesthetic is injected into the scalene muscle thought to be causing the tightness. If the patient’s symptoms gradually improve, this is considered a strong sign that they will benefit from surgical treatment.
How is thoracic outlet syndrome treatment planned?
Treatment of thoracic outlet syndrome is completely individualized, depending on the type of syndrome, the severity of symptoms and the underlying cause. The general approach is almost always to start treatment for the most common type, Neurogenic TOS, with conservative (non-surgical) methods. A significant proportion of patients show significant improvement with these methods. In vascular (venous and arterial) types, treatment is usually surgically oriented, as the situation is more urgent and there is an underlying structural problem.
Does thoracic outlet syndrome improve with physical therapy?
Yes, the cornerstone of management of neurogenic TOS is the thoracic outlet syndrome physical therapy program. This is not a passive “wait and see” approach, but an active and structured treatment process. The main goal of physical therapy is to mechanically expand the space in the thoracic outlet region. The goals for this are the following:
- Stretching tense muscles that contribute to compression (scalenes, chest muscles)
- Strengthen weak muscles that support posture (especially those around the pelvis)
- Gaining correct posture habits to the patient
- To allow the nerves to move more easily in the surrounding tissues (nerve sliding)
- Reducing overuse of the accessory respiratory muscles with proper breathing techniques
- Conservative treatment is usually tried for at least 3-6 months before surgery is considered for nTOS.
What are effective thoracic outlet syndrome exercises?
As part of the physical therapy program, thoracic outlet syndrome exercises, which are individually prescribed by a physiotherapist, are the most important part of the treatment. These exercises should be repeated regularly at home. The most commonly recommended types of exercise are:
- Doorway or corner stretching exercises (for the muscles of the chest)
- Scalene muscle stretching exercises (for the side muscles of the neck)
- Chin tuck (pushing the head back) exercise (for posture)
- Scapular squeeze exercises (for the back muscles)
- Rowing exercises (for strengthening the back muscles)
- Nerve gliding/flossing exercises
- Diaphragmatic (abdominal) breathing exercises
How do lifestyle changes and medicines help in treatment?
In addition to physical therapy, some simple but effective changes in daily life and medical treatments can help control symptoms.
Lifestyle and Ergonomic Arrangements:
- Avoid carrying heavy bags or backpacks on the shoulder
- Limiting the overhead activities that trigger symptoms
- Ergonomic organization of the office environment (monitor height, chair adjustment)
- Adjusting the sleeping position (so as not to put pressure on the arm)
- Losing weight in overweight individuals
- Taking regular breaks at work and doing stretching exercises
Drugs and Injections:
- Anti-inflammatory drugs for pain and inflammation (NSAIDs)
- Muscle relaxants for muscle spasms
- Special medicines for nerve pain (such as Gabapentin)
- Local anesthetic or Botox injections into the scalene muscles (temporarily relaxes the muscles, reducing pressure on the nerve and allowing physical therapy)
When is thoracic outlet syndrome surgery necessary?
The decision to operate for thoracic outlet syndrome differs from blind to the type of syndrome.
For Vascular TOS (Venous and Arterial): Surgery is almost always and often urgently necessary. Conditions such as clots, aneurysms or severe vascular stenosis necessitate surgery to prevent life-threatening complications such as gangrene or clots in the lungs (pulmonary embolism).
For neurogenic TOS: Surgery is considered a last resort. However, surgery becomes an option if, despite a structured conservative treatment program (physical therapy, injections, lifestyle changes) for at least 3-6 months, the patient continues to have severe and persistent symptoms that are severe enough to interfere with daily life or work.
What is the purpose of TOS surgery and what procedures are performed?
The main purpose of the surgery is to permanently enlarge the thoracic outlet area by removing the anatomical structures causing the compression and completely freeing the nerve/vascular bundle. This procedure is called “thoracic outlet decompression”. The most common procedures during surgery are as follows:
- First rib resection (removal of the first rib, which forms the basis of the compression)
- Cervical rib resection (removal of extra neck ribs, if present)
- Scalenectomy (Cutting or removal of the scalene muscles that cause compression)
- Neurolysis (removal of all adhesions and scar tissues around the nerve artery)
What is the special role of the Cardiovascular Surgeon in the treatment of vascular TOS?
The management of Vascular (Venous and Arterial) TOS falls squarely within the specialty of a Cardiovascular Surgeon. In these cases, our role is not limited to decompression by simply removing bone or muscle. A comprehensive vascular management is required. This governance includes:
Interventional Treatments: To perform pre-operative procedures, usually through a catheter, that dissolve the clot (thrombolysis) or balloon the stenosis (angioplasty).
Vessel Repair: Repairing a vessel that has been damaged by pressure during decompression surgery. This may involve patching with a piece of vessel (patch angioplasty) or removing the damaged section completely and creating a new pathway with an artificial vessel (graft) (bypass).
This requires a combination of both open decompression surgery and advanced vascular surgery techniques and is the specialty of Cardiovascular Surgery.
How does the recovery process work after surgery?
Postoperative recovery depends on the extent of the surgery performed, but the general expectations are as follows:
- The hospital stay is usually 1 to 3 days.
- For the first few weeks, medication is required for pain control.
- Return to light activities and desk work is usually possible within 2 to 4 weeks.
- Heavy lifting and strenuous arm movements should be avoided for 2-3 months.
Physical therapy is a critical part of recovery. It usually starts a few weeks after surgery and continues for several months to prevent scar tissue formation, restore mobility and strengthen the muscles.
What should people who experience thoracic outlet syndrome after treatment expect?
Post-treatment expectations depend on the type of syndrome and the treatment used.
Vascular TOS With timely and accurate surgical intervention, the prognosis is generally excellent. With blood flow restored, success rates are very high and the risk of recurrence is low.
Neurogenic TOS: Outcomes are more variable. The vast majority (-90%) of patients who undergo surgery experience good or excellent relief of their symptoms. However, because the nerves are under pressure for long periods of time, persistent symptoms such as some mild numbness may occur. a “good outcome” is usually defined as a functional improvement that greatly reduces the patient’s pain and allows him or her to return to work and daily life.
Conservative Treatment: Among those with thoracic outlet syndrome, approximately P-70 of those diagnosed with nTOS improve significantly with physical therapy and lifestyle changes alone and do not require surgery.
When should you consult a Cardiovascular Surgeon?
Consulting the right specialist at the right time is the most important step for a successful outcome.
Conditions Requiring Emergency Referral (Suspicion of Vascular TOS):
- Sudden onset of light and bruising in the arm
- Marked pallor and paleness of the arm and hand
- Weak or absent pulse in the affected arm
- Wounds on fingers that do not heal
If any of these symptoms are present, an emergency room or a Cardiovascular Surgeon should be consulted immediately.
Conditions Requiring a Planned Referral (Neurogenic TOS):
- If you have been diagnosed with neutrogenic TOS
- If you have not responded to at least 3-6 months of regular and supervised conservative treatment (physical therapy, etc.)
- If your complaints continue to seriously impair your quality of life
In this situation, it is appropriate to consult a Cardiovascular Surgeon experienced in TOS to discuss surgical options and the next step in the treatment plan. Expertise and a multidisciplinary approach to the management of this complex syndrome is the key to achieving the best outcome.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.